Orofacial Pain in Low- and Middle-Income Settings
Authors:
- Fernando Hormazábal, DDS: Hospital Clínico Dr. Félix Bulnes, Hospital Clínico Mutual de Seguridad CChC. Corporación Sintesys. Santiago, Chile
- Leonardo Lavanderos, PhD: Corporación Sintesys. Santiago, Chile
- Nicolás Skarmeta, DDS: Hospital del Salvador. Santiago, Chile
- Paula Espinoza, DDS: Hospital San Juan de Dios. Santiago, Chile
Impact of Orofacial Pain Conditions on the Global Population
Orofacial pain significantly impacts health and daily life by affecting fundamental activities such as eating, speaking, sleeping, and working. This widespread disruption leads to diminished quality of life, increased use of healthcare services, and greater workplace absenteeism, creating considerable economic and social burden.
The emotional consequences are particularly devastating, especially when acute pain leads to tooth loss. Economic barriers and limited access to appropriate care ultimately trap lower-income populations in a cycle where extraction becomes the only option, resulting in irreversible loss of masticatory function rather than tooth preservation. An estimated 3.5 billion people worldwide are affected by oral diseases [1], making these among the most prevalent global health problems, with disproportionate burden in low- and middle-income settings.
This cycle reflects broader healthcare accessibility challenges, where socioeconomic factors significantly influence access to appropriate pain management and preventive care, ultimately determining whether individuals can maintain their oral health and masticatory function or develop prevalent orofacial pain conditions. In most low- and middle-income country (LMIC) healthcare systems, attention to orofacial pain focuses primarily on dentoalveolar conditions requiring extraction or basic treatment. However, this narrow focus leaves a vast spectrum of non-dentoalveolar chronic orofacial pain conditions virtually invisible and untreated.
Furthermore, this constant exposure to episodes of acute pain and inflammation of odontogenic origin not only causes immediate suffering, but also acts as a powerful driver of peripheral and central sensitization, creating fertile ground for the transition to chronic orofacial pain even after the initial cause (such as a dental infection) has been resolved. While dentoalveolar pain receives some attention in LMIC healthcare systems (though often inadequate), other orofacial pain conditions such as musculoskeletal, neuropathic, neurovascular pain, and other orofacial pain syndromes represent common sources of chronic pain, contributing to significantly greater economic burden through increased healthcare costs and out-of-pocket expenses, lost productivity, and early retirement. These conditions disproportionately burden LMICs, where research, education, healthcare systems, access to orofacial pain specialists, and management of orofacial pain remain severely inadequate.
Opportunity for Orofacial Pain Care in Low- and Middle-Income Countries
Low- and middle-income countries face substantial challenges in delivering specialized orofacial pain care. Although international organizations have developed rapid and reliable diagnostic tools, fundamental barriers hinder their effective implementation in these settings. The primary barriers include: (i) absence of translations into local languages, and (ii) limited representation in international knowledge exchange within the orofacial pain field [2].
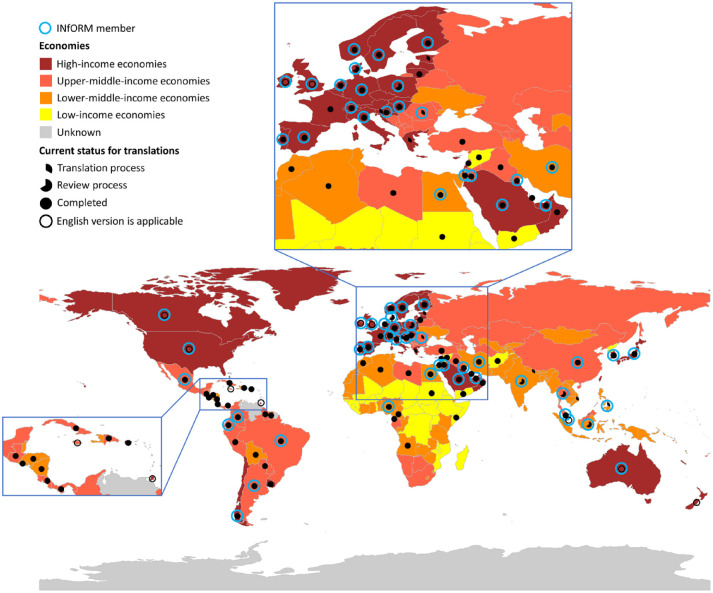
Figure 1. Global map shows the world’s countries by economy: low, lower-middle, upper-middle, and high income. The full and partial black dots and black circles represent the availability of local versions of the DC/TMD (Diagnostic Criteria for Temporomandibular Disorders): full black dots represent finalized translated and culturally adapted local versions; partial dots, local versions that are currently being translated or reviewed; and black circles, countries where the source version (English language) can be applied. The blue circles indicate countries with ≥1 members of INfORM (International Network for Orofacial Pain and Related Disorders Methodology). Clearly, the lower the income level, the less likely that a local version of DC/TMD is available. From [2].
