Fourteen early-career pain researchers and clinicians are taking part in the fourth cycle of the PRF Virtual Correspondents Program. This science communications training program provides participants with knowledge and skills needed to communicate science effectively to a wide range of pain researchers, and to patients and the broader public. Throughout the course of the program, the Correspondents will conduct interviews and podcasts with leading pain researchers, provide news and virtual meeting coverage – and blog posts! Take a look at their posts below, which will be published weekly over the course of the next six weeks.
Meet the PRF Correspondents

Week 6: Wednesday, September 8, 2021
Blinding in Studies of Physiotherapy Treatments: A Bit of Magic, Creativity, and Deception
Assessing Pain Management on TV Medical Dramas
Engaging Patient Partners in Preclinical Research
Slow Diagnosis, Poor Treatment: Endometriosis as a Key Contributor to the Pain Gap
Are We Ready to Remove Diagnoses From Our Patients?
Think of It as a Science Blog After-Party
Tolerating Uncertainty: The Next Medical Revolution?
It’s Been a Pleasure to Blog for You
Reflecting on Five Weeks of Correspondence
Long COVID and Pain: Too Much Focus on Research and Not Enough Focus on Clinical Practice
Blinding in Studies of Physiotherapy Treatments: A Bit of Magic, Creativity, and Deception
Therapeutic ultrasound was once a mainstay of physiotherapy treatment. When I was growing up, it was one of the treatments you were pretty much guaranteed to receive if you visited a physio. However, by the time I was studying to be a physio, ultrasound was on its way out. We still learned about ultrasound, but there was a focus on the lack of firm evidence around its effectiveness in treating musculoskeletal injuries.
How does a treatment go from being a common and effective treatment, to something that is no longer recommended in clinical practice guidelines? In contrast to early studies, new higher quality studies, where both the therapist and participant are blinded, found that ultrasound has no effect when compared to a sham treatment (see here for a review).
Ultrasound is incredibly easy to sham; you simply turn the machine off and neither the therapist nor the participant can tell the difference. This means that ultrasound is incredibly easy to blind in clinical trials, and trials that do take advantage of this show that ultrasound has limited benefits in treating musculoskeletal conditions. Blinding is important; meta-analysis shows that treatment effects are exaggerated both when participants and assessors are unblinded.
However, I think that ultrasound has been unfairly maligned in physiotherapy. Physiotherapy treatments for pain have been considered to be impossible to sham, so in the majority of clinical trials participants and therapists are unblinded – think of massage, spinal manipulations, dry needling, and exercise. It’s obvious to everyone involved who is getting the treatment. This means that, just like the early ultrasound studies, the evidence for these treatments is clouded by non-specific effects. The positive findings in clinical trials may be reflective of the bias resulting from of lack of blinding, rather than true treatment effects.
That’s why this new study is so exciting, as the authors used deception and advice from magicians to successfully blind participants AND therapists to dry needling. The authors first sought the advice of masters of deception, magicians, to come up with a series of manipulations to trick both participants and therapists. For example, therapists were asked to ask participants complex questions at critical moments in the treatment (inserting the needles), which acted as a form of misdirection, or cognitive illusion, for both the therapist and the participant. Therapists were also asked to wear latex gloves. This acted as a contextual cue for participants (encouraging the belief that a needle was about to pierce their skin and gloves were needed for infection control), as well as a way to reduce sensory feedback of the therapists. Finally, the researchers used actors as “fake” participants, who pretended to have the opposite response to their allocated treatment (reacting strongly to sham needles, and no response to real needles). Together, these manipulations (and others in the full paper), were successful. Both participants and therapists were no better than chance at guessing their allocation.
This study shows that with a bit of magic, creativity, and some deception, it is possible to blind both patients and therapists to an intervention that was previously thought to be impossible to sham. I hope that this methodology is widely adopted in future dry needling studies, allowing us to truly understand the treatment effect of this intervention.
But more than that, I hope that the creative and novel approach used to develop methodology is used to create shams of other treatments. I would love to see other common physiotherapy interventions successfully shammed, so that we can better understand their effectiveness.
On another note: This will be my final blog as a PRF virtual correspondent. I hope that you have enjoyed reading my posts as much as I have enjoyed writing them. For all things affordances, placebo, and VR, give me a follow on twitter (@ErinMacIntyre5).
Erin MacIntyre, physiotherapist, PhD candidate, University of South Australia.
Assessing Pain Management on TV Medical Dramas
Are you one of the millions of people who tune into medical television shows? Perhaps your favorite is one of mine: M*A*S*H*, House, or Grey's Anatomy? If you do enjoy a good medical TV drama you may have found yourself picking up on some of the jargon or medical knowledge that gets discussed on the show. A study conducted in 2014 showed that viewers can absorb significant amounts of knowledge from watching just a few episodes. As a result, viewers of medical TV shows may not only gain medical knowledge, but these shows can also influence patient perceptions of medicine and disease treatments.
For instance, earlier this year, the Olympia Lab out of Pennsylvania State University published a study that aimed to understand how medical TV shows depict acute pain management and how those depictions may influence TV viewers’ expectations of pain management. The study consisted of two reviewers who independently observed eight medical TV shows (Chicago Med, Grey's Anatomy, The Resident, ER, The Good Doctor, The Night Shift, House M.D., and Code Black). Each reviewer watched the first 10-15 episodes from the eight designated TV series, for a sum of 300 observed pain patient scenarios depicted across the series. Pain was depicted either explicitly by the patient or implied by a traumatic injury. Other types of pain not related to traumatic injury were often inferred as a symptom of a separate disease diagnosis.
The demographic information revealed that the majority of pain patients portrayed across the 300 total TV episodes were adult (83%), white (72%), and male (67%). With regard to the origin of the pain portrayed during the shows, most patients had pain related to severe trauma. Trauma was characterized as being severe if the condition was life threatening (e.g., a gunshot wound); otherwise the trauma was considered mild (e.g., laceration).
The authors also reported that the majority of the pain medications administered on the TV episodes were non-specific; only about 10% of all included patient subjects received an opioid analgesic for pain management. That being said, only 17% of patient subjects were actually prescribed pain medication on the show. The authors noted that in real life a patient presenting with traumatic injury likely receives painkillers immediately upon entering the emergency room, but this is not necessarily portrayed on medical TV shows.
Interestingly, in the present study, only about 3% of the patients were assessed for their pain. Assessment of pain may include the use of the PQRST pain scale. This is a common tool that asks patients to rate their pain using a visual scale of pain depicted by facial expressions. This information helps medical professionals choose analgesics that best serve their patients and provides a tool to measure pain relief.
It is apparent from this study that there are large ethnic disparities with regard to portrayal of pain patients, as well as disparities between real-word treatment and medical treatment portrayed on television. Further, if pain is a significant component of many disease conditions and an experience among the majority of individuals, perhaps portrayal of pain by the media should be more diversified and inclusive of the populations that are impacted by pain conditions.
This was my sixth and final blog contribution for the PRF Correspondents Program. Tune in for my future podcast on acupuncture and pain treatment.
Britt Knight, postdoctoral trainee, University of Connecticut, US.
Living a life with a chronic pain condition is not easy. Despite continuous research and development in the treatment realm, the ‘gold standard’ of pain relief remains the opioid family of compounds, including morphine, tramadol, oxycodone and codeine. Yes, these drugs may help relieve pain but their side effects are numerous: drowsiness, constipation, tolerance (leading to a decrease in effectiveness) and possible physical dependence and consequential withdrawal. Non-pharmacological therapies, such as physiotherapy or even acupuncture, are also used as adjuncts to medicines, but these are also limited in their effectiveness. Therefore, so far, not ideal.
The pandemic, as we all know, had devastating consequences on healthcare systems, healthcare workers and the general population. But for those already dependent upon the support and care of their country’s healthcare systems for relief from chronic pain, there were additional consequences from the world rapidly turning upside down. With access to non-COVID-related healthcare restricted, approximately 70% of chronic pain sufferers deemed that their condition had worsened during the pandemic in terms of severity and/frequency of episodes and the impact upon their everyday lives.
Patients said that the lockdowns and infringements on our daily freedoms introduced new pain triggers and compounding factors such as anxiety, stress, loneliness, and insomnia, combined with a general decrease in physical activity. Over half of patients reported that they had combated their pain by either increasing rest time or taking more medication, with both of these coping strategies having obvious downsides.
By no means am I saying that chronic pain patients were unique in their increased suffering during the pandemic. All patients, no matter their ailment, faced enormous changes in their treatment, and doctors and nurses across the world moved mountains in order to deliver the best care possible despite the healthcare crisis. What COVID-19 did for chronic pain was to highlight the many sticking plasters and string holding the flimsy system of pain treatment together, along with the still limited treatment options.
So, in this, my last PRF blog post, I urge pain researchers to keep working. A conservative estimate puts the global burden of chronic pain at 10% of the world's population, and this is only set to rise given an aging population. Pain in and of itself, unlike diseases such as cancer, is not fatal, yet it drastically and negatively impacts the quality of patients' lives. We need more research into this subject with the (hopefully) consequential breakthroughs and new treatments that give patients more autonomy over their condition, and that will prove more robust against future pandemics and health crises.
So, my message to active scientists is this: Keep working. Future scientists: Choose to do research in the pain field. Everyone else: Educate yourself about the fascinating field of research that is pain, and support those working in it – we will get there.
Alice Gregorie, PhD student, University of Leeds, UK.
No man is an island, goes the poem by John Donne. The things that move us deeply tend to make a splash, and the waves they cause travel through us and on to those closest to us, for better or for worse. No amount of stoicism or down-playing will change this.
At some point during the struggle with a chronic pain condition, many patients worry what this means for their relationships. And it is true that chronic pain, like any severe disease, places a burden upon couples, most often financially and emotionally. Partners do not only have to deal with their own worries about the patient's condition, but also have to reinvent their own role within the relationship as a provider of care and support, all while navigating the changed distribution of domestic and wage work. In studies, about half of all spouses report a high or even severe degree of burden and one-quarter has to adapt their employment status in some way.
Chronic pain, although deeply personal and in a manner, private, therefore also affects the social circle of the patient. But social networks are not one-way streets. The way partners react to pain patients shapes not only the relationship, but to an astonishing degree also the pain itself!
This may not come as a surprise to PRF readers, since Wilbert Fordyce, the intellectual father of this notion, was also a founding member of the International Association for the Study of Pain. But I think it bears repeating: It is something that does not immediately come to mind (outside of the specialized field of pain research) and even then, might not be considered “real.” This is not surprising given the initial framing and phrasing of this effect in Fordyce's day as a simple learning mechanism, operant conditioning. In truth, the matter is not only more complex than this early model suggested, but it has also become clearer, and more pronounced, that the learned experience of escalating pain is far from a manipulative or attention-seeking ploy on the part of the patient. It is inherently unconscious and very much real: Brain imaging has shown that not only are pain thresholds in chronic pain patients lower when patients are alone than when accompanied by their significant other, but this is also reflected at the level of the brain in reduced activity in the somatosensory cortex when the partner is present, compared to the activation when the patient is alone.
But merely being present is not enough and can even contribute to a deterioration of the status quo. Such maladaptive partner reactions to a patient's pain behaviors have mostly been classified along the dimensions of solicitude and punishment (neither tells you what it is that you should actually do, only what you should avoid doing), or by using the characteristic of how validating a response is.
Solicitude in this context means any well-intended and caring response that nevertheless has a detrimental effect on the receiver of this form of support. This may encompass a range of desirable reactions that ultimately reinforce the pain experience, from giving a massage to encouraging the partner to forego meeting unwanted or difficult obligations, like household chores. In the short term, solicitous behaviors might bring a certain degree of relief to the partner, but there is ample evidence that this reverses in the long run. Punishing reactions in this framework refer to any directly negative reactions of the partner such as lashing out in anger or frustration. Clearly, neither is adequate. The concept introduced by Annemarie Cano might be of greater help here. She and her team added the important dimension of validating the partner's needs and experiences. According to their work, central to lasting positive support is not the response itself but its role as a mechanism to promote emotional intimacy and closeness within the relationship. This can be achieved in any way that conveys acceptance and an effort to understand the patient's experiences.
How these findings and concepts can be translated into therapeutic measures is still not entirely clear. However, the most important barrier any such measure will have to overcome is its acceptance in the patient community. Explaining that this is a real effect – no psycho-babble, no adverse side effects, no strings attached, just communication and training – will be the big challenge.
Malika Renz, PhD student, Central Institute for Mental Health, Mannheim, Germany.
P.S.: This is my last blog post as a PRF Virtual Correspondent. The time was much too short, and so were the word limits! I hope you enjoyed reading the posts, if you did read them –make my day and let me know. And if you didn't read the posts, let me know why so I can get better. 🙂
Engaging Patient Partners in Preclinical Research
Over the last year, I have been very interested in learning more about how our patient partners can effectively work together with researchers and clinicians in chronic pain research. Last week, as a Toronto Pain Institute Fellow, I had the fantastic opportunity to listen to some very insightful talks on how can we facilitate meaningful patient engagement, what the barriers/challenges in this area are, and the different roles/responsibilities that patient partners can assume in an academic environment.
Laura Bennett, a PhD student in the Bonin lab and my co-fellow in the program, had an interesting question for the panelists: “How can patient partners contribute to preclinical research studies and labs?” This is a great question because many studies that have provided patient perspectives in chronic pain research have focused on human subjects/clinical research utilizing qualitative data typically collected using interviews and surveys. But lately, especially in Canada, many grant funders and other stakeholders require meaningful public and patient involvement in the research process, since patients are the ultimate end-users of medical research and therefore should be involved in it.
I was curious to get more insight into this area and came across a recent review paper that provided an up-to-date description of opportunities for patient engagement in preclinical research. The authors used a standard definition of preclinical research, which is “laboratory research conducted in cell and animal models.” They talk about the barriers to patient engagement in preclinical research, such as a lack of interactions between preclinical scientists and patients in research (traditionally a non-public facing field) and differences in research knowledge and experience.
The authors also noted that patient partners could engage in preclinical research by having different roles at various stages of research, including the setting of research priorities, funding, study design, and dissemination of findings. Importantly, patient partners' role could be at multiple levels within one project, encompassing varying levels of engagement (awareness, inform, consult, involve, collaborate, empower).
The study also highlighted the importance of offering training sessions for researchers to facilitate science communication with patients and the significance of providing credit, both in terms of authorship and monetary compensation, to patient partners. One of the notable findings in the paper was the mutual benefit of patient engagement for both the preclinical scientists and patients, as this engagement provides an opportunity to build new skills, knowledge, interests, and understanding of each other’s perspectives, which led to better communication and rapport. Some barriers to successful patient engagement included a lack of clarity in defining patient roles in research, insufficient researcher resources including time and funding, and an inability to accommodate diverse viewpoints, especially in terms of decision making at different stages of the research process.
This paper does a very good job synthesizing current patient engagement practices in preclinical laboratory research and underscores the critical role of collaboration between preclinical scientists and patient partners at different stages of the research process. It also demonstrates the future potential and opportunities to develop and nurture this relationship, which is built on mutual understanding and trust with a common goal of reducing the public burden of chronic pain.
Lastly, I want to add that this is my last blog post as part of the PRF Correspondents Program and I would like to thank Neil Andrews, PRF editor, for his support since the start of the program. I also want to acknowledge my fellow PRF Correspondents for sharing their stories through their blog posts. It was an honor to be one of the fourteen PRF correspondents from across the globe.
Please keep an eye out for my interviews with Sarah D'Angelo and Emeralda Burke on facilitating patient engagement in research, through the eyes of a pain researcher and a patient partner. I will also be chatting with Dr. Kirsty Bannister from King’s College London, UK, about her translational work in human psychophysics and descending pain control.
Bhushan Thakkar, PhD student, Department of Physical Therapy, Virginia Commonwealth University, US.
Slow Diagnosis, Poor Treatment: Endometriosis as a Key Contributor to the Pain Gap

The gender pain gap refers to a tendency to dismiss pain reported by women. Part of this problem is the insufficient research into pain related to the female reproductive system. Endometriosis is a poignant example. Caused by the abnormal growth of endometrial-like tissue outside of the womb, this condition results in severe pelvic pain that affects 10% of women worldwide. Despite this, research into it is underfunded relative to diseases with similar healthcare burdens. To read more about how endometriosis causes pain, check out my post from last week.
Identifying the problem
Pain is a common reason for a trip to the doctor; it alarms us and indicates that something is wrong. However, if your pain is caused by endometriosis, you can expect to wait for an average of 8 years before receiving a diagnosis.
