Advancing Understanding and Action on the Social Determinants of Health for People with Pain
Authors:
- Emma L. Karran, PhD: University of South Australia, Kaurna Land, Adelaide, Australia
- Ursula I. Wesselmann, MD, PhD, DTM&H (Lond.): Department of Anesthesiology and Perioperative Medicine, Division of Pain Medicine, University of Alabama at Birmingham, Birmingham, Alabama, United States
- Chinonso N. Igwesi-Chidobe, PhD: University of Bradford, United Kingdom and University of Nigeria, Nigeria
- Flavia P. Kapos, DDS, MS, PhD: Duke University, Durham, North Carolina, United States
Introduction
The term social determinants of health (SDoH) refers to the conditions in which people are born, grow, live, work, and age, and the fundamental drivers of these conditions: the distribution of power, money, and resources. [14] In this fact sheet we discuss the relevance of the SDoH to the pain field. We explain their relationship to health equity; highlight the need for multi-level, intersectoral strategies to address them, and describe the ways in which the pain community can take action to address avoidable disparities in pain outcomes.
The Social Determinants of Health are a Major Contributor to Health Inequities.
Stark inequalities in health exist within and between countries, with health outcomes closely aligned with levels of disadvantage (and advantage). Higher levels of socio-economic deprivation are associated with worsening health outcomes – such that a social gradient exists between communities that are most and least deprived. [15] This gradient reflects differences in people’s opportunities to live healthy lives, shaped by a wide range of social, economic, and environmental conditions. These conditions – i.e., the SDoH – include the conditions in which people live and work, their access to healthcare and education, food security, and income stability. When these factors are distributed unequally and unjustly, they give rise to avoidable inequities in health. Unequal exposure to adverse social, economic, and environmental conditions occurs systematically – with associated health inequities arising from and maintained by structures, policies, politics, and systems that give rise to the unequal distribution of power, income, education, and resources.
Health equity, conversely, is attained when “everyone has a fair and just opportunity to be as healthy as possible.” [3] Health equity could be the result of social and economic policies that aim to improve the lives of populations across the social gradient, with investment given in proportion to need. The health care sector has an important role to play in addressing the burden of illness. However, action on the SDoH also requires attention to the structural conditions in which people are born, grow, live, work, and age – at interpersonal, community, and societal levels as well as on a global scale.
How do the Social Determinants of Health Relate to Pain?
It is well recognized that the broader circumstances of peoples’ lives are as relevant to pain-related experiences and outcomes as they are to other health conditions that are unequally distributed in society. [5; 8; 9] Numerous studies globally have found that lower incomes, lower education status, and higher neighbourhood deprivation are associated with poorer pain outcomes. Race (and racism), ethnicity, age, sex, gender, occupational factors, and religious involvement have also been shown to impact the burden, impact, and risk of pain. [1; 11] Relatedly, many of these factors have been recognized to play a role in individuals’ healthcare experiences. Disparities in healthcare have been identified between groups characterized by socioeconomic position, race, ethnicity, and other socially stratifiable factors – notably in relation to opioid prescriptions, recommendations for surgery, and access to healthcare providers . As examples: minoritized racial and ethnic groups in the United States have been found to be less likely to receive opioids for the treatment of their chronic pain; [16] and people who do not identify according to a binary classification of gender (i.e., man or woman) may encounter under-informed health care providers and experience discrimination in the healthcare setting as well as in the broader societal context. [2] More broadly, the SDoH may impact health service accessibility and affordability, healthcare quality, and care pathways – differentially impacting people’s opportunities to recover from pain conditions in ways that are avoidable and unfair.
