Introduction
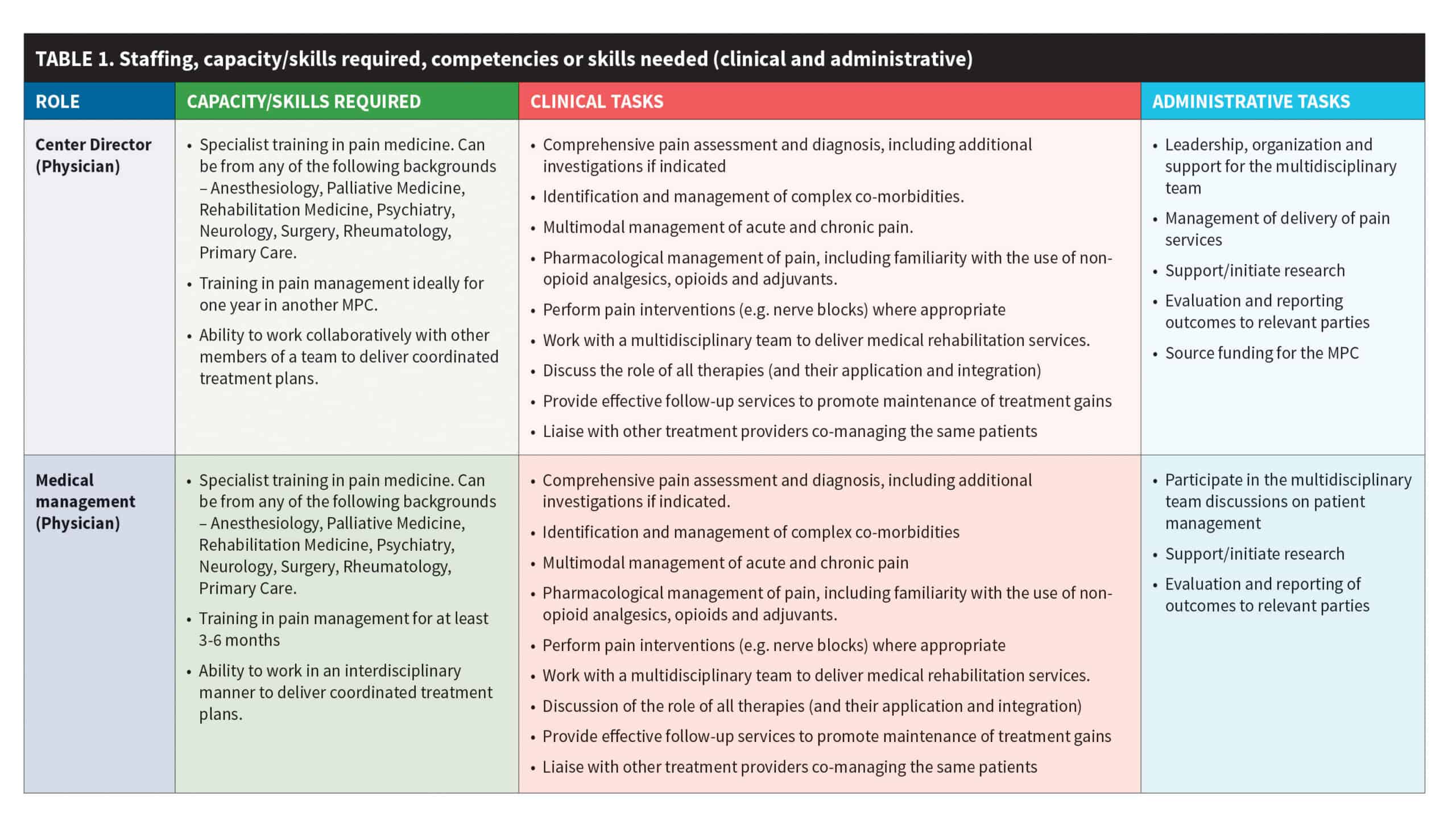
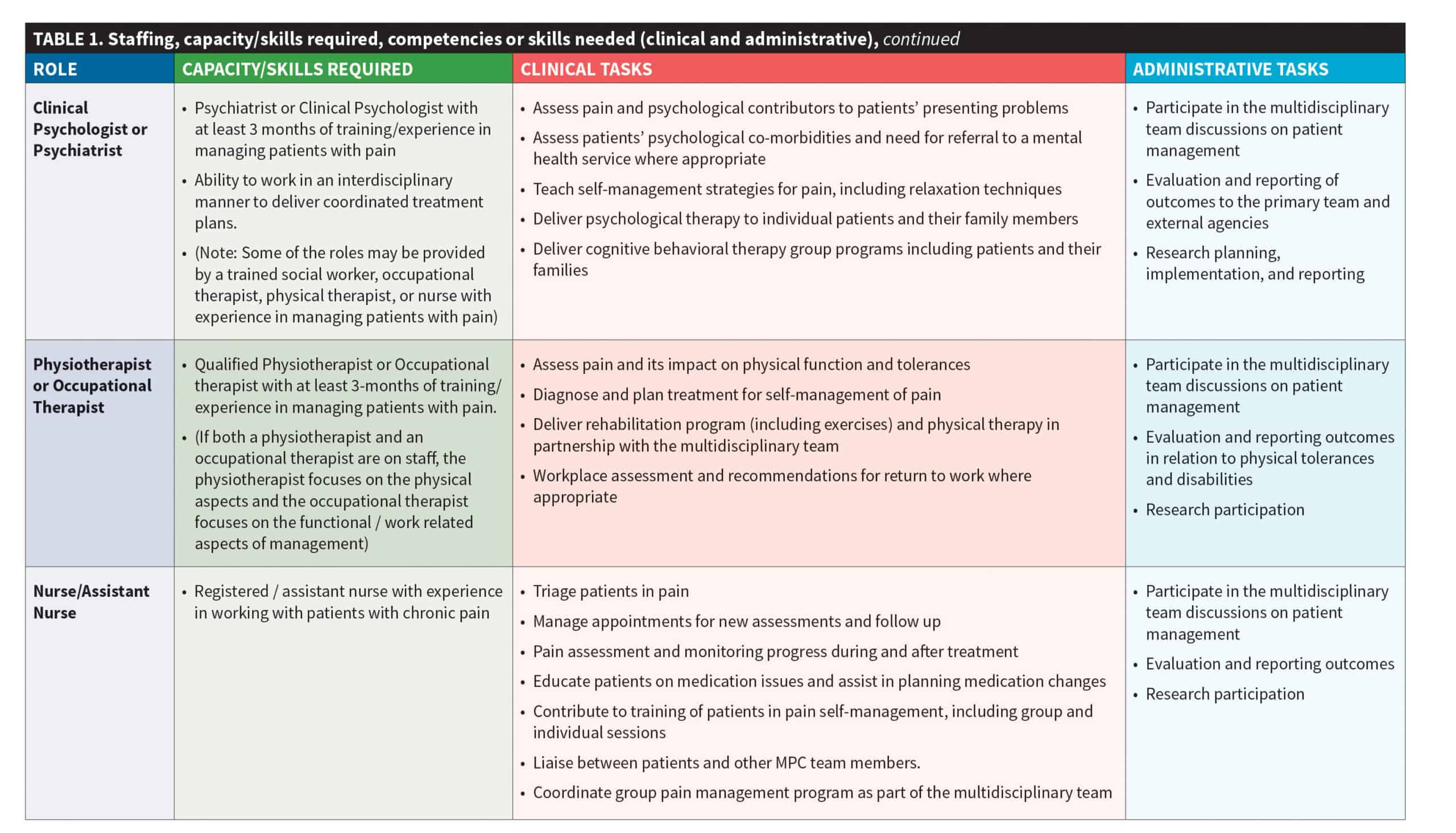
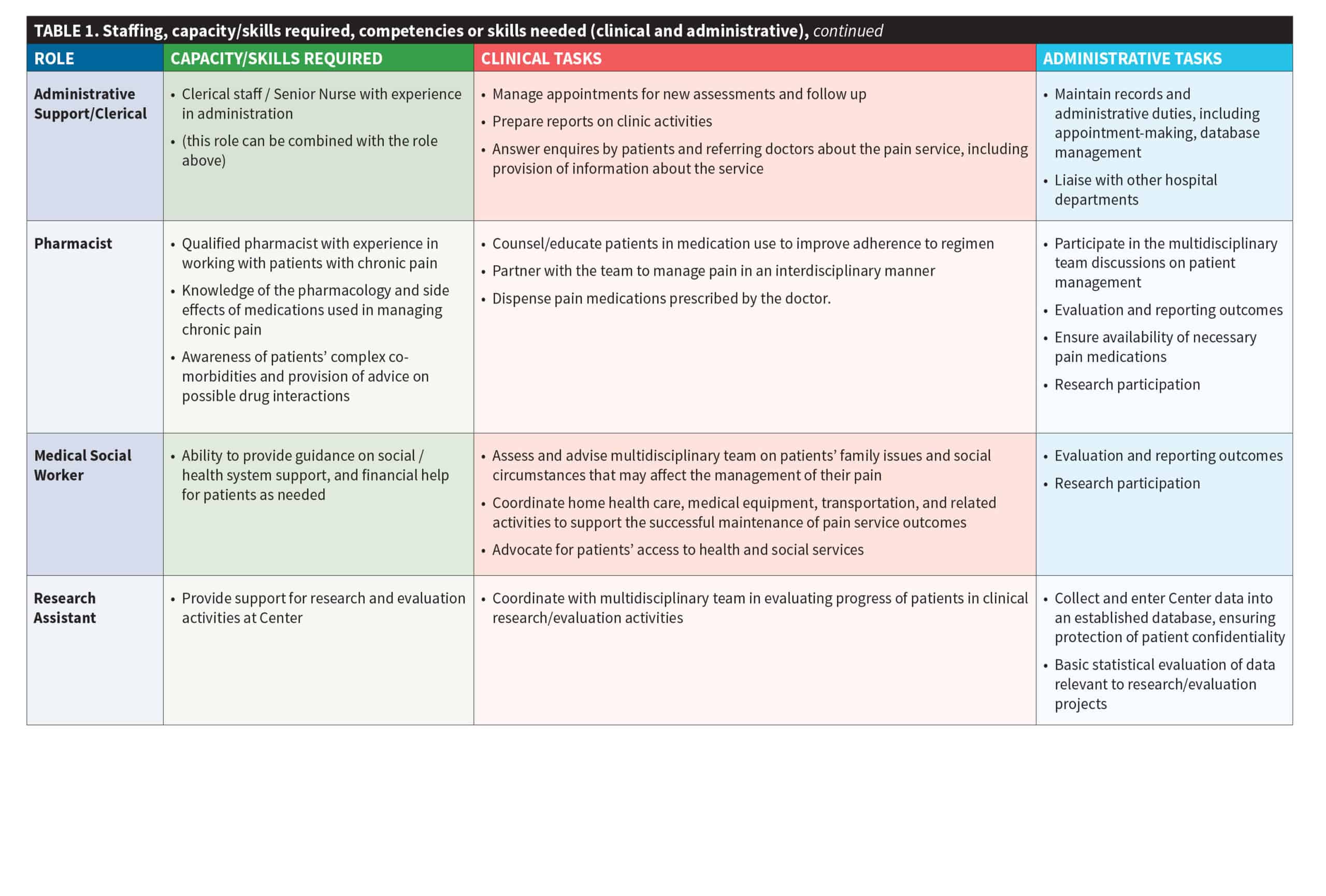
Rather than simply specifying which professional disciplines are required, the expert advisory group recommends that it is more practical to describe the main roles, capabilities, and tasks required from the participating health professionals (see Table 1).