A lack of simple, non-invasive diagnostic methods contributes to this delay. If endometriosis is suspected, further investigations may include a physical exam or a scan like an ultrasound or MRI. However, these can all appear normal in patients with endometriosis, and diagnosis is only confirmed by a surgical procedure called a laparoscopy. Developing non-invasive tests would significantly help patients to access treatment earlier.
Biomarkers are quantifiable biological markers that correlate with a disease state. Various biomarkers, detectable in blood or urine, have been suggested for endometriosis. These include microRNAs, hormones and endometrial haptoglobin, a glycoprotein upregulated by endometriosis-related inflammation. Unfortunately, these have not yet been validated or developed for use in diagnostics.
Diagnostic delays may also be due to symptom normalization. Personally, I’ve had gynecological issues since my teens and like many teenage girls seeking help for severe menstrual pain, I was frequently dismissed with responses like, “You’ve got to learn to deal with this because it’s going to happen every month!” or I was accused of exaggerating to avoid school.
This dismissive attitude, born from a male-orientated history of medicine, is all too familiar to many women seeking help for pelvic pain. It reinforces the idea that pain is normal for women and maybe others just deal with it better! Ultimately, however, we can feel when something isn’t right and self-reports should always be taken seriously.
Treatment
What solutions can be expected once the hurdles of getting a diagnosis are overcome?
The three conventional options are: painkillers, surgery, and hormone treatments. As discussed last week, surgical removal of lesions improves pain but does not always eliminate it. Surgeries also pose the risk of increased inflammation and nerve damage and might exacerbate symptoms. Moreover, as endometriotic lesions grow back, additional surgeries are required to continually clear them.
Hormone treatments can provide some relief, as lesions grow in response to estrogen surges in the menstrual cycle. However, evidence for long-term benefits is lacking and with side effects such as weight gain, acne, reduced libido and low mood, many patients are reluctant to take them indefinitely.
Commonly used painkillers for endometriosis include anti-inflammatory drugs like ibuprofen or mefenamic acid. These improve pelvic pain by reducing levels of prostaglandins, which are compounds that mediate inflammation and contract the uterus during menstruation. However, these are most effective when taken in advance of pain bouts, which can be hard to predict.
Opioid painkillers like codeine can alleviate pain, but they also cause constipation, which in turn worsens pain, particularly as endometriosis is often accompanied by gastrointestinal disturbances. Anti-inflammatory agents like ibuprofen, and opioid drugs, are unsuitable for long-term use as they can damage the gastrointestinal lining or cause addiction, respectively.
Inadequate treatment options are why many seek alternatives. Of the common self-management methods, cannabis use and applied heat show the most effectiveness. Cannabidiol, the non-psychoactive component of cannabis, is a promising potential therapeutic for endometriosis due to its anti-inflammatory properties but would require validation through clinical trials.
Endometriosis is a disease with an unmet clinical need. Despite growing research and recognition, much catching up is needed to understand its etiology, pathogenesis and how to treat it.
With this I conclude my final blog post. Thank you for reading and engaging with me! I am grateful for this opportunity from the PRF Correspondents Program and, as always, feel free to continue the conversation with me via twitter @sofia_fg_9or via email: s.fontana-giusti@reading.ac.uk
Sofia Fontana-Giusti, research assistant, University of Reading, UK.
Are We Ready to Remove Diagnoses From Our Patients?
Commonly, clinicians see patients with chronic pain conditions who received diagnoses that are not useful anymore. How should clinicians deal with this situation? Recently, two authors published a paper proposing guidance for clinicians to remove diagnoses that are not beneficial in reducing people's suffering.
We live in a society that encourages timely and accurate diagnoses with the justification of giving patients the best opportunity for a positive health outcome. Diagnosis offers several advantages. Receiving a diagnosis or a clear explanation about the cause of a health condition is essential for establishing a good patient-clinician relationship. Patients with acute and chronic pain conditions usually report that diagnoses imply that the proper treatment will finally relieve the suffering. There is no doubt that, in some situations, an appropriate diagnosis guides treatments and saves lives.
However, we are too good at matching signs and symptoms to specific categories even when the signs and symptoms would not cause harm to patients during their lifetime. The indiscriminate act of diagnosing a health condition may cause problems instead of solutions, in some situations. Some diagnoses may lead people to limit their social participation and encourage them to undergo expensive, invasive, and ineffective treatments. For example, diagnosing “rotator cuff tear” as the cause of shoulder pain might encourage unnecessary shoulder surgery. Also, some people receive multiple diagnoses (overlapping diagnosis), and managing one condition may interfere with another.
The recent study mentioned above suggested that clinicians need to develop skills to dediagnose a health condition, in some situations. According to the authors, dediagnosing includes removing conditions that have resolved due to recovery, reclassifying or renaming diseases, and eliminating specific diagnoses that are more harmful than beneficial to the person's health. Clinicians should consider the patient's needs, preferences, and interests during the dediagnostic process and always think about when dediagnosing will benefit or harm the patient. It is not an easy task. Perhaps, dediagnosing is more complex than the standard diagnosis.
In one example, the authors tell the story of a 94-year-old woman diagnosed with osteoporosis. The diagnosis was still present, but the authors identified some disadvantages of sustaining the label. The woman expresses worries and uncertainty about the osteoporosis diagnosis and the accompanying risk of fractures. The osteoporosis diagnosis is associated with prescriptions of non-osteoporotic drugs with possible adverse effects. Therefore, the osteoporosis diagnosis seems to do more harm than good to the woman. The authors suggest that dediagnosing osteoporosis would be acceptable since the woman has a low life expectancy.
This decision may be controversial, but I would love to see more researchers discussing how clinicians could use the dediagnosing framework in clinical practice. Twitter: @rodrizzo_pain.
Rodrigo Rizzo, doctoral candidate, Neuroscience Research Australia (NeuRA) and the University of New South Wales (UNSW).
Think of It as a Science Blog After-Party
It’s hard to believe that our blog posts for this cohort of PRF Correspondents have come to an end. As I think back on my previous posts, I’ve come to realize how rich the experience has been, on multiple levels. I jump at any opportunity to hone my communication skills, particularly in a writing style that is tangential to scientific manuscripts. But perhaps of greater value is the introspection required when sharing my viewpoint. In science, we go out of our way to remove our own biases when analyzing and reporting our findings. Although I’m a naturally introspective person outside of work, it was refreshing to bring both worlds together – work and personal life – for a brief time. For my final post, I’d like to share how I’ll continue this exercise.
At our first meeting of 2020, the leadership at the University of Florida Pain Research and Intervention Center of Excellence (PRICE) pondered how to better carry out our mission in integrating research, treatment, and education throughout the year. If you hadn’t noticed, I place great value on communicating science to those outside of academia. So, my suggestion was to improve PRICE’s visibility through more intentional use of social media – particularly podcasting. In the time since, PRICE has brought our social media initiative online, beginning with Facebook (and soon expanding to Twitter), and has launched the PRICE of Pain Podcast, with its accompanying Instagram account.
Asked to spearhead the podcast project, I was ecstatic to bring our vision to life. I imagined passively facilitating an environment where researchers, clinicians, and industry professionals could determine the content as a conversation naturally unfolds. Carl Rogers would be proud! I didn’t realize it at the time, but I intended to urge the guests to do what I’ve done in this blog: integrate themselves with their science. This vision was probably motivated by my favorite part of any research presentation: the Q&A. No matter how polished a presentation is, the great ones are marked by a subtle shift where formality gives way to the vulnerability, motivations, and passions of the researchers as they interact with the audience. I’m fascinated when the enthusiasm of researchers is sparked and the human element of their work shines through. I set out to catch lightning in a bottle, hoping that this fascination is contagious. As our audience grows, we hope to raise awareness of pain research amongst the public, cultivate an interdisciplinary network amongst scientists, and help researchers and clinicians recognize each other’s blind spots as we seek to better understand and treat pain.
The PRICE of Pain Podcast is still a work in progress, but I hope that you’ll join us on YouTube or our audio-only versions wherever you listen to podcasts. In the meantime, I extend my deepest gratitude to you for following my blog as I’ve explored these topics and ideas!
Joshua Crow, PhD, postdoctoral fellow, University of Florida, US.
Tolerating Uncertainty: The Next Medical Revolution?
“Ironically, only uncertainty is a sure thing. Certainty is an illusion.” Simpkin and Schwartzstein, 2016
As human beings, we all want some sort of certainty in our lives. It keeps us grounded and gives us peace of mind. It gives us a sense of direction so that we know where to go next. Growing up, we’ve even been taught that it’s important to be certain, like when answering a multiple-choice question where there’s only one “right” answer, or when we need to make an important life decision.
But what happens when we can’t tell right from wrong? When uncertainty comes knocking at your door, how will you answer? In my final blog post, I’d like to share one of my favorite perspective papers, one that I find myself reading time and time again whenever I’m faced with some sort of uncertainty in my own clinical work.
As clinicians, we’re taught to look for signs and symptoms that fit a certain diagnostic criterion, we’re taught that when certain clinical tests are positive we can be more confident in our diagnosis, and we feel good when we’re able to provide patients a clear, rational explanation of their problem. But we also learn that not every patient will present with textbook signs and symptoms or a clear diagnosis, that clinical tests have specificity/sensitivity and positive/negative likelihood ratios behind them, and that there will be times when you have to convey some sort of diagnostic or prognostic uncertainty to patients.
In this paper, the authors argue that we need to be better at tolerating uncertainty and that a culture of not being able to do so can be detrimental. Work-related stress, excessive ordering of tests which carry a risk of false positive results, premature closure when making a clinical decision and diagnostic errors are examples of what happens when we are obsessed with chasing certainty.
So how can we become better at tolerating uncertainty? The authors propose that our educational curriculums need to emphasize reasoning, the possibility of more than one right answer and consideration of patient values. Educators can focus on “how” and “why,” instead of just “what,” and embrace the grayscale of human illness, which can’t be neatly categorized. We should think of a diagnosis as dynamic and evolving and that certainty is not always the end goal. We should also question how important it is to be certain about our diagnoses and if that will change our outcomes (speaking from a musculoskeletal point of view).
“We can speak about “hypothesis” rather than “diagnoses,” thereby changing the expectations of both patients and physicians and facilitating a shift in culture.”
Healthcare professionals should then be taught how to communicate scientific uncertainty – perhaps by providing some reassurance to patients as to what we know that isn’t the issue, by acknowledging the factors that make the individual sitting in front of us similar to others but also what makes them unique, and by giving them a sense of hope by discussing a plan B if the situation changes.
Lastly, I leave you with Osler’s maxim that “medicine is a science of uncertainty and an art of probability.”
Big thanks to the PRF Correspondents program for providing early-career clinicians and researchers such as myself with this opportunity and thanks to all the PRF readers for taking the time to read this. Whether you’re a clinician or researcher, I hope these blog posts have given you something to think about as we all work together towards improving the lives of those living with pain.
Derick Luu, DC, chiropractor, master’s student, rehabilitation science, McMaster University.
It’s Been a Pleasure to Blog for You
We often hear the saying, “What does not kill you makes you stronger”; it is very popular to say this today, and to say, “Be resilient.” The Bible promises that there will be glory in our sufferings. Dostoyevsky wrote, “The darker the night, the brighter the stars.”
Literature and religion somehow keep insisting that the agony of being in pain elucidates the worth of life, at least over the long term – that all the time spent staring into the dark, circling around our own personal anxieties, is not a terrible way of spending the night but rather a fundamental expression of our humanity. To be a person is to suffer.
For me, the choice to study neuroscience was mainly driven by my Catholic upbringing. I was an enthusiastic kid who could not keep quiet, and from the church I had received very few and very weak answers. It was also a natural progression from my literary interests in understanding consciousness and free will. When the time came to decide on a topic for my master's thesis, I was reading Crime and Punishment and it completely narrowed my interest to the complexity of pain. I was happy to find a laboratory focused on the processing of pain in the peripheral nervous system and where I was involved in developing targeted treatments for chronic pain.
For my PhD, I made the fortunate move up to the brain. I am now studying how chronic pain remodels neuronal structure in a particular area that integrates the sensory components of pain and contributes to regulation of emotions. In fact, the anterior cingulate cortex (ACC) lies in a unique position in the brain, right above the corpus callosum, with connections to both the “emotional” limbic system and the “cognitive” prefrontal cortex. Thus, the ACC is anatomically in the right place to play an important role in integration of neuronal circuitry for emotion regulation. It is a distinctive region for understanding the psychological and behavioral dysfunction that contributes to suffering.
Feelings and emotions greatly influence our behavior, which is a good thing. The ability to control and manage uncomfortable emotions is not only a skill that we all would like to employ in uncomfortable situations, but it is also a primary goal for mental health clinicians in treating chronic pain patients. Avoidance of painful emotions is often the motivating force for negative behaviors such as substance abuse, binge eating, and suicide; these actions are maladaptive approaches to control or regulate painful emotions.
Aside from the literature describing cingulate surgery for the treatment of various neuropsychiatric conditions, there have been several published reports about experiences with cingulate lesions for persistent pain. A report from the 1960s shows that patients who underwent this treatment said they continued to have pain, but that it was “not distressing,” “not particularly bothersome,” and “doesn't worry me anymore.” Much of the anxiety in these ill, unhappy people, was no longer apparent.
Understanding the processes by which the anterior cingulate cortex contributes to regulation of emotions at a high cognitive level is still largely mysterious and this is an extremely challenging and fascinating area of study. Hopefully, my work will help make those processes a little less unknown.
It’s been a pleasure to introduce you to my life as a pain researcher. I hope you enjoyed reading the blogs!
Federica Franciosa, PhD student, University of Bern, Switzerland.
Reflecting on Five Weeks of Correspondence
For the past five weeks, I have been granted the opportunity to participate in the Pain Research Forum Correspondents Program. When I joined the team of Correspondents, we were given carte blanche – complete freedom to decide the topics we wished to explore on this platform. Looking back at my previous posts, together we have discussed women and pain in a three-part conversation on female representation in fundamental research, acknowledgement of women’s reported pain in clinical practice, and the current crisis in endometriosis diagnosis and treatment.
Now that my journey as a pain blogger is coming to an end, I am surprised to see that I focused so much of my writing on women’s issues in chronic pain research, treatment and management. I currently work in a fundamental science lab studying mechanisms underlying osteoarthritic pain. I assumed that as a writer, I would not divert my attention far from my comfort zone. Although, in one post, we explored recent developments in fundamental research on arthritis and the use of medical cannabis to treat inflammatory pain, interestingly, some focus of the blog was on sex-differences in behavioral and inflammatory profile outcomes.
Within my posts, I also created Valérie’s Book Club where, every week, I recommended a book that illustrates how collaborations between patients and scientists can make immense contributions to the advancement of science and medicine. From the mental health community’s sentence of schizophrenic mothers in Hidden Valley Road: Inside the Mind of an American Family, to the personal accounts of women in science, either as a scientist in Lab Girl or as a patient in Ask Me About My Uterus: A Quest to Make Doctors Believe in Women's Pain, it is clear that the fields of science and medicine have neglected women’s interests, with repercussions reflected even in today’s practices.
What I now realize is that when I was given a platform, I chose to speak about women’s issues in pain science and medicine. This realization solidified my beliefs that I want to transition from the fundamental research world of chronic pain to the chronic pain management and treatment field. I wish to continue advocating for women’s health in a clinical setting and increase the visibility of these issues for the public via science communication outlets such as the Pain Research Forum.
This post is dedicated to all of the women close to me who suffer from chronic pain. I hear you, I see you, and I love you.
Valérie Bourassa, PhD candidate, McGill University, Montreal, Canada.
Long COVID and Pain: Too Much Focus on Research and Not Enough Focus on Clinical Practice
At the start of the first peak of the COVID pandemic in South Africa last year, I was working as a physiotherapist at a step-down rehabilitation facility. My therapy typically consisted of a six-to-eight-week personalized physical rehabilitation program aimed at returning participants to their meaningful life roles in their community and family after hospitalization. Given the focus of my work, my major concern about the pandemic was an anticipated large influx of patients who would be needing physical rehabilitation post-COVID infection.
Initially, I was anticipating patients post-COVID needing physical rehabilitation for conditions such as ICU-acquired weakness and reduced cardiovascular endurance post-hospitalization. Then, I came across Daniel Clauw and colleagues’ article, Considering the potential for an increase in chronic pain after the COVID-19 pandemic. This opened my eyes to the very real (and very scary) possibility that there may be a global exponential surge in the incidence and severity of chronic pain as a consequence of “pandemic stressors” (e.g., isolation, economic stress, and anxiety and fear around contracting the virus). Further, patients may present with pain as a consequence of a “post-viral syndrome.” The prediction of a post-viral syndrome has turned out to be fairly accurate, with many patients presenting with what is now termed “Long COVID.”
Long COVID refers to illness symptoms persisting after patients have recovered from acute COVID-19 infection. Symptoms such as pain, fatigue, fever, coughing and brain fog, to name a few, have been known to persist for months after the initial COVID-19 infection. Although data on long COVID are rapidly emerging, little is known about the physiological mechanisms associated with long COVID and which patients may be at greater risk of developing long COVID. Interestingly, severity of acute COVID-19 infection does not seem to predict long COVID; patients with minimal symptoms of acute COVID infection have reported having long COVID. Similarly, the presence of co-morbidities does not seem to predict long COVID; young, previously fit and healthy patients have reported having long COVID.
Clearly, there is an urgent need for researchers to gain an improved understanding of the mechanisms of and risk factors for long COVID. Fortunately, I think this need is being addressed. Large funding organizations have channelled large grants to research laboratories investigating the mechanisms of and risk factors for long COVID. Although this is encouraging and will hopefully lead to improved outcomes for people who are yet to contract COVID-19, it does not help the patients who are currently suffering with long COVID. There needs to be improved efforts towards (1) educating clinicians on early identification of long COVID; (2) establishing interdisciplinary clinics (e.g., doctors, physiotherapists, occupational therapists, psychologists, psychiatrists, social workers, as a few examples) for managing patients with long COVID; and most importantly (3) implementing patient-centered, interdisciplinary treatment strategies to reduce the symptoms of long COVID and improve functional outcomes. Unfortunately, steps 1-3 require vast funding. Therefore, I am arguing that large private and government organizations need to prioritize funding education for clinicians and establishing and running long COVID clinics so as to reduce the individual and societal impact of long COVID.
Gill Bedwell, PhD candidate, University of Cape Town, South Africa.
As defined by the International Association for the Study of Pain, pain is “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” (italics are the author's). This revised definition is convenient and necessary as now it includes all the chronic pain syndromes that are not directly caused by injuries or any apparent damage, such as fibromyalgia, stress-induced pain, migraine, and chronic low back pain, among others.
Considering that an injury is not really required to experience pain, it makes sense that emotional distress brought on by a breakup, the death of a loved one, an unexpected goodbye, social rejection, or any other stressful event, can be felt as a physical pain. “Your words hit me hard,” “this hurts,” and “my heart is broken” are phrases that people often use to describe their feelings. That last phrase just reminded me how Aristotle referred to pain as a “heart emotion,” comparing pain with pleasure as both were considered crucial expressions of the character or virtue of human beings.
One of the most iconic examples of pain as a heart emotion is the Takotsubo cardiomyopathy, or broken heart syndrome. People subjected to emotional distress – for example, a breakup – can feel symptoms similar to an acute myocardial infarction, including chest pain, difficulty breathing, fatigue, and sometimes back pain, with a spontaneous reversal of these symptoms as well.
But why can emotional pain also be perceived as physical pain? In the particular case of cardiomyopathy, it is believed that a sudden and large increase of circulating levels of catecholamines (adrenaline, noradrenaline, and dopamine), in response to the stressful event, can led to the chest pain. The heart is “connected” to the central nervous system through the vagus nerve; thus, the same neurotransmitters involved in pain modulation are activating their receptors at different sites.
On the other hand, many neuroimaging studies have found a significant overlap in the neural circuits involving both physical and emotional aspects of pain, in brain areas such as the anterior cingulate cortex, insula, amygdala, striatum and thalamus. Moreover, these areas are also involved with depression, anxiety, fear, and other behaviors closely associated with pain modulation. Interestingly, it has been reported that acetaminophen, a common painkiller, reduces the neural responses associated with social rejection, demonstrating a substantial overlap between physical pain and social pain physiology.
The complexity of pain results not only from the sensory, neural mechanisms of pain but also from the multiple circuits involved in the cognitive-affective aspects of pain experience, as well as from the effect of emotions on physical pain and vice versa. Pain is both terrible for patients and fascinating for scientists, and a complete understanding of these phenomena will take us a long, long time to achieve.
This is my last blog post, but it is definitely not a goodbye! Stay tuned for more content that we PRF Virtual Correspondents are preparing for you.
Finally, I want to thank Dr. Vinicio Granados-Soto and Dr. Francisco Mercado for their mentoring and for contributing to my scientific career, pushing me forward to be a better pain researcher.
Yarim De la Luz-Cuellar, PhD student, Center for Research and Advanced Studies, Mexico City.
Week 5: Tuesday, August 31, 2021
A Boxer, A Rock Climber, and the Incredible Hulk
Pain and Culture: Reflecting on Cultural Sensitivity in Healthcare
Changing the Emphasis From Fixing to Facilitating
Pain Catastrophizing or Pain-Related Worrying?
Women and Pain, Part 3: Endometriosis and Delayed Diagnosis
The Effect of Spicy Food on Sensitivity to Pain
Always a Bridesmaid, Never the Bride….
Pain affecting the low back region is a major health problem that becomes more prevalent with increasing age. Chronic low back pain (cLBP), or pain lasting at least three months, is the second leading cause of disability in the United States. To manage symptoms, patients may opt for nonpharmacological (diet and exercise) and/or pharmacological approaches (acetaminophen or anti-inflammatory drugs).
While chronic pain is likely the result of specific biological pathways involving both the peripheral and central nervous systems, pain is an individual experience that also includes a psychological component. Regular exercise is an essential aspect of both mental and physical health, as well as for managing chronic pain. A previous study on patients with knee osteoarthritis showed that at-home exercise programs can significantly improve knee pain up to two years. Although home exercise is clearly beneficial, a previous study showed that a majority of patients will not participate in at-home exercise programs.
Patients with chronic back pain often have a fear of movement, referred to as kinesiophobia, which can lead to passive coping strategies and a sedentary lifestyle, both of which can lead to psychological distress and physical disability. So the question becomes, How do healthcare providers promote at-home exercise therapy despite knowing that most people will not necessarily participate in these programs?
The combination of games and exercise therapy, referred to as exergames, is being investigated as an alternative method for motivating patients to participate in long-term at-home exercise programs. In 2013, one publication showed that industrial workers who used exergames on the Nintendo Wii had significantly reduced chronic back pain, and another publication showed that older adults who used Microsoft’s Kinect showed significant improvements in their hip muscle strength compared to those who participated in conventional training. Last November, the Laboratory of Müller-Werdan in Germany published a study on the use of virtual reality (VR) for managing chronic back pain in older adults.
For background, VR is a digitally created immersive experience. As opposed to holding a game controller to engage in a digital environment, the VR experience is observed through a special headset or helmet. While you can’t feel the elements of a digital environment (at least not yet!), wearing the VR headset tricks your brain into believing that you are someplace else without leaving your home. The authors of the Müller-Werdan paper showed that VR exergames are a feasible option for motivating older patients, and they proposed some guidelines for creating exercise programs for this pain cohort.
Investigations into the physical nature of VR games have demonstrated profound physiological effects, for instance, on heart rate and sweating, while immersed in a VR experience (e.g., game or video). Others have demonstrated that patients who experienced stroke and used VR treatment showed improved limb function, and that VR treatment can also result in pain reduction.
These studies show both the feasibility of using VR for therapeutic purposes as well as significant beneficial health effects for various patient populations. Moreover, with regard to costs, the price of a VR headset is minimal compared to the thousands of dollars that could be required for medical care, hospital stays, and rehabilitation. Although no single method may always be beneficial for treating pain, VR technology is a potential alternative or nonpharmacological approach that can be easily combined with other methods to promote a healthier and less painful physical experience.
Britt Knight, postdoctoral trainee, University of Connecticut, US.
A Boxer, A Rock Climber, and the Incredible Hulk
My PhD involves the use of virtual reality (VR), and as someone who a year ago had no idea what a head-mounted display or a graphic card were, I've experienced a steep but rewarding learning curve. The best part has been having the opportunity to explore VR literature. If you have some spare time, I highly recommend reading some papers in this area. It’s got everything – from having people embody (take on a virtual body, also known as an avatar) virtual lobster claw arms that open and close as you contract your abs, to improving the effectiveness of therapy by having people talk to themselves as Sigmund Freud. The creativity and innovation in this area is inspiring, and I can’t wait for VR interventions to hit clinical practice.
While doing some reading last week, I came across a case study where a 45-year-old man with longstanding low back pain underwent a four-week VR intervention aimed at improving pain and function. During the first session, the participant embodied three different avatars: a boxer, a rock climber, and the Incredible Hulk. The participant strongly identified with the boxer character, and so this avatar was used for the following three sessions. During the session, the participant was asked to “make muscle poses, throw air punches, and punch a virtual punching bag.” He completed three sessions in the lab, after which he took the VR home for a week.
The participant had good results from the treatment! He had improvements in pain (from 5/10 at baseline, to 2/10 at the end of the intervention). At a three-month follow-up, this pain reduction had been maintained, and the participant also had a significant reduction in disability compared to baseline.
But how does this work?
The exact mechanisms are still unknown, but I like to think of them in terms of affordances (check out my blog from last week for a quick run-down on this concept). If we view pain in terms of affordances, or possibilities for action in one’s environment, then embodying a strong avatar may work to shift one’s affordances in a way that allows for more meaningful engagement with the world. By embodying a boxer, the participant was able to take on some of the characteristics of a boxer, such as strength, power, and mastery. These characteristics may be able to shift one’s affordances. The sustained improvements at the three-month follow-up suggest that this occurs not only during the VR intervention, but that there is some carryover to the real world. Perhaps the shift in body perception was strong enough to impact the participant's affordances throughout his life – allowing him to engage differently with the world and therefore decrease his functional limitations over the three-month period until the follow-up.
However: This is all very speculative! We don’t have any definitive answers as to what is causing the observed results. These results also need to be replicated in larger trials (and tested against a placebo). But, as a proof-of-concept case study, this work opens the door to many new avenues of research, and eventually novel treatment options!
Erin MacIntyre, physiotherapist, PhD candidate, University of South Australia.
With news headlines, peer-reviewed studies, and even a Louis Theroux documentary, the opioid epidemic running rife in North America is notorious, and commonly mentioned in scientific publications and grant applications alike as part of the motivation to find non-opioid alternatives for pain relief. However, the growing opioid epidemic in large regions of Africa has yet to receive, and perhaps never will receive, as much scientific and media attention.
Rather than fentanyl, heroin, or oxycodone, in Africa tramadol is the most commonly abused opioid. A relatively weak analgesic in comparison to morphine (approximately one-tenth of the strength), tramadol is not yet listed as a controlled substance by the International Narcotics Control Board, and therefore does not fall under the same supply and prescription restrictions as other opioids. But tramadol's lesser potency is not reflected in repercussions from use of this drug, with Africa accounting for approximately 87% of global drug seizures in 2019.
With a high proportion of manual laborers, farmers, fishermen, etc., the majority of African tramadol users take the drug to allow themselves to work harder and for longer in order to have the best chance of retaining their jobs. By mixing tramadol with alcohol and/or energy drinks, a smaller proportion of users take tramadol as both a party drug and aphrodisiac. Despite being a prescription drug, tramadol can be freely bought both from pharmacies and street vendors alike, with expired and counterfeit pills finding their way into African countries from China and India. Consumption of counterfeit pills runs the additional risk of people consuming high doses of tramadol, undetermined doses, as well as unknown synthetic opioids, leading to possible overdose and death.
Despite similarities between the North American and African epidemics, there are obvious differences. Very few, if any, countries in Africa have the doctors and rehabilitation facilities to deal with the crisis. African border controls, being less stringent and often corrupt when compared with America, will continue to allow tramadol to find its way to street traders and consumers. America has attempted to deal with its own opioid crisis through stringent law enforcement and tough sentences for those found trafficking and possessing narcotics. This has proved costly and ineffective, and forces people into lifelong criminal activities to support themselves and their addictions, and thus the epidemic continues to grow.
The US has demonstrated that in the "War on Drugs," drugs have definitely emerged victorious. Access to opioids is still required for legitimate pain relief for patients, and therefore a total ban on opioid supply is not the answer. Instead, African and other countries now have the chance to implement a more holistic and evidence-based strategy, with drug policies based on education and community outreach rather than heavy-handed treatment of users as criminals and giving users prison sentences. Although there is no easy solution to these catastrophic opioid epidemics, a more humane course of action may lead to more hopeful outcomes for both individuals and the African continent.
Alice Gregorie, PhD student, University of Leeds, UK.
Pain and Culture: Reflecting on Cultural Sensitivity in Healthcare
“In our faith we don’t say much about pain. He learned to be quiet and we didn’t know he was so sick.”– Ruth Davidhizar, personal anecdote (see paper here).
Pain and culture is a topic that seems to be overshadowed by the more popular aspects of the biopsychosocial model like stress, psychological comorbidities, and socioeconomic status. But once you start thinking about it, the relationship between pain and culture becomes quite apparent in healthcare. This can be seen in the form of traditional medicine healers, different cultural pain-relieving remedies, an immigrant struggling to find a healthcare practitioner who speaks their language, or a child helping to translate in English to the doctor how her mom is feeling.
Culture is a strong force that can shape one's own beliefs and behaviors. In turn, this can influence not only how pain is experienced but also how it’s expressed. While pain is a universal phenomenon (minus those with congenital insensitivity to pain), there appear to be differences in how certain cultural groups perceive and express pain.
But how does this impact those working in healthcare? In this blog post, I’d like to highlight a few key points of this paper, where the authors conducted a literature review of the care of culturally diverse patients in pain. The authors formed seven key strategies to help improve a healthcare practitioner's cultural sensitivity.
One strategy is simply to have an appreciation of the variability in how one affectively expresses pain. Cultural responses to pain can be stoic, where individuals are less expressive and tend to “grin and bear it,” or the responses can be emotive, where individuals are more likely to verbalize their expressions. Your intuitive reaction to a stoic individual may be that they aren’t in that much distress, thus downplaying their pain experience, while for an emotive individual, you might think they’re over-reacting. Take a moment to reflect on how your perception and behavior changes as a healthcare professional when interacting with a stoic versus emotive individual.
The next strategy is to have an appreciation of different communication styles. For example, an individual may feel that nonverbal expressions such as wincing or groaning are sufficient to communicate one's own experience of pain, whereas another individual may use vivid descriptors to express what they’re feeling. Additionally, in some cultures such as in East Asians, asking for assistance may be considered disrespectful, as it may be viewed as taking a doctor or nurse away from more important duties.
Another thing to consider is the kind of historical or cultural ties that a treatment has. For example, would there be a different effect if acupuncture (a popular medical treatment in East Asia) was provided to someone who has never heard of it, versus someone who grew up in a traditional East Asian household, where acupuncture was the first option for any sort of aches and pains, and all they hear from close friends and family members is how effective acupuncture was for them?
One final strategy worth mentioning is to explore your own personal biases and prejudices as a healthcare practitioner. Whether implicitly or explicitly, we are all shaped by our own cultures, beliefs, and values, which may influence how we view and act with those who are different from us. Therefore, it may be a good idea to once in a while take a moment to pause and reflect on our own cultural sensitivity towards others.
Derick Luu, DC, chiropractor, master’s student, rehabilitation science, McMaster University.
It can be considered a cliché to say that politicians often lie. But lying is not a “skill” that particularly belongs to them. It is part of everyday life in any kind of job or situation.
Each student enrolled in my PhD program should attend a course on scientific integrity. I attended the course last year, which was held online. The teacher appeared on my computer screen and asked all the students if we had lied in the past few hours. I had spent the entire morning analyzing my experimental data, which, although tedious, was relatively straightforward to do. Yet I blushed at the teacher’s question.
What if I had done something wrong in my analysis? Copying-and-pasting is a repetitive, quick action that can easily cause mistakes, which are all but natural to occur.
I followed the course and learned about scientific misconduct. I went through my data again to make sure that everything was correct, and fortunately it was. I could only think of accidents and/or oversights that could lead to a mistake. Falsification and fabrication of data never crossed my naïve mind.
Curiosity and ambition are important for scientific research. However, it is not uncommon for the latter to get the better of the former, driving one to resort to desperate measures in the quest for recognition and success. Cases of plagiarism, fraud, data fabrication, and theft were, are, and probably will be discovered. These are clear examples of misconduct.
Questionable research practices are less obvious cases of scientific misconduct and are also more difficult to detect. They can be the reuse of data, which happens when authors recycle figures from published papers without stating so; conflict of interests among journals, reviewers, and competitors; and failure to acknowledge the ideas and contributions provided by others. They can also involve misrepresentation, inaccuracy, or bias.
The intense pressure to publish abundantly in order to remain competitive for funding can lead some scientists at any step of the career ladder to skirt the boundaries of ethics. Applying the “scientific method” does not seem to be enough anymore to be successful. The academic environment is often stressful. Making a mistake could harm the perpetrator with dire personal consequences. However, the impact on the community and other authors is also just as relevant.
It must remain a priority for all scientists to meticulously review their own manuscripts and train their mentees to do conscientious research.
Asking yourself, every day, as a scientist, and as a person as well, “Did you lie today?” is a simple habit that can be very beneficial. Not only does it encourage high standards of scientific conduct, but it also renews the genuine curiosity that ultimately promotes the aims of ethical research, such as knowledge and truth.
Federica Franciosa, PhD student, University of Bern, Switzerland.
Changing the Emphasis From Fixing to Facilitating
Pain promotes behavior change; it motivates us to seek help. Patients seek help from healthcare professionals (HCPs) to take their pain away – to fix their “pain problem.” In return, HCPs offer patients treatment interventions such as surgery, exercise, medication, and manual therapy manipulations to fix the pain. These treatments are frequently framed as interventions needed to fix the problem, needed to take the pain away. But do HCPs really have the ability to fix pain?
The body strives to restore homeostasis after insult. Tissues heal after damage. However, the ability of the body to restore homeostasis and heal damaged tissue is undervalued. Too frequently HCPs downplay the power of the body to heal itself, which leads to patients not understanding and not appreciating their body’s fantastic ability to restore homeostasis and heal damaged tissue. Patients develop misconceptions that their body is fragile and vulnerable to re-injury.
I believe that presenting interventions as being the key to fix the pain is naïve and inaccurate. HCPs cannot and do not fix pain. This may sound counterintuitive, but bear with me as I justify this claim with an example. Surgical intervention following a fracture is often vital to reduce pain and stabilize the fracture. However, the surgery does not fix the damaged tissue, nor does it fix the pain. After the surgery, the body will promote callus formation at the fracture site and heal any soft tissue that was damaged at the time of the fracture. Broadly speaking, as the tissue heals and the peripheral inflammation resolves, there will be reduced activation of peripheral nociceptors and the pain will subside. The surgical intervention, physiotherapy exercises, and medications administered by HCPs did not fix the fracture and the pain. Instead, these interventions facilitated the body's ability to fix the fracture and the pain.
I believe it is important for HCPs to frame treatments with this narrative: Our bodies are robust and are generally excellent at healing themselves, and HCPs have useful treatment interventions that can help our bodies to promote healing. HCPs have the responsibility to accurately explain the role of their interventions, without overestimating their value. I believe that changing the emphasis of the role of medical interventions from fixing damaged tissues to facilitating healing of damaged tissues will promote resilience and reduce fear-avoidance behaviors after injury.
Gill Bedwell, PhD candidate, University of Cape Town, South Africa.
Pain Catastrophizing or Pain-Related Worrying?
Some researchers have raised concerns about the capacity of existing self-report measures to capture the concept of pain catastrophizing defined in the cognitive-behavioral literature as “to view or present pain or pain-related problems as considerably worse than they actually are.”
Pain catastrophizing
The term “pain catastrophizing” emerged when researchers observed that people have different responses during painful events. Commonly, people who experience pain try to find ways to tolerate, minimize, or reduce the discomfort of their experience. Researchers found that people usually shift their attention from the painful sensation, imagine something else, tell themselves that everything will be all right, and keep urging for relief from the pain as soon as possible. Some of these coping strategies might be useful in some contexts, but may become unhelpful in other situations. For example, urging for immediate pain relief may be helpful if someone has an injury but becomes less important when the person has a chronic pain condition and has already received adequate health care.
The evidence of maladaptive cognitions led researchers to identify “exaggerated negative thoughts brought to bear during actual or anticipated painful experiences.” Researchers proposed a list of thoughts to develop “pain catastrophizing” scales. The development of these scales opened the opportunity to explore the influence of pain catastrophizing in clinical and experimental research. The term “pain catastrophizing” became popular in the pain field.
Thirty years have passed, and the exaggerated negative mental set has been considered one of the most important predictors for chronic pain. For example, a meta-analysis with 30,000 patients found that levels of pain catastrophizing before surgery predict the persistence of pain after surgery, even considering the possible influences of primary diagnosis, surgery type, and study design. The problem is that the research community accepted the items of pain catastrophizing scales as a precise way to capture the conceptual idea of pain catastrophizing. For several years there were no studies investigating the degree to which the content of the measurement instruments reflects the idea of pain catastrophizing.
Pain-related worrying
Then the question arose: Can we really measure the concept of pain catastrophizing with the existing self-report measures? In 2020, a group of researchers decided to answer this question. The authors created a long list of items from six pain catastrophizing measures as well as items from worrying, vigilance, pain severity, distress, and disability questionnaires. Using an online survey, the researchers asked people to determine the relevance of each item from the list with the definition of the existing psychological concepts (e.g., pain catastrophizing, pain-related worrying, distress). The authors expected to find higher scores for pain catastrophizing items with the instruments of pain catastrophizing. The study revealed that items from pain-related worrying, vigilance, pain severity, distress, and disability were consistent with their respective concepts.
In contrast, items from pain catastrophizing scales were associated with pain-related worrying and pain-related distress definitions. For example, a common thought, “When I am in pain, I anxiously want the pain to go away,”did not relate to pain catastrophizing. Instead, this item was an example of pain-related distress. Even statements consistent with the concept of pain catastrophizing (e.g., “This will never end”) was also related to pain-related distress. The study showed that disentangling pain catastrophizing from pain-related distress is almost impossible. For this reason, the authors suggest using the term “pain-related worrying”to capture both pain catastrophizing and pain-related distress.
Should we recognize that we cannot capture pain catastrophizing as defined in the cognitive-behavioral literature? Twitter: @rodrizzo_pain
Rodrigo Rizzo, doctoral candidate, Neuroscience Research Australia (NeuRA) and the University of New South Wales (UNSW).
Are the Prescription Opioid Tapering Guidelines for Patients With Chronic Pain Working? Or Do We Need a New Approach That Focuses on Clinical Data and Patient Neurobiology?
Millions of Americans and people around the world use opioids to treat their chronic pain. In 2016, within the context of the ongoing opioid epidemic and the lack of consensus amongst physicians regarding opioid prescription, the Centers for Disease Control and Prevention (CDC) released new guidelines that cautioned clinicians about both starting new opioid prescriptions and increasing the dose of existing prescribed opioids. The CDC recommended tapering of opioids with careful consideration of the benefits and risks of treatment options.
The overall volume of opioid prescribing (almost 57%) decreased over the next year, and different institutions across every state limited opioid prescriptions and encouraged physicians to taper opioids. One of the causes of this decrease was attributed to the involuntarily tapering of opioids in patients who were on long-term stable opioid therapy. The other reason was that fewer new opioid prescriptions were prescribed.
Thus, to examine the potential risks of opioid dose tapering, Agnoli et al. published a study this August that found a 68% increase in overdose events, and a doubling of mental health crises, among tapered as compared to non-tapered patients. Furthermore, the risks of tapering were greater in patients who had faster dose reductions and higher baseline doses.
This study, unfortunately, underscores the concerns that Beth Darnall, a Stanford pain scientist, and colleagues had raised in 2019, in a letter published in Pain Medicine. The letter petitioned lawmakers in the US to alter the CDC guidelines and guide the “development and implementation of policies that are humane, compassionate, patient centered, and evidence based in order to minimize harms and protect patients taking long-term prescription opioids.” Although opioid tapering guidelines were issued to improve patient safety and health, many other studies have highlighted similar concerns, demonstrating that reduction or discontinuation of prescribed opioids can actually increase the risk for overdose deaths, suicide, increased pain, fear of pain, and mental health crises.
Dr. Darnall and Dr. Howard Fields, in their perspective published in PAIN this August, advocate for an approach to opioid tapering “using neuroscience-based concepts, clinical data, and patient centeredness that addresses patient expectations and values patient autonomy.” They highlight the limitations of the opioid tapering literature and remind everyone that a one-size-fits-all regulatory “solution” fails to address the specific needs of these patients. To be truly effective, they recommend working with patients to adjust the taper (addressing their willingness to try a taper and their expectations); identifying other medications and nonpharmacologic options; working with patients to evaluate and treat any comorbid psychiatric conditions; and recognizing those who do not receive analgesic benefits from opioid therapy. Dr. Darnall has published work (see here and here) in the area of patient centeredness in opioid prescribing.
Incorporating pain education into the training of all clinicians and using motivational interviewing to engage patients, providing digital behavioral pain medicine, utilizing harm reduction strategies, and reducing stigma amongst clinicians towards opioids are some of the other steps many previous studies have found to improve pain and function in chronic pain patients.
Bhushan Thakkar, PhD student, Department of Physical Therapy, Virginia Commonwealth University, US.
I am writing this post from a city I do not (yet) know, in a country I have never visited before, trying to tell the person whose language I do not speak that I would like whatever is on the menu today, and WiFi. In short: It's my one long vacation of the year and I am loving it.
And on this trip, I am so embedded in thinking and writing about pain that I wonder: Does the shop owner (who is now bringing me some sort of … hot cake?) experience pain the same way I would? Pain is universal, but it is, after all, also subjective. How would he talk about being in pain? How would he deal with it?
Since pain is such a personal thing, there is probably little that doesn't affect how we experience and express it. Age plays a role, and education. Gender absolutely does. So does socioeconomic status and the relationship you have with your clinician. But culture? How would one even go about measuring cultural effects on pain experience and expression?
The first problem I ran into was that it is practically impossible to come to a definitive answer when trying to measure differences in pain experience: Every meaningful measure of pain that we have is based on someone's ability to introspect and to communicate, even those that are used in laboratory settings to quantify sensory perceptions. Given this inherent problem of objectively assessing something that lives in the subjective – psychology and psychiatry are struggling with this as well, believe me – what sense would it make to separate pain experience and pain expression to find out how the two might differ from culture to culture?
One way around that problem is to reduce it to the expression part and be mindful of that small limitation. Fine by me: I have always been more interested in what you say you feel instead of trying to find what you might objectively, supposedly feel.
But browsing the literature, I promptly stumbled over the next hurdle: The vast majority of research contrasts immigrants and their first- or second-generation descendants with the local population in – you guessed it – industrialized, mostly Western countries. That is comparing ethnic majorities to minorities, and one group that has access to culture-congruent healthcare to one that potentially has not! From this perspective, it cannot be surprising that African and Hispanic Americans report more severe chronic and acute pain, have higher pain sensitivity, and experience lower pain tolerance levels (see data from these reviews here and here).
There are a few studies that address this problem by comparing data acquired in different countries using the same protocol. Sure, if we wanted to carry this to extremes, we might need to take a long hard look at how “culture fair” our tools and questionnaires are. Psychological test theory has long since worked on the premise that tests and questionnaires are culturally loaded, based on their use of language or other implicit knowledge. In the case of intelligence tests, a lot of work has gone into constructing tasks that specifically measure the construct intelligence and nothing else. For pain, we have a non-numeric rating scale that uses smiling and frowning faces….
But maybe I am missing the point here entirely. Maybe it really is less important to know who presents with more or less pain due to their cultural background. When someone is in pain, you try to help them, no matter what and why. The how, on the other hand – how coping works, what resources the different cultures offer to deal with pain, especially with chronic pain – is a field of study that could really make a difference. If your status as the strong head of the family allows you to power through the exercises with your physiotherapist, you embrace it. If your faith in a higher being putting you to the test will give you an ounce of relief from your pain, I will pray with you. If stoicism is what lets you bear your illness, no one has a right to tell you it's bad because you really need to express yourself more. Pain is a formidable enemy. We cannot afford to sneer at anything just because it is foreign to us. We should not exclude it from our research and our curiosity.
Malika Renz, PhD student, Central Institute for Mental Health, Mannheim, Germany.
“The idea that women have to get used to and put up with menstrual pain is almost embedded in our DNA. It is somehow normal that this pain shouldn’t be of concern, treated, or investigated. But anything that affects well-being needs to be treatable.”
– Professor Philippa Saunders, University of Edinburgh, via this article.
Women are more likely to experience chronic pain, which is in part due to the existence of several disorders that affect only the female reproductive system. In this blog post I will focus on one such example: endometriosis. This painful condition affects 10% of women worldwide, which in the UK is a similar number to that of women affected by diabetes.
In a healthy state, the tissue lining the womb grows and sheds each month, under hormonal control. In endometriosis, this lining (called the endometrium) starts to grow outside of the womb in areas where it shouldn’t be, such as the ovaries, nearby ligaments, the lining of the pelvic cavity (peritoneum), bladder, or intestine.
Most commonly this ectopic tissue is found near the reproductive system. It is also possible, though rare, for it to travel to distant parts of the body via the blood or lymph. Wherever it is, endometrial tissue responds to the hormonal fluctuations of the menstrual cycle, thickening and breaking down each month. As it cannot exit the body via the vaginal canal as usual, it becomes trapped to form lesions.
This debilitating condition often begins in early adolescence and has pain at its core, with the major symptom being severe pelvic pain that is constant or follows a cyclic pattern. Many additional symptoms can occur, and these vary depending on lesion growth and location.
Endometriosis-related pain is described as nociceptive, inflammatory, and neuropathic.
“Nociceptive” relates to the physical pain we are most familiar with – when something that causes bodily damage hurts us, like dropping something on your toe. Sensory neurons called nociceptors convert this stimulus into a biochemical neural signal that is transmitted to the central nervous system (CNS), including the brain where the experience of pain is created.
Endometriotic lesions act as painful stimuli and directly activate nociceptors. Various studies (such as this one) have shown that nerve fibers resembling nociceptors are found at a higher density in the peritoneum of women with endometriosis compared to those without the condition. Furthermore, pelvic pain is more severe when these fibers are closer to the lesions.
If this pain is simply nociceptive, it would make sense that you could eliminate the pain by removing the painful stimulus, i.e., the endometriotic lesions. Indeed, surgical removal of these lesions significantly improves pain in most patients, but does not eliminate it, indicating that there is a lot more going on.
When lesions break down during menstruation, this causes pockets of inflammation to form, contributing to flare-ups of pain around this time. Inflammation involves immune cells and molecular mediators that amplify pain, many of which (such as monocytes and cytokines) are elevated in the peritoneal fluid of women with endometriosis.
As well as sensitizing areas of endometriosis to painful stimuli, inflammatory processes appear to drive the growth of endometriotic lesions, for example, by creating new vessels around them to increase their blood supply.
The third type of pain, neuropathic pain, is caused by damage or dysfunction to nerves. This pain type is present in some people with endometriosis, usually due to lesions growing near or even inside a nerve.
Some with endometriosis may also feel pain away from the pelvic region, in areas innervated by the same nerves as the reproductive system, such as lower in the leg. This symptom, known as “referred pain,” may also have a neuropathic cause. While inflammatory features have been the focus of endometriotic pain research, neuropathic involvement is steadily gaining research interest.
With such a large proportion of women suffering from this chronic, painful, and (currently) incurable disease, research is paramount. Stay tuned for Part 2, where I will discuss the current state of treatment and research into endometriosis.
Sofia Fontana-Giusti, research assistant, University of Reading, UK.
Women and Pain, Part 3: Endometriosis and Delayed Diagnosis
In the past few weeks, we’ve been talking about women and pain, and how a woman’s pain is more likely to be dismissed by a health care provider than a man’s pain is. Today, I want to continue the conversation by tackling a topic that is very close to my heart: pelvic pain and endometriosis.
Endometriosis is a pathology where tissue normally found in the endometrium, the lining of the uterus, is found outside of the uterus, on and around other organs such as the pelvic peritoneum, the ovaries, the recto-vaginal septum, the bladder, and even the bowel. This causes chronic inflammation and the accumulation of scar tissue. Most importantly, the patient suffers from chronic pelvic pain, and pain during menstruation, ovulation, and sexual intercourse, and is associated with heavy bleeding, fatigue, and a notable decrease in physical, mental, and social wellness. Endometriosis affects one in 10 women, with an estimated 176 million women around the world currently suffering from the disease (see here and here).
So what is wrong with this picture? Well, of the symptoms associated with endometriosis mentioned above, most of them would be accepted and expected to occur during normal healthy periods. As a result, endometriosis is often missed, and diagnosis delayed. In fact, women suffering from endometriosis will go between 6 to 11 years before receiving an official diagnosis, despite continually seeking treatment for their symptoms.
What needs to change? We need to stop accepting chronic pain as a normal side effect of menstruation and encourage women to seek medical advice if they are experiencing constant discomfort. Most importantly, clinical standards to address pain in women’s health must change. Check out this week’s book recommendation for a compelling illustration of this issue.
Valérie’s Book Club:
Do you want to read more about how science communication can impact knowledge and discoveries? Join my book club! Every week, I will be recommending a book that illustrates how collaborations between patients and scientists can have immense contributions to the advancement of science and medicine.
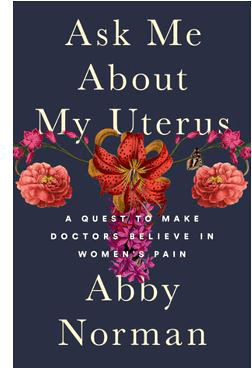
This week’s recommendation is Ask Me About My Uterus: A Quest to Make Doctors Believe in Women's Pain, by Abby Norman (2018).
This is the true story of a woman who was repeatedly hospitalized for excruciating pelvic pain, only to be sent home with antibiotics for urinary tract infections every single time. In this book, the author recounts the journey of how the failures of her health care providers to correctly diagnose her endometriosis, and their constant dismissal of her chronic pain, impacted her physical, emotional, and interpersonal well-being. As she states it best, being a woman is NOT a pre-existing condition.
Valérie Bourassa, PhD candidate, McGill University, Montreal, Canada.
The Effect of Spicy Food on Sensitivity to Pain
It is well established that pain experience can be influenced by many social and cultural factors. Recently, the relationship between diet and pain sensitivity, as well as the role of diet in chronic pain management, is another such factor that has received attention from researchers.
In Mexico, spicy food is a daily obligation in our diets, even for children. With more than 200 varieties of chili peppers and infinite ways to prepare them (fresh, dried, roasted, in sauces), we Mexicans are so familiar with chili peppers that the sensation of a burning mouth when eating is completely normal and sometimes unnoticed. Even candy and fruit are usually sprinkled with chili powder. Food that is not spicy equals insipid food.
But what does spicy food have to do with pain? Capsaicin is a molecule found in chili peppers that binds to TRPV1, a type of ion channel that is mostly activated by heat (above 43°C). The binding of capsaicin contained in food to TRPV1 in the oral cavity is felt as a burning sensation, since capsaicin activates the ion channel just as heat does.
Interestingly, some researchers have reported that regular chili pepper consumption can reduce the risk of mortality from a variety of diseases, including cancer, respiratory conditions, and cardiovascular conditions. However, according to this work from Dr. Hong Li and colleagues, chronic spicy food consumption can also increase pain sensation in people.
Since the constant activation of TRPV1 by spicy food and its effect on pain thresholds had not been studied before, these researchers evaluated the effect of sweet, spicy, or tasteless (placebo) gelatin intake in Chinese healthy volunteers. Sweet and spicy gelatin, but not placebo, induced a better emotional state, and also increased cold-pain and pressure thresholds as measured in the hand and forearm, respectively. The heightened thresholds remained even after the taste stimulation was stopped. However, only spicy gelatin consumption for three or more days reduced the cold-pain and pressure thresholds in these subjects, suggesting that a long-term spicy diet can reduce basal pain thresholds in people.
Because of these results, it seems like we Mexicans and many Asian populations are in trouble in terms of pain sensitivity. Chronic consumption of spicy food can make us more sensitive to pain compared to other populations with different diets. Nevertheless, many other factors can also affect pain thresholds. Moreover, even though spicy food is a strong cultural feature in my country, not all Mexican people enjoy it. Such individual differences in one's affinity for spicy food influence basal pain thresholds, and so studying the effect of chronic spicy food intake would become more and more complicated.
The interesting work from Dr. Li and colleagues can be transferred to many other countries to validate these findings in different populations, for the purpose of studying differences in sensitivity to pain. Learning more via such research gives us another way to better understand pain mechanisms as well as develop evidence-based pain management, targeted to the individual, in the future.
Yarim De la Luz-Cuellar, PhD student, Center for Research and Advanced Studies, Mexico City, Mexico.
Always a Bridesmaid, Never the Bride….
When people outside of academia think of research, grand images of breakthrough treatments, drug discoveries, and miracle cures most commonly come to mind. Pop culture even echoes this perspective in fiction novels and on the big screen. Sadly, the spotlight is often given to these types of findings by media publications as well, while less glamorous (although crucial) observational studies fly under the radar. I’m just as guilty, but a study recently published in PLOS One made me think that it’s time to change my ways.
Researchers from the University of Pittsburgh analyzed data from over 21,000 patients who had visited the university’s seven pain management clinics. The patients had completed a battery of validated pain assessments, including a body map to indicate the location of their pain, as part of their visit to the clinic. Although using pain location and distribution in the diagnosis of individuals with chronic pain, this is the first study to apply an algorithm to look at the combined reports from such a large sample of patients. Not only did patterns emerge to delineate nine distinct subgroups based on where pain was distributed in the body, but each subgroup was significantly associated with varying levels of pain intensity and impact. Even more interestingly, the subgroup that patients fell within during their initial visit significantly predicted their pain outcomes at a three-month follow-up visit.
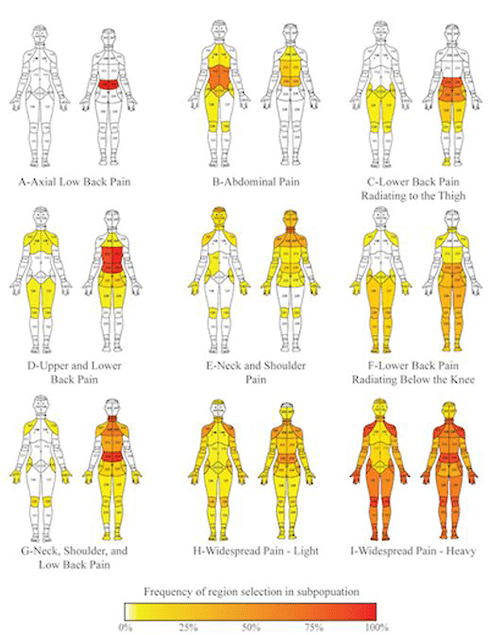
The results from this type of observational study alone won’t cure anyone of their chronic pain. In some ways, these findings generate even more questions to be addressed in future research. However, revealing new relationships regarding how chronic pain presents across individuals makes data from the highly subjective experience appear much less nebulous. Breakthrough treatments, drug discoveries, and miracle cures all rest upon a pillar of understanding. Forming this clearer picture of how chronic pain conditions affect patients strengthens that pillar, making discoveries of mechanisms, targeted treatments, and eventually means of disease prevention all the more possible.
In an earlier post, I expressed my opinion that science needs to be more visible to non-researchers. Too often, the public only becomes aware of our work during the endgame of a protracted battle waged over a career of setbacks and small advances. Perhaps that’s why the zeitgeist is now so easily influenced by misinformation. If the public doesn’t see the incremental advances that only come after setbacks, they’re bound to step in the same bear traps and wander down the same dead ends that researchers had already found themselves at. Celebrating and sharing advances like the observational study above would highlight another aspect of the stringent, empirical process of science. Showing more of what leads up to a breakthrough may make the cures seem a little less miraculous … but it may restore a trust in science that we’re so desperately fighting for.
Joshua Crow, PhD, postdoctoral fellow, University of Florida, US.
Week 4: Monday, August 23, 2021
What If I Could Train My Brain Not to Be in Pain?
Goodbye to the Biopsychosocial Model?
Why Don’t Politicians Listen to Scientists?
A Curious Form of Intractable Pain
Learning About Ancient Indian Medicine for Managing Pain
Exploring the Barriers to Adopting a Biopsychosocial Model in Healthcare Professionals
Pain Education Is Good But Can Be Better
Pain in Autism Spectrum Disorders: Part 2 – Feeling and Describing
Cannabis and Arthritis: Recent Developments
All Aboard! The Pain Education Train Is Leaving!
Self-Medication With NSAIDs in Mexico: The Opioid Epidemic's Little Brother?
What If I Could Train My Brain Not to Be in Pain?
It sounds like a nonsense children's rhyme but in fact, training your brain is one of the hot topics in non-pharmaceutical research for novel treatments, and not only for pain! Research teams around the globe are currently targeting any disorder with a link to brain and mind, from autism to hallucinations and from epilepsy to ADHD. And why wouldn't they be? To train a brain is just a different expression for learning – and if there was a possibility to simply relearn how to not be ill, who wouldn't take that?
I touched on the topic of unmet needs for (pharmaceutical) pain management in my last post, and I want to complement it today with a dive into neurofeedback – basically, training your brain to be in less pain by making the underlying neural processes visible. The most commonly used technologies for making your brain activity visible as a feedback signal is electroencephalography (EEG).
 In practice, picture a person wearing a bathing cap such as the one shown above, with electrodes attached (do not go swimming with these, though) that measure differences in electric potential all over the scalp. Despite how it looks, EEG and other imaging techniques commonly used for neurofeedback are extremely safe, even for children. The signal measured is transferred to a computer and processed in real time into more meaningful feedback, which can be presented as sound, tactile stimulation, or, most often, visually on a monitor.
In practice, picture a person wearing a bathing cap such as the one shown above, with electrodes attached (do not go swimming with these, though) that measure differences in electric potential all over the scalp. Despite how it looks, EEG and other imaging techniques commonly used for neurofeedback are extremely safe, even for children. The signal measured is transferred to a computer and processed in real time into more meaningful feedback, which can be presented as sound, tactile stimulation, or, most often, visually on a monitor.
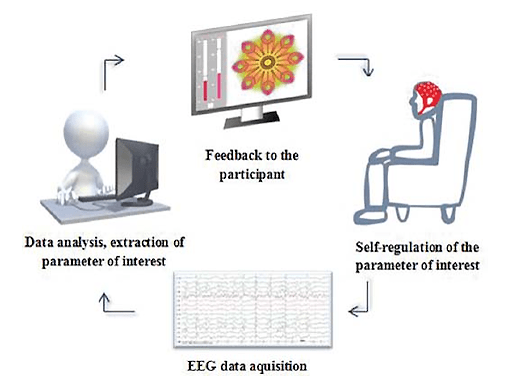
The brain is usually a black box to us. Making its inner workings visible and tangible lets us learn very effectively to manipulate our brain activity in a desired way. In the past, this line of research focused on controlling brain-computer interfaces using thought alone, e.g., to move prosthetic limbs or to fly a drone (check it out on YouTube here) or to try to communicate with locked-in patients (see here). More recently, however, researchers have turned to applying the same principles to mental and brain-mediated health. Pain, for example, is not a mental disorder, but it is constructed in the brain. The source of the pain may lie in the nociceptors scattered across the body, but the quality of hurting is created in the brain. It is also controlled in the brain. We all have powerful mechanisms of pain modulation in our brains, and the hope is to train the brain to use these mechanisms at will.
The latest review of the literature found that neurofeedback reduced pain ratings in 19 of 21 published studies, and although the size of this effect varied dramatically among studies, half of the studies reported clinically significant reductions in pain of more than 30%. The seven studies that followed up on patients after treatment found that symptom reduction remained stable over several months. Given the serious limitations medicine is facing in conventional pain management and the negligible adverse effects of neurofeedback training, this might be a real chance for the field to improve patients' quality of life.
A few caveats at this point: Not all of the studies conducted so far were controlled trials, and most of them do not fulfill the standard of being fully randomized and double-blinded. The controlled trials with the least risk of being biased used fMRI to derive a feedback signal from the brain, a method that is much more expensive and in general not yet as well studied as EEG-based neurofeedback.
To conclude with the very favorite phrase of every researcher – clearly, more research is needed. But in this case, I am actually happy about that conclusion, because my dissertation project focuses in part on implementing an fMRI neurofeedback paradigm for patients suffering from fibromyalgia, complex regional pain syndrome, or depression. I am already intrigued by how different people react to the challenge of regulating the feedback signal – leave a comment if you want to know more! (Beware, though, at the peril of having your ear talked off.)
Malika Renz, PhD student, Central Institute for Mental Health, Mannheim, Germany.
Goodbye to the Biopsychosocial Model?
This may be a bit controversial, but it may be time to move past the biopsychosocial model when it comes to conceptualizing pain.
The biopsychosocial model is widely accepted amongst pain researchers. Within this model, pain cannot simply be reduced to one cause but rather should be thought of as a complex experience, with many overlapping contributing factors. However, despite the improvements over the biomedical model, I argue that the biopsychosocial model has significant limitations in its conceptualization and implementation in clinical practice.
The biopsychosocial model is often portrayed as a Venn diagram (see below), which I think perfectly illustrates the limitations of this model. The three parts of the model are illustrated as being separate, creating artificial boundaries between the domains. In my experiences as a clinician, this fragmentation of the model applies to clinical practice, where patients' pain is reduced to one or two of the domains.
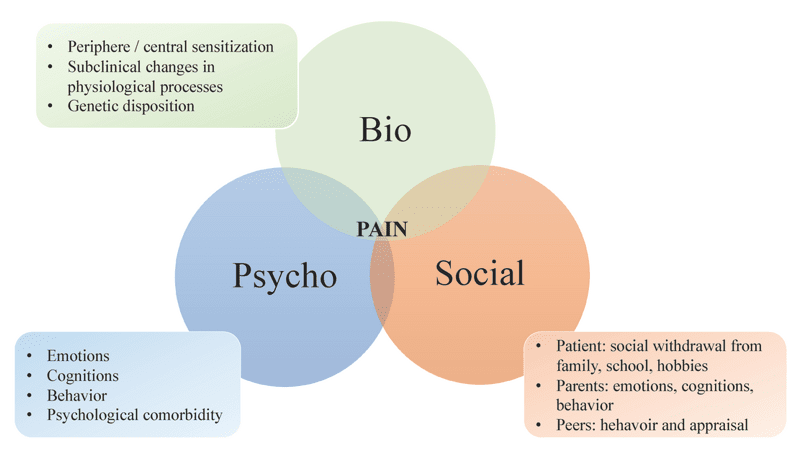
I do want to note that the above is not how the biopsychosocial model was originally conceptualized. However, this is the way it is commonly implemented clinically and in research.
But where do we go from here? A new paper from earlier this year proposes an enactive approach to pain. The enactive model is quite complex (and full of jargon!), so today I’ll just discuss one part of the model: affordances (see note below). Affordances refer to an individual’s range of behavioral choices, or opportunities, given their current environment and bodily state. They rely on the bidirectional relationship between the body and the environment. One commonly used metaphor is thinking about a chair. For most people, a chair is for sitting, and therefore affords sitting. However, for a dog, a chair isn’t for sitting; it might be for chewing or scratching.
But how does this apply to pain?
Let's start with acute pain. Pain relates to danger, or threat, to one’s body, thus changing the way we interact with the environment. If you hurt your knee, walking or bending the knee may be a behavior to be avoided, and stairs may seem steeper than before (your affordances change!). The body becomes a barrier to normal, practiced behavior in the world, leading to reduced interaction with painful movements and thus facilitating tissue healing. Then, as healing and pain reduction occur, one’s affordances also normalize.
Chronic pain is slightly different. Affordances are affected beyond just physical tasks, and there are broad consequences for several affordances – psychological, cultural, relationships, and other normal behaviors such as sleep and exercise. This can lead to disengagement with the environment as a whole. Chronic pain patients also often describe feeling alienated from their body. Thus, chronicity of pain can be seen to change both the relationship with one’s body and with the environment, in a complex and emergent fashion.
If we go back to our chair example, when one is experiencing pain, the affordances experienced differ. Low back pain can make sitting painful; thus, instead of affording sitting, the chair affords a pain experience. Clinically, we may think of the ways we can change affordances. How can we guide someone forward to meaningfully engage with their environment (practice the movement, reassurance about pain not indicating damage)? And how can we change the environmental context to allow for new affordances (a higher chair)?
Overall, I don’t think that there is one perfect model to conceptualize pain. I like how affordances encourage a holistic approach to understanding and treating pain, and focus on how people with pain can better navigate both their own body and the environment around them in terms of action possibilities.
Note: I also want to highlight that this is just one perspective and understanding of enactivism, and is based mainly on the ecological tradition of affordances. There is significant debate about these concepts, which is well beyond the scope of this blog!
Erin MacIntyre, physiotherapist, PhD candidate, University of South Australia.
Why Don’t Politicians Listen to Scientists?
Science, at least when we view it with an idealistic attitude, relies on cold, hard facts. Theories must be backed by evidence, and should more reliable yet contravening evidence come to light, then those theories must be reviewed and amended. In contrast, politics is messier. There is lobbying, differing opinions, scandals, liberal to conservative views, and above all the desire to win the majority vote and remain in power.
In the US in 2020, Donald Trump cut funding for research and development, which dropped by 5.1% (accounting for inflation from 2018 levels) to $134.1 billion, and cut funding to the Department of Energy, the National Science Foundation, and the National Aeronautics and Space Administration. The only federal agency to receive a significant increase in funding (at +13.5% from 2018 levels) under the Trump administration was the Department of Defense – make of that what you will.