A review of the relationships between socioeconomic position and pain proposed that individual-level socio-economic factors (e.g., income level, education status, occupational position) and structural-level factors (e.g., neighbourhood deprivation and environmental conditions) interacted with psychosocial, biological, and behavioral factors to determine pain experiences. [10] A recent study based on data from 1.3 million people across 146 countries over 10 years aimed to examine the connection between national unemployment rates and reported pain levels found that a 3% increase in a population’s unemployment rate was linked to a 1% average increase in the number of people reporting physical pain. The analysis further found that outcome was largely driven by women: when unemployment increased, pain levels increased mostly among women rather than men. [12]
Complex inter-relationships with personal characteristics such as gender, race, and ethnicity were also acknowledged to be relevant. The multitude of ways in which various personal characteristics interact with power, oppression, and privilege to produce health inequities is depicted by the theoretical framework of intersectionality. [13] This framework acknowledges that the complex interactions of a combination of characteristics may compound privilege or discrimination – leading to better (or worse) health outcomes than if an individual had just one of the characteristics. It is important to recognize that there is wide global variation in social structures and hierarchies – aspects of identity that are meaningful in some cultures (sex, gender, race, ethnicity, sexual orientation, disability, and socioeconomic and cultural factors), may be less relevant in others. Context-specific explorations of intersectionality and its impacts on health opportunities and outcomes are likely to be a necessary component of developing effective policies and action to address health inequities and reduce the burden of pain for all. [4]
The SDoH Have Multi-Level Consequences for People with Pain and Need Multi-Level Strategies to Address Them
The SDoH impact the pain-related experiences of people living with pain, including their opportunities for pain prevention and management – thereby contributing to the unequal distribution of pain across populations. The consequences of multi-level determinants of pain and their interaction with systems of inequity (e.g., racism, sexism, classism, ableism, ageism, heterosexism, and gender binarism) may accumulate over the life course and potentially contribute to intergenerational transmission of pain and its consequences. [6] A recent review of research of social disparities in pain over the last 50 years identified high-priority areas for future research, including greater attention to lower-income countries, chronic pain prevention, and macro-level drivers of pain disparities. [4] Action to address the SDoH and health inequities requires collaboration across multiple sectors of society – including healthcare, education, social services, justice, employment, housing, and transport – to develop strategies to address the broad range of factors that impact health and well-being. Effective strategies to address health inequities require supportive government policies and political will.
The Pain Community Can Take Action to Address Health Inequities
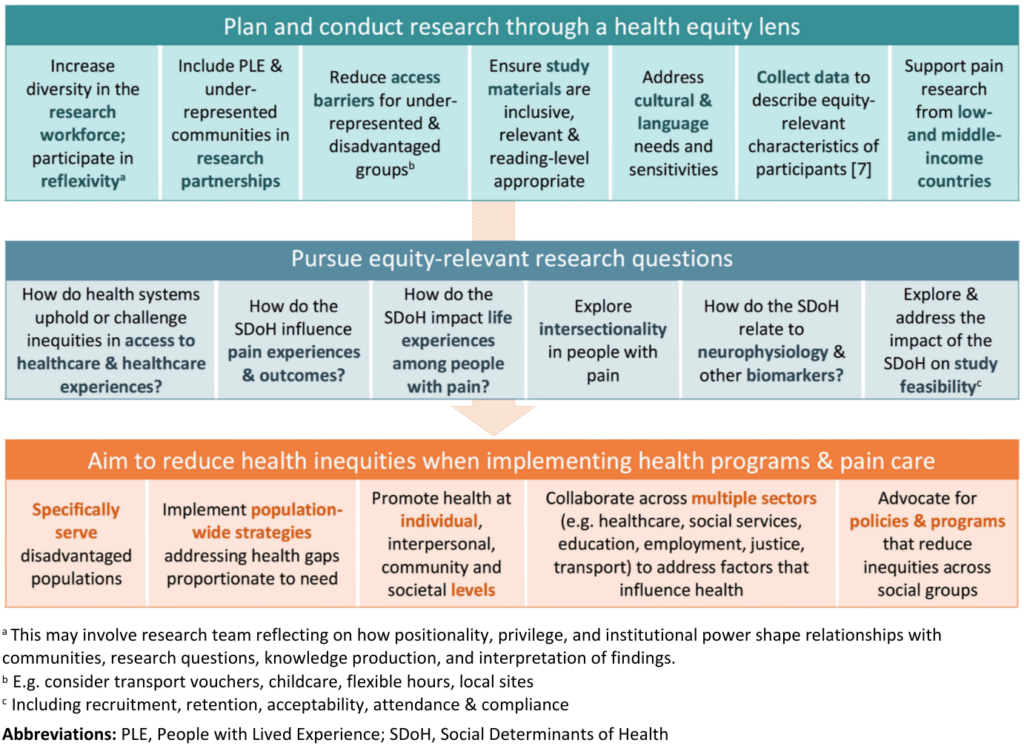
There are a multitude of ways in which the pain community can strategize to address avoidable disparities in pain and health outcomes. Examples of research practices, care considerations, and multi-sectoral collaboration to advance progress towards greater understanding and action on health inequities are outlined in Figure 1.