Broadly, at least one member of a pain center needs to be able to assess and guide appropriate treatments for biological pathologies, and another member needs to be able to assess and treat psychological contributors to pain presentations. Other staff should be able to provide advice on exercises and activity upgrading. All staff should be able to provide basic education about pain in ways that are appropriate and make sense to the patients being treated. In many instances, these roles may overlap, but they all require coordination and planning. This means that attention needs to be given to how this will be achieved and who will be responsible for its oversight. It is critical that all members of the team work together in an interdisciplinary manner.
In this section, we describe the most common professional composition of the Multidisciplinary Pain Center (MPC) but recognize that the actual personnel available will vary across centres and countries.
Personnel
Adequate staffing is a critical part of a successful MPC. The collaborative and united approach of diverse personnel go beyond what many Southeast Asian health facilities typically offer. Achieving the recommended mix of staff may take time and patience, and will require a willingness to be flexible and to be open to compromise.
Below is a recommended list of both required and optional staff to operate an MPC. Founders of an MPC can begin with core required staff and add to their resources as their Center grows. Core required staff are indicated by an asterisk (*). Examples of position descriptions for core required staff are available as Appendix 3.
- A lead physician* in one of the disciplines listed below is essential. The physician must be interested and trained in managing patients with pain. Apart from the lead physician, the center should ideally have at least one other physician from any of the listed disciplines and should also have access to expertise as needed in relevant disciplines.
- Anesthesiology
- Rehabilitation medicine
- Psychiatry
- Surgery
- Primary care
- Rheumatology
- Neurology
- Palliative care
- Access to other health professionals in the following skill areas is also essential:
- Physiotherapy or occupational therapy*
- Clinical psychology*
- Nursing *
- Pharmacy
- Social work
- Office support/clinical administration*:
This may be a person with several responsibilities, and may be described as a secretary, receptionist, Center clerk. - Research personnel
Interested researchers or students from a local university may be available to participate in collaborative projects.
Achieving the recommended mix of staff may take time and patience, and will require a willingness to be flexible and to be open to compromise.
Roles, Skills, Clinical and Administrative Tasks
The main roles, tasks, and required skills for the Center staff are summarized in Table 1. The table is intended as a guide rather than a prescription. Each Center will need to consider its priorities and the resources available in deciding which mix will suit it best.
Recommended Prerequisites for All Personnel
The main objectives in this section are to ensure staff competency in the biopsychosocial assessment and management of pain. It
is anticipated that if all staff can achieve a reasonable degree of competency in the skills and characteristics outlined in this section it will greatly improve the effectiveness of the MPC.
Desirable characteristics for MPC personnel:
- Understand the main objectives of the MPC and act accordingly.
- Commit to working as a member of a multidisciplinary team.
- Understand the contribution of psychosocial issues to chronic pain.
- Show empathy to all patients.
- Possess and use effective communication skills.
- Understand and respect cultural norms in their respective communities.
- Participate in continuing professional development.
- Commit to ethical clinical practice.
Core competencies recommended for all clinical personnel
It is strongly recommended that all clinical personnel should feel competent in teaching patients pain self-management skills. Some personnel will have a high degree of competence, but all personnel should feel confident in their ability to augment their specialist skills with guidance and support for appropriate self-management practice by their patients, (See Training section).