Cultural Context, Educational Gaps, and Social Health in Orofacial Pain
The limited global recognition of orofacial pain burden, combined with gaps in specialist training, diagnosis, and treatment in LMICs, reflects the structural determinants of inequality in dental care access. Within this context, orofacial pain remains particularly neglected, characterized by disconnection between health systems, local culture, medical education, and dominant global medical frameworks.
To address these challenges, a promising and viable solution may be a meta-epistemic relational approach—that is, examining how different knowledge systems (Western medical frameworks and local cultural beliefs about pain and healing) can interact and work together to create more comprehensive solutions. Through this approach, we can develop a systemic vision that addresses the important need for educational, research, and dissemination efforts fostering broader collaboration grounded in local cultural contexts.
This includes developing local knowledge to maximize relevance and applicability of diagnostic tools in LMICs, while thoughtfully adapting global frameworks like the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) [3] to local contexts. By ensuring local accessibility and cultural validation of these instruments, we can enhance their effectiveness. This epistemological reorientation will strengthen community-adapted strategies for improving education and social health access in these contexts.
Building on this foundation, we suggest advocating for a tridifferential perspective—analyzing problems simultaneously from clinical, cultural, and economic angles. This approach could help identify areas of tension (triferences)—the different priorities among these three viewpoints—while enabling collaborative solutions based on ecopoietic logic: creating solutions that emerge naturally from local environments and cultures in partnership with established frameworks [4,5].
A Roadmap for Action: Proposals for Orofacial Pain Integration
The 74th World Health Assembly resolution [6] emphasized the important need to improve oral health and access to orofacial pain care, creating an opportunity to build upon existing efforts. Our proposed approach offers a complementary pathway through cultural resonance in educational and clinical practice, enabling the co-production of relational diagnostic tools—developing diagnostic instruments together with patients, communities, and health professionals in collaborative partnerships.
This collaborative approach prioritizes cultural sustainability alongside technical efficiency—recognizing that diagnostic tools achieve optimal effectiveness when they are culturally relevant and contextually appropriate for local healthcare settings. Such tools should integrate accessible technologies validated through participatory methodologies that involve local healthcare professionals and communities, ensuring they address real clinical needs in LMICs while building on existing global knowledge and expertise.
To translate this resolution into tangible results, we propose a collaborative roadmap based on three pillars:
- Transdisciplinary EducationDevelop joint educational modules for pain specialists from different health professions focusing on differential diagnosis and management of dentoalveolar/non-dentoalveolar orofacial pain and the principles of chronic pain diagnosis and management.
- Applied ResearchFoster multinational research lines, supported by IASP, that focus on validating low-cost diagnostic tools for dentoalveolar/non-dentoalveolar orofacial pain conditions and identifying risk factors for pain chronification following common dental and craniofacial surgical procedures.
- Policy and AdvocacyWork collaboratively to ensure that national clinical guidelines and public policies on chronic pain explicitly include comprehensive orofacial pain management, ensuring coverage and funding.
REFERENCES
- Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño CC, Kearns C, et al. 2019. Oral diseases: a global public health challenge. Lancet. 394(10194):249–260. https://doi.org/10.1016/s0140-6736(19)31146-8
- Lobbezoo F, Aarab G, Kapos FP, Dayo AF, Huang Z, Koutris M, Peres MA, Thymi M, Häggman-Henrikson B. The Global Need for Easy and Valid Assessment Tools for Orofacial Pain. J Dent Res. 2022 Dec;101(13):1549-1553. https://doi.org/10.1177/00220345221110443
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo F, Michelotti A, Brooks SL, Ceusters W, Drangsholt M, Ettlin D, Gaul C, Goldberg LJ, Haythornthwaite JA, Hollender L, Jensen R, John MT, De Laat A, de Leeuw R, Maixner W, van der Meulen M, Murray GM, Nixdorf DR, Palla S, Petersson A, Pionchon P, Smith B, Visscher CM, Zakrzewska J, Dworkin SF; International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014 Winter;28(1):6-27. https://doi.org/10.11607/jop.1151
- Hormazabal F, Lavanderos L, Malpartida A. Biocybernetic model for the diagnosis and treatment of chronic pain: An approximation from cognitive neurosciences and the theory of complexity. Kybernetes 2020;50(2):369-385. http://dx.doi.org/10.1108/K-07-2019-0469
- Lavanderos L, Malpartida A. Life as a relational unit, the process of ecopoiesis. Kybernetes 2024;53(12):5047-5060. https://doi.org/10.1108/K-05-2023-0859
- World Health Organization. Oral health. Seventy-Fourth World Health Assembly Resolution WHA74.5, Agenda Item 13.2: Oral Health. 31 May 2021. Available at: https://apps.who.int/gb/ebwha/pdf_files/WHA74/A74_R5-en.pdf. Accessed 8 August 2025.