Figure 1. Suggestions to Drive Understanding and Action on Health Inequities in the Pain Field
Conclusion
Greater attention to the SDoH as major contributors to health inequities is fundamentally important to reduce the global burden of persistent pain. Adopting an “equity lens” to pain research and care is a crucial step towards advancing health for all people with pain.
References
- Atwoli L, Platt JM, Basu A, Williams DR, Stein DJ, Koenen KC. Associations between lifetime potentially traumatic events and chronic physical conditions in the South African Stress and Health Survey: a cross-sectional study. BMC psychiatry 2016;16:1-10. https://doi.org/10.1186/s12888-016-0929-z
- Boring BL, Mathur VA. Gender Discrimination is Associated with Greater Chronic Pain Interference Among Women. J Pain 2025;31:105376. https://doi.org/10.1016/j.jpain.2025.105376
- Braveman P, Arkin E, Orleans T, Proctor D, Acker J, Plough A. What is health equity? Behavioural Science & Policy 2018;4(1):1-14. https://doi.org/10.1177/237946151800400102
- Grol-Prokopczyk H, Huang R, Yu C, Chen Y-A, Kaur S, Limani M, Lin T-H, Zajacova A, Zimmer Z, Cowan P, Fillingim RB, Gewandter JS, Gilron I, Hirsh AT, Macfarlane G, Meghani SH, Patel KV, Poleshuck EL, Strain EC, Symons FJ, Wesselmann U, Dworkin RH, Turk DC. Over Fifty Years of Research on Social Disparities in Pain and Pain Treatment. Pain 2025 Jun 4. Epub ahead of print. https://doi.org/10.1097/j.pain.0000000000003676
- Institute of Medicine (US) Committee on Advancing Pain Research Care, and Education. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press, 2011. https://doi.org/10.17226/13172
- Kapos FP, Craig KD, Anderson SR, Bernardes SF, Hirsh AT, Karos K, Keogh E, Losin EAR, McParland JL, Moore DJ. Social determinants and consequences of pain: Towards multilevel, intersectional, and life course perspectives. J Pain 2024;25(10):104608. https://doi.org/10.1016/j.jpain.2024.104608
- Karran EL, Cashin AG, Barker T, Boyd MA, Chiarotto A, Maxwell LJ, Mohabir V, Sharma S, Tugwell P, Moseley GL. Developing consensus on the most important equity-relevant items to include in pain research: a modified e-Delphi study. Pain 2025 Apr 16. Epub ahead of print. https://doi.org/10.1097/j.pain.0000000000003621
- Karran EL, Cashin AG, Barker T, Boyd MA, Chiarotto A, Mohabir V, Petkovic J, Sharma S, Tugwell P, Moseley GL. It is time to take a broader equity lens to highlight health inequalities in people with pain. Br J of Anaesth 2025;134(1):235-237. https://doi.org/10.1016/j.bja.2024.09.026
- Karran EL, Grant AR, Moseley GL. Low back pain and the social determinants of health: a systematic review and narrative synthesis. Pain 2020;161(11):2476-2493. https://doi.org/10.1097/j.pain.0000000000001944
- Khalatbari-Soltani S, Blyth FM. Socioeconomic position and pain: a topical review. Pain 2022;163(10):1855-1861. https://doi.org/10.1097/j.pain.0000000000002634
- Lea CR, Oliver RJP, Smothers Z, Boucher NA, Youssef NA, Ames D, Volk F, Teng EJ, Koenig HG. The moderating effect of religious involvement on the relationship between PTSD symptoms and physical pain in US veterans and active duty military. Military Behavioral Health 2019;7(3):327-335. https://doi.org/10.1080/21635781.2018.1526149
- Macchia L. Research: the link between recessions and physical pain. Harvard Business Review, 1 March 2022. Available at: https://hbr.org/2022/03/research-the-link-between-recessions-and-physical-pain. Accessed 4 June 2025.
- Macgregor C, Walumbe J, Tulle E, Seenan C, Blane DN. Intersectionality as a theoretical framework for researching health inequities in chronic pain. Br J of Pain 2023;17(5):479-490. https://doi.org/10.1177/20494637231188583
- Marmot M, Bell R. Fair society, healthy lives. Public Health 2012;126:S4-S10. https://doi.org/10.1016/j.puhe.2012.05.014
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Health CoSDo. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008;372(9650):1661-1669. https://doi.org/10.1016/s0140-6736(08)61690-6
- Morales ME, Yong RJ. Racial and ethnic disparities in the treatment of chronic pain. Pain Med 2021;22(1):75-90. https://doi.org/10.1093/pm/pnaa427