The list in Box 2.1 is a basic set of competencies that can be learned during the intermediate level training course (Devonshire, Nicholas, 2018)
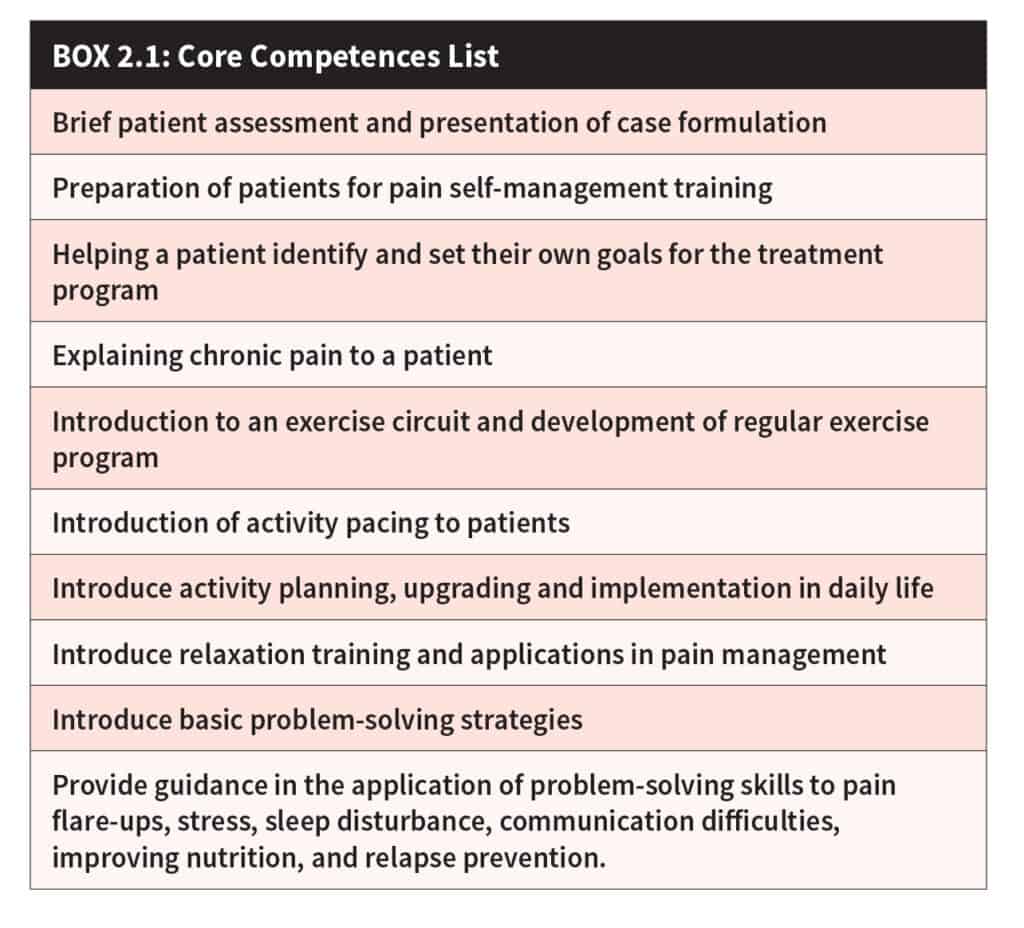
The first task for each center is to identify which health care professionals to train in pain management and at which level to start.
Training for MPC Staff
Training in interdisciplinary pain management should take a layered approach, starting with entry level (basic pain management concepts and skills), intermediate level (sufficient for active participation in
an MPC) and advanced level skills (required for development and supervision of training for other health professionals). Intermediate- level training is mandatory for those working in an MPC as part of preparation for establishing a Center.
The first task for each center is to identify which health care professionals to train in pain management and at which level to start. Ideally, all
those who deal with patients in pain in a hospital should have at least basic level knowledge and skills in this work. In the first instance, in the absence of formal training, the MPC personnel should act as models for other hospital staff.
Entry-level Training
Foundational entry-level training should be mandatory for all those intending to work in an MPC. It is also desirable for those interested in referring patients to the Center, as well as for relevant hospital administrators. Ideally, all frontline hospital staff should participate in entry-level training over time.
This training may be delivered by a local leader who has been trained by the IASP Multidisciplinary Pain Center Toolkit team. It is also recommended that a member of the IASP team should be present, at least initially, to assist in the implementation stages.
Recommended training for this level should include:
- Essential Pain Management (EPM) /EPM-lite: 4 to 8 hours
(See Appendix 4 for more information) - Model of care: A description of multidisciplinary care working in an interdisciplinary style: 1 hour
Intermediate-level Training
Intermediate-level training is mandatory for those working in an MPC. The personnel must have successfully completed all the relevant courses described below, as conducted by members of the IASP Multidisciplinary Pain Management Center Toolkit team.
Centers should support training for all personnel to achieve competence in the following tasks:
- Clinical assessment of pain: generic and discipline-specific,
2 to 4 hours - Case formulation (included in number 4 below)
- Pain management-pharmacological (prescribers need to have more in-depth knowledge of drugs, side effects, indications / contraindications, dosages and how to titrate to effect, while non- prescribers only need a superficial knowledge of this):
4 to 8 hours - Pain management-non-pharmacological: Training in ways of teaching pain self-management. Competency evaluation via two options:
- Face-to-face workshops (30 to 40 hours over four to five days) with observer-rated assessment of skills in role-playing at the end of the workshop, followed by 20+ hours of clinic-based practice with online follow-up with members of the IASP team as arranged.
- Online interactive webinar training (9 hours of weekly 90- minute sessions with a total of 20 to 30 hours of clinic-based practice between sessions)
- Follow up consolidation and support – online options, mentoring, supervision – by local experts with advanced level training and/
or external experts including workshop faculty. This can also be provided online. Examples include Project ECHO [1] and Continuing Online Professional Education, University of Sydney [2]
Advanced-level Training
Advanced-level training is mandatory for Center personnel working in leadership roles within their professional disciplines in an MPC. Consistent with the proposed “hub and spokes” model for developing country-wide multidisciplinary pain services, IASP expects that these individuals will take on training roles within their country. Leaders would build capacity by developing other MPCs within their country, and the original IASP MPC Toolkit team would no longer be required for this role. However, an extended mentorship could be offered to the local leaders by members of the IASP team, possibly by a series of online sessions to minimize costs and disruptions.
All trainers must have successfully completed the relevant courses outlined below, as conducted by members of the IASP Toolkit team. Recommended participants in the training include the following:
- Mandatory: Train-the-Trainer course delivered either face-to-face or via a series of interactive webinars. The face-to-face workshop would be 20 to 30 hours over three to four days while online webinar training would be 9 hours over six weekly or fortnightly sessions. Both would require clinic-based practice between sessions (for the webinars) or following the face-to-face workshop: 20+ hours over six to twelve weeks).
- Desirable: In addition to the mandatory training, participants should complete an observation period at an existing MPC. The period should last at least one week but preferably longer.
- Desirable: In addition to mandatory training, if feasible, it is recommended that participants experience further specialist training in pain management consistent with their professional discipline (3 to 12 months). If the lead physician already has a Masters-level pain management degree this can be reduced to 1-3 months.
Cost Issues
Face-to-face training is more expensive than online training due to travel and accommodation costs. Face-to-face training would require local fundraising to cover these costs.
Webinar training would require access to the internet and a computer with audiovisual capabilities. A small fee may be associated with the cost of the trainer and assisting technician, to be negotiated later, and no travel or accommodation costs would be incurred.
References
[1] Shelley MB, Katzman JG, Comerci GD, Duhigg DJ, Olivas C, Kalishman S, Monette R, Britt M, Flatow-Trujillo L, Arora S. ECHO Pain Curriculum: Balancing Mandated Continuing Education With the Needs of Rural Health Care Practitioners. J Contin Ed Hlth Professions 2017; 37(3): 190-4. DOI: 10.1097/CEH.0000000000000165.
[2] Devonshire E, Nicholas MK. Continuing education in pain management: using a competency framework to guide professional development. Pain Reports, 2018; e688.
This manual was produced independently by IASP with the support of an unrestricted grant from Pfizer Independent Grants for Learning & Change.
IASP brings together scientists, clinicians, healthcare providers, and policymakers to stimulate and support the study of pain and translate that knowledge into improved pain relief worldwide.