Contrastingly, President Biden launched his ultimately successful campaign with "Listen to science," promising to enlist science and scientists to tackle the pandemic, the economy, climate change, and technology and industry within the US. Although there are, of course, many factors as to why Biden won his presidential race against Trump, his trust in science was undoubtably a contributing element in winning the popular vote – therefore, the voting public must also have faith in the scientific process and community?
Here in the UK, amongst the many startling changes the COVID-19 pandemic brought was the daily appearance, on our TV screens, of scientists who were regularly given more airtime than the politicians of the day. The government vowed to make policy only "on the basis of a rigorous analysis of the evidence," but it wasn’t before long that different countries, based upon the same science, were making radically different policies concerning isolation time, social distancing, testing, and lockdowns. What is now known in hindsight is that the Scientific Advisory Group for Emergencies (SAGE) had been advising the UK government on social distancing measures, shielding, and scaling up of mass-testing capacity since early March 2020, yet, consistently, policy did not follow this advice, or at best followed it with considerable delay, with consequential rises in case numbers and fatalities. So once again, politicians and their policies chose to ignore the scientists.
This is not the first time that the UK government has ignored recommendations given by their scientific advisors. In 2009, Professor David Nutt compared the risk of injury when horse-riding with the considerably lower risk of taking recreational cannabis. He further suggested, as was his role as chair of the Advisory Council on the Misuse of Drugs (ACMD), that the classification of recreational drugs in the UK should be based on evidence of the actual harm that the drugs cause. As a result, Nutt was dismissed from the ACMD, and cannabis remains a Class B drug in the UK, equivalent to that of amphetamine.
So the public listens to and trusts science. Science trusts facts and evidence. Scientists provide sound advice. And politicians? They want the vote.
Alice Gregorie, PhD student, University of Leeds, UK.
A Curious Form of Intractable Pain
It’s late summer, 2021. Josie is catching up with her husband and putting together dinner with her family, all while dealing with a nagging headache that started on the way home …
… in July of 2018.
At the moment, it’s nothing debilitating. Most days, she describes her headache as being “noticeable, but annoying, kind of like a shirt collar that’s just a little too tight.” On a bad day, she ends up in the emergency room with headache pain so excruciating that it causes her to vomit. Josie has new daily persistent headache (NDPH), a malady that is an untreatable, consistent headache that lasts from three months to 27 years. She reached out to me through a post I shared from work linking long-term COVID-19 to chronic pain conditions. The media article pointed out the potential for viral infections to trigger intractable pain (pain that cannot be alleviated through treatment). “… it gives me a ton of hope knowing that maybe COVID-related research could help folks like me,” according to Josie.
Josie remembers the exact day that her headache began, a strange characteristic of many people suffering from NDPH. She developed a mild headache on the way back home from a holiday weekend with family in the summer of 2018. She initially passed it off as the beginning of a head cold, but despite some rest and over-the-counter pain meds, the pain escalated. By the next morning, she knew that something was not right, but Josie had no way of knowing that she would battle that same headache every day for the next three years.
Emergency room doctors and specialists couldn’t explain Josie’s condition, writing her reported pain off as everything from migraines to drug-seeking visits to the ER. In an attempt to escape headaches that only subsided when she slept, Josie removed proinflammatory foods from her diet, avoided activities that raised her blood pressure, sought out comfort in online communities made up of those with NDPH, and even found a month-long reprieve following an occipital nerve block.
But the symptoms eventually came raging back. Eventually, following a second lumbar puncture (which resulted in a painful cerebrospinal fluid leak), doctors determined that the original headache and neck pain likely came from a human parvovirus infection … but that did little to explain why the headaches have persisted. The symptoms of human parvovirus typically subside in one to two weeks. Like others battling NDPH, Josie is left to mitigate her symptoms through a combination of dietary and behavioral accommodations. She still spends the occasional day home from work, shielded from light and noise, and suffering through debilitating pain.
Although NDPH broke into the medical literature in the 1980s, sequelae following a flu outbreak in the late 1800s strangely mirrors hallmark signs and symptoms of NDPH. Today, more than 30% of NDPH patients can trace onset of symptoms to a non-related viral infection. As COVID-19 continues its march across the global population, physicians’ quest for the solution to NDPH is renewed. For Josie’s sake, and those like her, I hope a better understanding is just over the horizon.
Joshua Crow, PhD, postdoctoral fellow, University of Florida, US.
In the search for a catchy title for this post, I checked to make sure that the one I chose was not already taken. What does this title mean, and what is this post about? Just continue being intrigued. Pain is a hot topic for researchers and of coursealso for ageneral audience.
Pain science includes neurology, immunology, endocrinology, epigenetics, psychology, physiology, and other areas. Integrating these multiple fields of research is helping to clarify the mechanisms underlying pain.
But whose pain are we studying, exactly?
Worried that female hormone cycles would complicate results, many pain scientists have deliberately excluded female subjects from their studies. Others stuck with males because that is how things were always done. Therefore, data acquisition was designed and conducted for males, both for rodent and human subjects. It has always been about male pain.
In 2007, Jeffrey Mogil of McGill University and his colleagues noticed that male mice showed different pain behaviors depending on the scientists present during the experiment. To investigate whether it was the sight or smell of a human that caused the effect, the researchers acquired a promotional cardboard cutout of the ubiquitous Ms. Paris Hilton. Yes, Paris Hilton. They found that the cardboard cutout had a painkilling effect in mice, and that this Paris-mediated analgesia appeared to be gender specific. Male mice spent less time licking their wounds when “she” was in sight, but females showed no such effect. Also, male mice, but not females, had lower constitutive expression of a gene called c-Fos in a part of the spinal cord that transmits nociceptive signals to the brain, suggesting reduced neural activity in this pain pathway.
In vitro and ex vivo models of nociceptive transmission, and behavioral research on male samples and subjects, have unveiled aspects of the physiology of pain, and have had implications for clinical practice. But how much knowledge have we failed to generate because of the focus on males?
Sex differences in the pain pathway can be found at all levels of the neuraxis, from receptors in peripheral neurons, to the spinal cord, and to the subcortical structures and cortex of the brain. As recently reviewed by Mogil, the pain genetic landscape of the sexes is certainly different, and it comes as no surprise that several proteins participating in pain-related neural circuits have been found to play sex-dependent roles. The influence of sex hormones represents a significant source of pain-related variability that likely impacts men and women differently. Sex-related differences in pain may also reflect differences in the endogenous opioid system. There is also evidence suggesting sex-related cortical differences during the processing of pain-related stimuli, potentially implicating the influence of sex hormones on differential brain activation.
Unfortunately, much of the research in the pain field still suffers from the methodological limitation described above. However, performing experiments in both sexes is not only ethically correct but also the scientifically right thing to do.
Federica Franciosa, PhD student, University of Bern, Switzerland.
Learning About Ancient Indian Medicine for Managing Pain
Over the past decade there has been growing interest in nonconventional or alternative approaches for pain management such as yoga, acupuncture, and herbal therapies, to name a few. Historically, these approaches are derived from an ancient medical system called Ayurveda (sounds like ai·yr·vay·duh), which originated from the subcontinent of India.
To understand more about this medical system and the benefits it may have for pain patients, I sought the expertise of Dr. Amala Guha from the University of Connecticut. Dr. Guha is a trained research scientist in the field of immunology, with a master’s degree in public health, and has clinical training from Ayurvedic schools of medicine in India.
For background, the word Ayurveda comes from the classic south Asian language Sanskrit, which combines the word “Ayuh,” which means life, and “Veda,” which means knowledge. The word Ayurveda can be translated as the “science of life” or “wisdom of life.” As a school of medicine, Ayurveda contains two arms. The first focuses on the use of alternative approaches for therapeutic management of disease symptoms and is referred to as Ayurvedic Medicine. The second arm focuses on supporting healthy living for healthy individuals. For instance, individuals may practice preventative Ayurveda to support good mental and physical health by meditating, doing yoga, and maintaining good hygiene.
“According to Ayurveda, pain is a big factor in all lives and conditions. As there are various types of pain, no single approach is applicable to all. Ayurveda customizes medical approaches according to each patient and their needs (individualized medicine).” – Amala Guha
Trained physicians in Ayurveda therefore customize palliative and preventative care based on the needs of the individual. Compared to Western medicine, which is progressing towards personalized medicine, Ayurveda has been individually treating patients since 1000 BCE. That being said, obtaining proper training in Ayurveda and Ayurvedic Medicine is currently not possible in the United States. This is due to a lack of accredited Ayurveda medical school programs, and, like Western medical school programs, becoming a trained physician in Ayurveda requires several years of training from an accredited institution, most of which exist in India. This is not to say that Western-trained physicians cannot learn Ayurveda, but they would need to attend additional training from an accredited Ayurveda school of medicine and obtain a proper license before being able to practice Ayurveda.
Similar to Western medicine with regard to drug doses and the risk of adverse side effects, any biologically active substances such as spices and herbs (e.g., turmeric) with known medicinal properties (e.g., anti-inflammatory) warrant caution when being added to one’s diet. Thus, taking a therapeutic dose of an herb can cause adverse reactions and a possible trip to the emergency room if consumed haphazardly. The same can be said about practicing yoga without proper instruction and increasing your risk for an injury.
In summary, when seeking medical advice for alternative methods, take care to inquire about the credentials and training of the clinician or medical care provider you have chosen. Hopefully, as more individuals show interest in alternative approaches, the availability of trained professionals will also increase, therefore allowing more opportunity for patients to incorporate these strategies into their therapeutic regimens for managing pain symptoms. In you are interested in learning more, please visit Dr. Guha’s website.
Britt Knight, postdoctoral trainee, University of Connecticut, US.
Exploring the Barriers to Adopting a Biopsychosocial Model in Healthcare Professionals
George Engel proposed the biopsychosocial model for healthcare in 1977 (see here) but it seems that even after more than 40 years, we (healthcare professionals) are still struggling with implementing this model in modern healthcare. In this blog post, I’d like to highlight some of the key points made by Ng and colleagues in this recent paper from PAIN. This was a systematic review and meta-analysis of 25 articles looking at the barriers and enablers influencing healthcare professionals in adapting a biopsychosocial approach to musculoskeletal (MSK) pain. The authors used a qualitative approach to synthesize the evidence, and three major themes emerged.
The first theme examined the knowledge and skills of healthcare practitioners. Some of the barriers identified included: a lack of communication, interpersonal, and counseling skills when dealing with sensitive topics; difficulty integrating clinical explanations with a broader biopsychosocial framework that made sense to patients; a lack of skill in managing patients’ concerns, beliefs, expectations, emotions, and reactions; and being unaware of other treatment options and lacking clarity on when and where to refer patients. Healthcare professionals also felt frustrated, uncomfortable, insecure, and embarrassed to ask about psychosocial factors.
For MSK practitioners, it’s understandable how asking questions about depression, anxiety, trauma (physical, sexual, emotional), adverse childhood events, and social determinants of health might make one feel uncomfortable (this applies both to the practitioner and to the patient), but we need to remember that we’re not just treating a “low back” (or insert whatever anatomical structure); we’re treating a complex human being with past experiences, beliefs, worries, fears, emotions, and anything else you can think of that makes someone human.
It’s also understandable that we (MSK clinicians) don’t feel that we have the knowledge or skills to deal with psychosocial factors, so we shy away from asking. Maybe we can’t do much depending on what our clinical training and scope of practice allows, but we do know that there’s a relationship between psychosocial factors and chronic pain, and how important these factors are in the prognosis for a person. We can use this information to educate patients while doing our best to address modifiable lifestyle factors like sleep, physical activity, nutrition, and stress. These types of low-hanging fruit involve behavior change, and if you have ever tried to make a lifestyle change, you know that it’s much easier said than done. But that doesn’t mean we shouldn’t try. Consider referring to healthcare colleagues that can help such as a psychotherapist, social worker, fitness trainer/coach, dietician, or nutritionist.
But it doesn’t just end there. We also need to consider other barriers such as patient willingness, healthcare insurance coverage, community access, language barriers, and other sociocultural factors. These factors (funding models, workforce training, health policy, organizational and social factors), which relate to the second and third major themes of the paper, are just as important as the first theme.
As you can see, it’s going to take a whole team of people at different levels of the healthcare system to embrace Engel’s 40-year-old vision for healthcare. But individually, it always starts with you. So although it may feel overwhelming or even terrifying to embrace a biopsychosocial model when you were taught in a biomedical model, know that a good place to start is to just take a step back and listen to the human being in front of you.
Derick Luu, chiropractor, master’s student, School of Rehabilitation Science, McMaster University, Hamilton, Canada.
Pain Education Is Good But Can Be Better
In 2018, an international group of researchers published three articles about low back pain in The Lancet. The authors created a list of commonly available interventions with their respective recommendations. The recommendations depend on the level of evidence stratified by pain duration (acute or chronic) and the clinical course of the condition (getting better or getting worse). Patient education is considered the first-line treatment for acute and chronic low back pain.
Pain education is good …
Patient education assumes that patients are not passive recipients of the information. Imagining that rehabilitation is a journey from the “city of pain” to the “city of well-being,” we might think of education as more like a bicycle than a car that helps patients reach their destinations. Researchers have shown that the “patient education bicycle” is effective and affordable to transport patients with low back pain closer to the “city of well-being.”
Patient education, as well as bicycles, is relatively old and has evolved over the years. Patient education was centered on the anatomy of the spine and the prescription of movements to protect the back. Over time, researchers learned that the protection of the back does not help people with low back pain. In fact, the focus on the “right” posture to do natural movements is associated with more worries and functional limitations.
Researchers have investigated other educational strategies consistent with the current evidence for low back pain. Today, patient education involves teaching people about biopsychosocial factors associated with low back pain. Modern patient education includes strategic content to decrease back pain misconceptions (pain resulting from an injury) and worries (low back pain always gets worse and never gets better), and increase confidence in patients' ability to keep active despite the pain. There are excellent educational materials clinicians should consider using in their clinical interactions (e.g., The Back Book and Explain Pain. Studies have shown that modern patient education programs can improve psychosocial factors in patients with low back pain. Particularly for chronic low back pain, patient education can even reduce pain intensity and disability.
… but it can be better
Although pain education reduces disability for chronic low back pain, the intervention alone only improves some psychosocial factors in acutelow back pain. However, recent research suggests that the limitations of pain education for acute low back pain are temporary. The authors suggest that some adjustments in the current pain education approaches would increase their efficacy and reduce disability.
In a study published last week in the Journal of Pain, the authors used a method (causal mediation analysis) to understand how changes in some psychosocial factors affect disability. This method assessed the extent to which the intervention affected psychosocial factors proposed to change disability. In addition, the statistical technique estimated which psychosocial factor would cause the most substantial change in an outcome if it was successfully targeted by the treatment. The study investigated the influence of three common psychosocial factors for low back pain: 1) positive beliefs about the consequences of back pain (back beliefs); 2) exaggerated negative thoughts about back pain (pain catastrophizing); 3) patients' confidence in accomplishing functional tasks despite the pain (self-efficacy).
The authors showed that it is possible to reduce disability through all those proposed mechanisms investigated in the study. However, self-efficacy was the psychosocial factor that would cause the most substantial reduction in disability. That explains a lot about why pain education did not cause meaningful changes in disability; in this trial, pain education changed all these psychosocial factors a little bit except self-efficacy.
Implication
We need to review the content of pain education for acute low back pain to target self-efficacy and, perhaps, improve function with the intervention.
Pain education is good but can be better. Twitter: @rodrizzo_pain.
Rodrigo Rizzo, doctoral candidate, Neuroscience Research Australia (NeuRA) and the University of New South Wales (UNSW).
Pain Neuroscience Education: Identifying Patients Who Need It, and Using It as an Adjunct to Movement and Exercise, Not as a Standalone Treatment
Pain is a complex phenomenon. It is an essential and normal human experience, but when pain persists it can become maladaptive. Our perception of pain is influenced by many factors, including our thoughts, our beliefs, and our understanding of pain. These factors contribute to pain as a biopsychosocial phenomenon. That is to say, pain is much more than just tissue injury; it also has psychological and social influences. Thus, for every pain patient there is a variety of factors that have an impact on pain, function, and overall health.
When I was a practicing physical therapist, I would spend time answering my clients' questions about their pain, and providing them with information about their current pain problem and its impact on their overall health. I also aimed to eliminate some of their fear/stigma about something they may have seen on the Internet or heard from their friends. My big-picture goal was to create a lasting change in patients' beliefs about pain, and in turn increase their engagement in the behavioral change recommendations aimed at reducing their pain. Thus, pain education addresses patient misconceptions about pain processes and helps shift their perspective to the idea that pain is influenced by biological, psychological, and social processes.
One common pain education approach is pain neuroscience education (PNE), which is commonly used by physical therapists and other health professionals. PNE aims to help patients understand their pain from a biological and physiological perspective. It helps them experience less pain and disability by utilizing a range of educational interventions, with the underlying goal of reconceptualizing what pain is. Reconceptualizing pain as a protective response to a real or perceived threat, rather than as a marker of tissue damage, allows for fear reduction and improved participation in movement/exercise.
PNE can be implemented in many ways. During the initial evaluation, one of the many important components includes allowing patients to tell their pain story instead of simply using a checklist or intake form. This may seem less efficient, but it can provide important information about the client's understanding of their pain, which leads to more effective educational interventions. Several studies utilizing PNE for patients with musculoskeletal pain have demonstrated decreases in pain and fear avoidance, changes in patients’ perception of their pain, improvements in patients’ attitudes about pain, and increases in physical performance.
Two things that have recently gained a lot of attention among physical therapists using PNE is that not all patients with pain are candidates for PNE, and that PNE should be used as an adjunct to movement and exercise rather than as a standalone treatment. Louw et al., in their Viewpoint, strongly argue that PNE was created to complement other multimodal approaches within a biopsychosocial framework, and that it should not be the focus of treatment. Rather, it should be used to effect changes in beliefs and attitudes about pain and improve delivery of evidence-based interventions. It is also critical that physical therapists be experienced enough to recognize who is a good candidate for this intervention. Patients need to be interested in learning more about pain, and open to new narratives. Patients with chronic pain, widespread pain, sensitization, fear and catastrophizing, and kinesiophobia (fear of movement) are good candidates.
As PTs, we must address chronic pain using a multimodal approach focused on movement, exercise, and patient education approaches like PNE to improve the overall health of our patients.
Bhushan Thakkar, PhD student, Department of Physical Therapy, Virginia Commonwealth University, US.
Pain in Autism Spectrum Disorders: Part 2 – Feeling and Describing
“Knowing what we feel is the first step to knowing why we feel that way. If we are aware of the constant changes in our inner and outer environment, we can mobilise to manage them.”
– Bessel van der Kolk, from his book The Body Keeps the Score (2014)
Pain differs from simple sensation, as it is also an emotional experience. In addition to sensory processing difficulties, emotional regulation, socialization, and communication differences in autism spectrum disorders (ASDs) can also alter the pain experience.
The above quote describes how a disconnect from knowing what we’re feeling prevents us from being able to cope with changes. These changes could be a sudden change in sound or light, abdominal pain arising from hunger, or a change of emotion or arousal. Problems in identifying, understanding, and describing one’s own emotions is known as alexithymia and occurs in a high proportion of those with ASD.
The term alexithymia was coined in the 1970s as an observed characteristic of psychosomatic illnesses – where psychological factors cause or aggravate physical symptoms. There is a commonly held notion that if something is psychosomatic, it is "all in the head" and therefore "not real," as if the mind or emotions are just some fictitious curiosity. However, what we experience is very real, whether it has a corresponding biomarker or not. All pain has a psychological component and is therefore liable to alteration by emotional states. So how is pain experienced by those who find it hard to understand their emotional state?
In patients with fibromyalgia, those who had alexithymia reported higher pain intensity and psychological distress than non-alexithymic patients. Similarly, in a study of chronic neuromuscular pain, those who scored higher in alexithymia measures reported higher pain intensity and worse psychological and physical functioning due to their pain. It may be that this impaired emotional awareness promotes a hypervigilance for bodily sensations including discomfort and pain. Pain might also be inadequately managed in those with alexithymia, because if you don’t know what you’re feeling, you can’t effectively attend to your needs, self-soothe, or ask for help from others.
Emotional regulation refers to the ability to respond to a range of emotions in a flexible and socially acceptable way. This is a socio-cognitive endeavor that requires re-evaluation of an emotional situation to modify its impact. This re-evaluation and processing of emotional signals is disrupted in individuals with ASD, including those with "high-functioning" autism. Only once nociceptive signals reach the brain can that pain be experienced. Emotional regulation can have a direct effect on that pain experience, especially through reappraisal and suppression techniques, and an impairment in this regulation might lead to heightened or longer-lasting pain.
Diagnostic criteria often highlight social deficits as a central component of ASD, perhaps because these deviate the most visibly from societal norms. This describes behavior such as reduced eye contact, difficulty initiating or maintaining conversations, and pedantic or unusual speech patterns. As a result of "atypical" communication styles and a reduced willingness for neurotypical people to engage with them, people with ASD can struggle to make friends.
Social support can improve physical as well as social pain (e.g., of rejection), but this may not be as available to those with ASD, who report higher levels of loneliness, anxiety, and depression. Neurochemical investigations of the social deficits, and an apparent "pain tolerability" in autism, have focused largely on a potential imbalance of the body’s opioid system, though inconsistencies and variability of these studies mean that this area requires further investigation.
Pain is a complex experience that can be dissected and studied from several different angles. The same can be said for ASD, which involves a range of differences in emotion, sensory processing, social interaction, and communication styles that can all interact with how pain is experienced. It is therefore important to understand the nuances when different groups of people experience or communicate their pain so that we can be as inclusive as possible in research as well as in diagnosis and treatment.
If you would like to continue this conversation, feel free to contact me by email (sofia.fontana-giusti@reading.ac.uk) or via twitter, @sofia_fg_9.
Sofia Fontana-Giusti, research assistant, University of Reading, UK.
Cannabis and Arthritis: Recent Developments
The persistent challenges related to chronic pain management, as well as the continued alarm regarding the opioid epidemic, are driving patients and healthcare providers to search for safer and effective alternatives to opioids to treat chronic pain. One of these alternatives that has made waves in the media is medical cannabis.
The idea of a non-addictive, safe method of pain alleviation sounds very appealing, doesn’t it? However, it is important to note that there are more forces marketing medical cannabis to the masses than there are clinical studies investigating the benefits for chronic pain patients. In fact, the FDA has only approved medical cannabis as a treatment for epilepsy. One reason for this is that the route of administration plays a big role in the effectiveness of cannabis in treating pain, and that methods to measure inhaled substances with precision and consistency are limited.
So where does that leave us? Well, animal studies are ramping up, with more research teams focusing on specific chronic pain syndromes, such as arthritis. Cannabis is composed of over a hundred different cannabinoids. The two main phytocannabinoids are tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is the psychoactive or “euphoric” component of cannabis, while CBD is a non-psychoactive component of the plant. In a recent animal study, the pain-alleviating effects of these two components were investigated in the context of chronic inflammatory pain. THC successfully reduced the pain response of rats, while minimal effects were observed when CBD was administered.
In addition to pain relief, the effect of a drug on the immune system is important to investigate, as it can help predict the progression of an inflammatory disease. The ideal drug would decrease or soothe the immune system’s activity. THC generated no change in immune response, while CBD was accompanied by increased levels of some of the immune components studied.
There are well-documented differences in pain incidence, prevalence, and experience between men and women. However, these differences are not well described in the context of pain alleviation via medical cannabis. A recent study found that male and female rats reacted similarly to THC and CBD, both in terms of pain alleviation and immune changes.
Valérie’s Book Club:
Do you want to read more about how science communication can impact knowledge and discoveries? Join my book club! Every week, I will be recommending a book that illustrates how collaborations between patients and scientists can make immense contributions to the advancement of science and medicine.
This week’s recommendation is Darkness Visible: A Memoir of Madness by William Styron (1992). As pain scientists, we spend years studying the best methods to assess pain in human patients, and to replicate pain behaviors in animal models. A lot of this time is spent critiquing our current methods, which are simplistic and maybe unreliable in certain populations. Yet we always circle back to those same old methods because they are established. Why does this happen? It is because physical pain, like psychological pain, is a unique individual experience that is hard to describe. The best written description of pain that I have ever read has come from this book. The author describes the continuum between physical and psychological pain based on his experiences, and even Styron, a prolific writer, is at a loss for words when the pain is at its worst. This is a very moving account of the pain experience, and I really recommend it to our PRF readers!
Valérie Bourassa, PhD candidate, McGill University, Montreal, Canada.
All Aboard! The Pain Education Train Is Leaving!
Pain education has become an important and prominent aspect of physiotherapy undergraduate training. However, in my experience, it might be lagging in the training of other healthcare professionals (HCPs). Although I am writing from a South African perspective, training in adequate assessment and effective management of pain has been reported to be undervalued and insufficient in undergraduate HCP training all over the world (Spain, Australia and New Zealand, Canada, Norway, North America, and Europe).
Disparities in pain management training amongst different HCPs may be a barrier to implementing holistic patient-centered care. Conflicting "pain language" can be harmful; we (HCPs) need to speak the same language. However, for HCPs to be able to "speak the same language," we all need to have foundational pain neuroscience knowledge.
Postgraduate pain training is becoming increasingly available, which is very encouraging! However, efforts to implement training in pain for undergraduates have been much more sluggish. Through my experience teaching for a postgraduate diploma in pain management at University of Cape Town, I have seen many qualified HCPs struggle with their pain philosophies being so fundamentally challenged; it is often a huge paradigm shift for them. I applaud them for taking on the challenge. But why do we need to wait until after students are qualified HCPs to provide them with the vital knowledge and skills to assess and manage different types of pain effectively? Let’s avoid putting future HCP graduates through this massive paradigm shift. We need improved efforts for laying down the essential foundational pain neuroscience knowledge at an undergraduate level, for all healthcare disciplines alike. We should all follow physio’s lead and plant the seed in undergraduates for it to flourish at a postgraduate level.
Gill Bedwell, PhD candidate, University of Cape Town, South Africa.
Self-Medication With NSAIDs in Mexico: The Opioid Epidemic's Little Brother?
Opioids are strong painkillers mainly used for severe, short-term pain or for terminal painful illnesses such as cancer. Nevertheless, the opioid misuse and overdose epidemic is a serious public health issue in the US, with both prescribed and illegal opioids causing thousands of deaths.
Except for our northern region, access to opioids and their distribution for pain treatment are very limited in Mexico. Due to a lack of pain specialists and unsuitable pain management in hospitals, Mexican people actually do not know how to treat pain, and drugstores prefer not to sell opioids even though these drugs have been approved since 2015 for cancer pain patients and palliative care.
But it seems that we Mexicans insist on having our own self-medication epidemic with another type of analgesic: the non-steroidal anti-inflammatory drugs (NSAIDs).
NSAIDs may not be causing respiratory depression or a marked physical dependence like opioids do, but the abuse of these apparently safe drugs can lead to short- and long-term, severe adverse effects. NSAIDs are drugs that block the action of the cyclooxygenases (COX), a group of enzymes that modulate inflammation, fever, and pain. However, COX enzymes are also responsible for protecting the gastrointestinal tissue, regulating blood pressure, and controlling renal processes. Therefore, misuse and overdose of NSAIDs can disturb many physiological systems by interrupting COX functions.
According to a local study, the NSAIDs that cause the most adverse effects in the Mexican population are metamizole, ketorolac, diclofenac, and acetaminophen. The last is not an NSAID due to its lack of anti-inflammatory effects, but it was included in the investigation as it is a drug widely used for the treatment of mild pain. More than 60% of adverse reactions were well tolerated and did not require medical attention but, in some cases, unwanted effects of NSAIDs extended to gastrointestinal bleeding, renal failure, heart attack, and cerebral stroke.
Self-medication is widely accepted, as it prevents wasting the time and money required for medical care and health insurance, a service unreachable for most people in my country. Even though pain is the most common reason for visiting a doctor, some pain is easy to identify (such as headache or menstrual pain), is not severe, and is often managed at home with self-prescribed analgesics. Thus, people prefer to follow recommendations from others, who assure them that they found pain relief with over-the-counter analgesics. But sometimes people consume leftover painkillers from past treatments to avoid spending money on new ones, leaving aside any proper dose regimen, and probably masking a more serious disease that really needs medical supervision.
At first, I considered self-medication with NSAIDs a public health problem for low-income countries with no access to appropriate pain management. But, given the reach of the opioid epidemic in high-income countries, it looks like pain treatment is a problem that goes beyond the economy. Therefore, the poor understanding of different kinds of pain and the lack of public awareness about the use of analgesics turn any self-consumption of painkillers into a potential epidemic, everywhere and anytime. Right now, I am very grateful for the low availability of opioids in Mexico.
Opioids and NSAIDs are effective and safe when administered at appropriate doses, for brief periods, and under medical supervision. It is urgent to improve access to analgesics while introducing public guidelines for restricted usage and dosage, along with investment in a better understanding of pain pathologies and the development of safer pain therapies.
Yarim De la Luz-Cuellar, PhD student, Center for Research and Advanced Studies, Mexico City, Mexico.
Week 3: Tuesday, August 17, 2021
A Knowledge Translation Campaign to Reduce Imaging for Low Back Pain
In Search of the Runner's High
How Do Pain Patients Feel About CBD?
Graded Motor Imagery: Training the Brain as a Treatment for CRPS
“Keep Swimming”: Did Dory Read the Clinical Practice Guidelines for Low Back Pain?
Pain in Autism Spectrum Disorders, Part 1: Sense and Sensitivity
Women and Pain, Part 2: No, Your Patient is Not “Emotional”
“Participants in Pain Studies Are More Than Just WEIRD….”
Do We Still Need Animals for Pain Research?
What Is Central Sensitization?
A Knowledge Translation Campaign to Reduce Imaging for Low Back Pain
One of the reasons why I chose a career in pain research is to help translate research into clinical practice. As I discussed in my first blog post, there is a massive gap (17 years!) between scientific consensus and changes in clinical practice. One example of this is imaging for low back pain. As a rare example of scientific consensus, routine imaging is no longer recommended in the majority of low back pain cases (see this study for a recent review). Imaging is not needed to guide diagnosis or treatment, and there is a growing recognition of the harms that imaging can cause.
One way to bridge the gulf between research and public opinion is a public health campaign, and a recent study tested this theory, surveying patients' responses to a new public health campaign aimed at reducing the use of imaging for low back pain. The campaign consisted of posters with messages like “Back scans can lead to dangerous and unnecessary treatments” and “Back scans can’t heal – they can harm.” Spoiler alert: The campaign did not go over well.
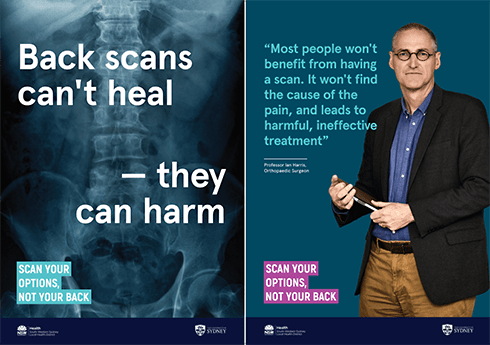
In true COVID-era fashion, participants doubted that the information was true and mistrusted the source of the information. For instance, one participant said:
“If I walked into a hospital like that I’d turn around and walk straight back out again, sorry. It’s like, if this is what these people actually believe then I’m out of here because that’s ridiculous; they’re just scaring people to get rid of people.”
They were skeptical about the reasons behind the campaign, with some participants expressing that it may be a way for the government to reduce healthcare spending.
It wasn’t all negative. Participants were interested in learning more about the topic. They also thought that the campaign would lead to good conversations with health professionals. Interestingly, there was also a theme about trusting their clinician over public health messages, indicating that this may be a more effective means to change public opinion on the topic. For example:
“I would look at these posters walking in the hospital and think, oh god, roll my eyes, have a chuckle at it, and ignore them. I would rely on my GP; I would go to my trusted GP and my experience is mainly with my mum having as many scans as she did have done.”
The results of this study are both surprising and exactly what I expected. As a clinician, I have known about the harms of overdiagnosis for years. Over the same timeframe, I’ve also had similar conversations, not only with patients but with friends and family. Given the prevailing biomedical model of pain, which explains pain in terms of tissue damage, it is no surprise that people believe that scans are useful for back pain. And given the current climate of mistrust of authority, it makes sense that people would be skeptical about the motivations behind such an initiative.
While this public campaign didn’t have the anticipated result, it does give us clues as to how we can begin to make a difference in this important issue. The authors suggest that future campaigns could use more positive messaging. There could also be a focus on educating clinicians about the dangers of inappropriate imaging, and effecting change during individual clinical interactions.
Image credit: Sharma et al. Health Expectations. 2021;24:648-658.
Erin MacIntyre, physiotherapist, PhD candidate, University of South Australia.
In Search of the Runner's High
A major function of pain is that it hinders us; it slows us down and forces us to protect the injured part of the body and give it the time it needs to heal. However, as any keen long-distance runner will attest to, the logical advice to not run through the pain and take a few days off is one of the hardest to follow. I count long-distance running (half-marathons; I’m yet to conquer a full one) as one of my hobbies, but why do runners continue to push themselves beyond the point of "normal" exercise pain, and even use the pain to spur them on?
Some may suggest the "runner’s high" to be the culprit. This is the nirvana-like state that runners quite literally chase after – a feeling of mental well-being and elation, reduced stress, and even a noticeable lack of the ability to feel pain. Although not fully understood, the release of endorphins by the body is thought to cause this effect – the prefix "endo" meaning "within" and "orphin" being a contraction of morphine, i.e., the body’s own natural opioids. More recently, endocannabinoids (namely, one called anandamide) – substances similar to those found in cannabis – have also been implicated, as these were found at higher levels within the body tissues of mice that had been subjected to extended periods of wheel running compared with those that had not. Both endorphins and endocannabinoids are widely known to induce states of euphoria as well as analgesia (pain relief), which fits with the sought-after characteristics of the runner’s high.
Whatever the biomechanism, could the pain-relieving effect and euphoric rush of the runner’s high underlie long-distance runners' perseverance no matter what?
Blame has also been placed at the door of the long-distance runner mindset – the thinking that pushing yourself toward your time and distance goals must hurt, and pain means that you are achieving these goals. Running, at times, is inherently painful, and the more you push your body the more it is going to hurt. Some sports psychologists even go to the point of promoting methods of raising a runner’s pain tolerance in order to push a runner faster and farther.
Perhaps what is most likely is a combination of the two factors: the sheer stubbornness of a runner combined with the body’s own incredible pain-relieving abilities. Perhaps the greatest mystery to most of the population is the fact that other people run at all. After all, there’s been no predator chasing us for the last millennium or two.
Alice Gregorie, PhD student, University of Leeds, UK.
How Do Pain Patients Feel About CBD?
Cannabis is the most commonly used illegal substance in the world. In the United States cannabis remains a Schedule I drug. However, over the past 15 years the number of state legalizations for medical cannabis has steadily increased. As of 2020, more than 35 states and four territories have legalized medical cannabis for childhood epilepsy, chronic pain, as well as anxiety disorders.
Medical cannabis refers to the use of cannabis/marijuana or components of the cannabis plant such as cannabidiol, also known as CBD, for managing symptoms related to medical conditions. CBD is one of more than 100 molecules identified in the cannabis plant. CBD, compared to marijuana, is not a scheduled substance.
The increasing popularity of CBD products, as well as social media content regarding the perceived health benefits, has contributed to public interest in CBD and cannabis-related products. Additionally, the scientific community has also shown increasing interest in understanding the health benefits of these substances. While this has led to an increase in the number of scientific investigations, there is much more knowledge yet to be gained.
One thing that has become clear is that medical cannabis is increasingly being used by patients to treat pain. This led to a recent publication out of the Moeller-Bertram Lab from Vitamed Research that aimed to identify the attitudes among pain patients about the use of medical cannabis.
The authors created a survey for individuals who attend pain clinics to report their level of knowledge of CBD-related products and their perceptions of the health benefits of these products for managing pain. The data include results from 253 participants, of whom about 152 (60%) reported prior use of CBD products.
Demographic information revealed that about half of the participants included in the study identified as being white (56%) or non-Hispanic (51%). In addition, nearly 37% reported that they had difficulty working due to disability, and 5.1% reported having served in the US armed forces.
When asked about their awareness of CBD products, nearly 80% of participants reported knowing someone who had previously used these substances, and 80% of participants reported that somebody they knew (neighbor, family, friend) had suggested to them that they use CBD, whereas the remaining participants reported that their “treating providers” had suggested CBD for their pain management.
Questions pertaining to the effectiveness of CBD products revealed that 60% of participants reported beneficial outcomes for managing back pain, nerve pain, and neck pain. Furthermore, nearly half of all participants reported that using CBD products reduced the number of opioid medications they needed for managing their symptoms.
Interestingly, when asked if CBD was harmful or addictive, 70% of participants reported that they did not believe CBD was harmful or addictive. However, about half of individuals admitted that they would feel more comfortable about considering the use of CBD products if these products were prescribed and/or distributed by a doctor.
Overall, the majority of individuals included in this study reported positive attitudes about the use of CBD-related products for managing pain. Furthermore, the results of the study also suggest that CBD-related products may provide an alternative non-opioid treatment strategy that may help reduce symptoms related to common chronic pain conditions, as well as reduce the use of opioid medications for symptom management.
Britt Knight, postdoctoral trainee, University of Connecticut, US.
The essayist Elaine Scarry, in her 1985 book The Body in Pain, wrote, “Physical pain does not simply resist language but actively destroys it.”
Being in pain is hard to experience and also to convey accurately to others. Pain’s indescribability is frustrating for both sufferers and health care professionals. When we are hungry or thirsty, we know what to do to fulfill such physiological needs. When we fall in love, we search intensely for words and poetry to describe how this truly feels to us. But which words or methods are available to define the pain we are feeling?
In the history of pain research there have been many attempts to measure pain. The most widely adopted tools rely on the subjective reports of patients. In the 1950s, the psychologist Ronald Melzack began to collect the words that patients used most frequently to describe their pain. In an attempt to comprehend pain’s emotional dimensions, besides the primary nociceptive one, he organized this vocabulary into three categories: sensory, affective, and evaluative. The result was the McGill Pain Questionnaire, still very much in use today, although there have been studies questioning its efficacy in a clinical setting.
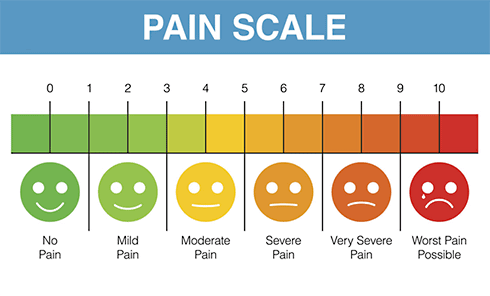
By far the most frequent tool used today to measure pain is the classic 0 to 10 numerical scale. This range of numbers is commonly accepted and used to accommodate more gradations of sensation. But is it really enough to describe pain?
Rating a headache from 0 to 10 gives a number that is relative to previous experiences, to a sort of “baseline level,” and also to cultural background and language. Thus, it is relative to the individual and can also reveal the extent to which cultural context shapes language and, therefore, perception.
A dear friend of mine, E., suffers from a still-undiagnosed chronic pain condition. Imagine waking up every day asking yourself, “How much is it from 0 to 10?” Then, depending on the answer each day, E. must consider whether it is possible to leave the bed and prepare breakfast. There is no official name for such a pain condition, according to the 12 specialists whom she has seen, so she calls it “simply a pain that starts from the base of the neck, travels along the spinal cord, expands to the ribs, the pectoral muscles, and its latest stop is my knee joints.” Further, she says, “On the days that pain comes I feel fear, shame, anger, and despair. But as in every game, there is a master villain. For me it is loneliness. The fact that none, besides maybe the ones who are experiencing it, are able to help or understand how desperate you are during the time that each centimeter of your body is hurting.” What score would all of this correspond to?
The unsatisfactory outcome of the numerical scale and the self-reported nature of pain scores make physicians unable to standardize treatment or to assess how successfully a treatment has worked. There is a need not only to increase the understanding of the neurobiology of pain, but also to find ways to compare and quantify its dimensions.
“Getting to know” the patients can help to achieve a true person-centered assessment of the pain condition. When patients use more words for their pain, they also help doctors gain a more precise understanding of how pain affects patients' daily lives. Instead of pain “actively destroying the language,” each sufferer can open a door toward new ways to communicate pain.
Federica Franciosa, PhD student, University of Bern, Switzerland.
Graded Motor Imagery: Training the Brain as a Treatment for CRPS
GMI, or graded motor imagery, is a cool rehabilitative approach originally described by Lorimer Moseley in a randomized controlled cross-over trial he conducted in 2004 (see here). Its potential as a treatment for CRPS is interesting.
CRPS is not only a regional limb problem, but neuroimaging studies have shown changes in sensory cortical processing, disinhibition of the motor cortex, and a disrupted body schema, leading to some funky changes in the brain and the rest of the body (for more detail on CRPS and neuroimaging, see here). It’s been hypothesized that these brain changes can lead to phenomena like “delayed laterality,” where the person will have difficulty discriminating between left and right; “cognitive neglect,” where the person will express how a body region doesn’t feel like it belongs to them; and “referred sensations,” where touching the affected body region will elicit sensations in a completely different body region (more on referred sensations here). Interestingly, these changes have not only been seen in CRPS patients, but in post-stroke pain and phantom limb pain.
The super cool thing about the brain is that it has the ability to change, and this is where GMI comes in. GMI involves a three-stage process: 1) Recognition of laterality; 2) Imagined movements; and 3) Mirror therapy.
Briefly, recognition of laterality involves being shown pictures of the person's limb in different positions and attempting to discriminate whether it is the left or right limb as quickly as possible. The pictures can vary from being generic, to adding more context and an increase in difficulty, to something more abstract. There’s a cool app by the Neuro Orthopaedic Institute (Noigroup) called “Recognise app” that is designed exactly for that (see here).
The next stage, imagined movements, involves mental visualization of the affected limb in different positions and movements that relate to the individual’s contextual environment. This can also progress from visualizing simple movements like moving your ankle up and down to more functional tasks like hopping or running.
Lastly, mirror therapy involves placing a mirror between the limbs and watching the reflection of the unaffected limb move. Again, this can progress in various ways, by having both limbs move or performing more functional tasks like grasping objects or writing. For a super cool video of David Butler showcasing how to do mirror therapy, see here.
Now, whether or not GMI is an effective treatment compared to other therapies for CRPS is beyond the scope of the blog, but briefly, a systematic review and meta-analysis from 2013 here, a Cochrane review in 2013 here, and an updated systematic review in 2017 here all concluded that GMI may be effective for CRPS. However, the quality of evidence is low due to small sample sizes and heterogeneity of the populations in the studies. It seems that the frequency and dosage of GMI, and in what order the stages of GMI are completed, might matter as well (see here and here).
Other interesting rehabilitative approaches for CRPS that are still being investigated include tactile sensory discrimination and somatosensory rehabilitation (here and here). Although more work needs to be done from a research perspective, I’m very excited for what’s to come in the future.
Special thanks to Dr. Demetry Assimakopoulos for helping me to write this blog post by providing his invaluable expertise and clinical experience with GMI!
Derick Luu, chiropractor, master’s student, McMaster University, School of Rehabilitation Sciences, Hamilton, Canada.
“Keep Swimming”: Did Dory Read the Clinical Practice Guidelines for Low Back Pain?
A few weeks ago, my kids decided to watch Finding Nemo again. I grabbed a popcorn bucket and enjoyed the movie with them. In the story, a clownfish named Marlin loses his son, Nemo, in the open sea. Marlin and his friend, Dory, set off on a vast ocean journey to bring Nemo home. Marlin and Dory carried a diver's goggle with the possible address to find Nemo. In the middle of the adventure, the mask dropped accidentally in the deep ocean (see video on YouTube here). Marlin was hopeless, with no idea what to do. “Do you know what you gotta do?” asked Dory. “Just keep swimming…. Just keep swimming.”
I was almost sleeping, but something jumped into my mind. Did Dory read the clinical practice guidelines for low back pain? This is the message researchers and clinicians want to transmit to patients with acute low back pain. We usually read statements suggesting “Keep active despite the pain,” according to different clinical practice guidelines for acute low back pain. The primary justification for this recommendation is the favorable prognosis and diagnosis of the condition. Most people with a recent episode of low back pain will improve over time regardless of the treatment received. The back is strong, and there is no evidence showing that everyday movements or postures put the back in danger. Finally, there are more advantages than disadvantages in keeping active despite the pain. For instance, social activities provide a sense of meaning and belonging.
Clinicians and the media should keep reminding people of these messages, and perhaps tell people other stories to motivate them to stay active despite the pain. People like stories about the science of pain. Recently, I read a study showing that moving a part of the body that is exposed to a painful stimulus reduces pain intensity. In the experimental study, the authors administered painful stimuli to healthy subjects' left and right hands. The left hand was always in the rest position, and the right hand moved according to a visual cue. The authors were interested to see if the simple act of moving the right hand reduced the pain. For this, they compared the pain levels between the left hand and the right hand of healthy participants. The study found that the simple act of preparing for the action (before the action) was associated with pain attenuation. In addition, participants reported even less pain during the movement. The authors speculated that sensory attenuation during the movement may result from the combination of sensory and motor inputs. The pain attenuation just before the movement (preparation phase) may result from motor inputs or movement expectation. This study suggests that natural movements have an analgesic effect and calm down the pain system.
I know that this is an experimental study in healthy volunteers. We should not generalize the findings to people with acute low back pain. However, the Finding Nemo story and the experimental study imply “keeping active.”
How many stories can you tell patients about the importance of staying active despite the pain? I would love to hear them. Follow me on Twitter @rodrizzo_pain.
Rodrigo Rizzo, doctoral candidate, Neuroscience Research Australia (NeuRA) and the University of New South Wales (UNSW).
We will soon be witnessing the culmination of a massive OxyContin lawsuit and with that, quite possibly, the end of media coverage of the opioid epidemic in the US. The rising awareness of opioid dependency as a major public health concern is closely paralleled by increased interest in medical cannabis. Clearly, patients suffering from severe or chronic pain are still in need of analgesic treatment, and pharmaceutical components are one tool that no one seriously wants to do away with. But are we in danger of replacing one highly addictive drug with the next best thing?
TLDR (Too Long, Didn't Read): No, not really. But the price we have paid as a society is too high for us not to learn our lesson.
The trend we currently see is one toward more liberal laws concerning medical and recreational cannabis use. More patients will seek alternatives to opioid treatment. More clinicians will be helpfully educated by companies selling the products their patients seek. Finally, more patients will just try and self-medicate. It would be in all of our best interests to curate the information we have, very much including all the facts we are not sure about, and to make all of it available and understandable. What we have instead is a cacophony of pot enthusiasts who (correctly but beside all points) remark that cannabis has been used as a herbal medicinal product for hundreds of years“the most dangerous drug”reviews of systematic reviews are being written.
But if I were a physician or a patient, all I would really want to know is: Does it help? Does it hurt?
The issue is complicated in the case of cannabis, not only by conflicting political stances but also by the messy definition of what is being discussed: The whole plant or one of the at least 113 cannabinoids it contains? The best-studied cannabinoids are THC and cannabidiol (CBD), which have wildly different spectra of effects. THC is the psychoactive component most relevant for recreational users, whereas CBD acts in many ways as the benign brother of THC, mitigating many of its more adverse effects. Add to that the standard challenges any new drug faces – dosage recommendations, pharmacokinetics, the best form of delivery. This is the 2020s, after all; no sane person will advise you to start smoking to benefit your health.
Considering that for a comprehensive answer to our first question (“Does it help?”) we would need large, pre-registered randomized controlled trials for any combination of the factors described above, it is not surprising that science has not yet arrived at a consensus concerning efficacy. There is some evidence that medical cannabis (any of the fuzzy set) may help reduce pain in neuropathic pain conditions, cancer pain, fibromyalgia, and migraines. CBD might help in reducing the number of opioids necessary to achieve a constant level of pain reduction. This is not solid evidence, and appreciating this is fundamentally important to manage expectations.
But evidence-based medicine does not equal randomized controlled trials only. Non-clinician scientists tend to forget that the physician's expertise and the patient's experience are just as valid a source of evidence as are the studies. The physician knows the patient much better than the researcher knows the study participant. Patients know their pain so much better than either.
In my world, this amounts to the pivotal point shifting to question 2: “Does it hurt?”
And here, the research seems a lot less conflicted. If you are not intending to regularly smoke large quantities of something of uncertain composition, if your brain is mostly matured, if you are not at an unusually high risk for psychoses, and finally, if you are talking to a physician to check for possible drug interactions, the risks look very acceptable, especially for combinations with less THC and more CBD than is customary for recreational use. A systematic review focusing on medical instead of any other cannabis use found that serious side effects were as common in those who received cannabinoids as in those who received placebos, and made up less than 5% of all observed adverse effects. The risk of becoming addicted is lower than for alcohol or nicotine or opioids.
So, no – cannabis is not the next Oxy. But let us try to stay ahead of clever marketing campaigns this time. What we have in our toolbox to manage pain is not enough. Physicians know it, patients know it, and you can be sure that people trying to make money know it, too.
Malika Renz, PhD student, Central Institute for Mental Health, Mannheim, