When pain is predictably provoked by mechanical stress, and eased by its alleviation, we quickly implicate a mechanical, or at least peripheral, nociceptive mechanism, and apply diagnoses like mechanical low-back pain that justify our favoured peripherally directed interventions. While the logic is attractive, what if central processes could mediate this presentation? Centrally mediated pain masquerading as peripheral.
We recently investigated the idea of centrally-mediated mechanical symptoms (Harvie et. al 2015 PDF). The study involved twenty-four people with the type of persistent neck pain problems seen in everyday practice, and all with pain on rotation. They performed head rotation to their first onset of pain (P1), in three virtual-reality conditions where the amount of rotation that they saw did not match reality. Instead, the viewed rotation was more or less than was actually occurring, creating an illusion of movement that was different to actual movement. Remarkably, pain with movement depended not only on how far people actually moved, but how far it appeared they had moved (see figure and explanation in caption below).
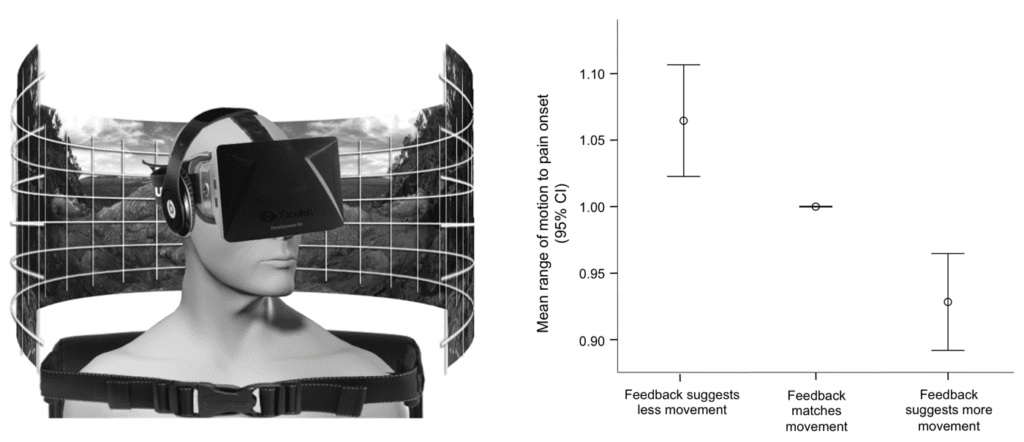
That pain with movement can be reliably modulated by the (visual) suggestion of more or less movement (i.e. by a non-mechanical input) is significant, and prompts us to reconsider the mechanical presentation.
In the past, perceptions such as pain were simply considered a read-out of incoming information. However, it has become clear that we could not make sense of the world if sensory information was not first filtered and arranged by our subconscious. In the case of visual perception, for example, the infinite array of colours, edges and shapes are arranged by our subconscious into the meaningful objects that we see and understand. Certain rules seem to govern this process — such as the way objects are arranged according to continuity of lines, colour and motion. The rules that govern the construction of pain, while only recently receiving attention, appear to involve the brains analysis of information relating to bodily danger. Nociception is the most obvious signal of danger to the body — but not the only one. Specific movements for example, might also become signals of bodily danger because of their meaning derived from association with injury. This would explain how (visual) signals of movement may have come to be a contributor to pain in these people with neck pain.
While ample research supports the idea that signals of threat influence pain, this study suggests specifically that information about the body in space (whether visual, proprioceptive or vestibular) that has been associated with an injury, might be relevant signals of threat. Indeed their influence may even result in a clinical pattern that appears mechanical, but is in fact centrally driven.
The treatment of threatening pain-associations is an ongoing field of study. In the meantime I think that there are a few things we can do to better align clinical practice with the threat-based understanding of pain that this finding aligns with. Firstly, we can expand our minds and clinical assessments to identify both nociceptive and non-nociceptive sources of threat (guaranteed we wont treat something we don’t assess!). Secondly, we can leverage our skills in education and behaviour therapy to encourage thoughts and actions that counter threat.
Some for some ideas about countering threat/threatening associations in the clinic:
- Nijs, J., Girbés, E. L., Lundberg, M., Malfliet, A., & Sterling, M. (2015). Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories. Manual therapy, 20(1), 216-220.
- Moseley, G. L. (2003). A pain neuromatrix approach to patients with chronic pain. Manual therapy, 8(3), 130-140.
- Russek L, McManus C. A Practical Guide to Integrating Behavioral and Psychologically Informed Approaches into Physical Therapist Management of Patients with Chronic Pain. Orthopedic Physical Therapy Practice. Jan 2015;27(1):9-16.
- Moseley, G. L, Butler D.S., Beams T.B., Giles T., J. (2012). The graded motor imagery handbook. Noigroup publications.
- Moseley, G. L, Butler D.S. (2015). The Explain Pain Handbook: Protectometer. Noigroup publications.
- Pain-related fear: Exposure-based treatment of Chronic Pain’ Editors: Johan W.S. Vlaeyen, Stephen J. Morley , Steven J. Linton , Katja Boersma , and Jeroen de Jong , 1st ed., IASP-press, 196 pages, 2012
Daniel Harvie
 Dr Daniel Harvie is a PhD graduate of the Body in Mind research group at the University of South Australia. His PhD thesis investigated a new theoretical model relating to how chronic pain develops – the Imprecision Hypothesis. Daniel is now part of the CONROD injury research centre at Griffith University, Queensland. Here he is focussed on better understanding chronic pain and developing brain-based treatments, with a specific focus on whiplash associated disorder. He has a clinical physiotherapy background, including a clinical masters, and has taught Pain Sciences and Clinical Reasoning to physiotherapy students.
Dr Daniel Harvie is a PhD graduate of the Body in Mind research group at the University of South Australia. His PhD thesis investigated a new theoretical model relating to how chronic pain develops – the Imprecision Hypothesis. Daniel is now part of the CONROD injury research centre at Griffith University, Queensland. Here he is focussed on better understanding chronic pain and developing brain-based treatments, with a specific focus on whiplash associated disorder. He has a clinical physiotherapy background, including a clinical masters, and has taught Pain Sciences and Clinical Reasoning to physiotherapy students.
References
Harvie, D. S., Broecker, M., Smith, R. T., Meulders, A., Madden, V. J., & Moseley, G. L. (2015). Bogus Visual Feedback Alters Onset of Movement-Evoked Pain in People With Neck Pain. Psychological Science, 0956797614563339. PDF




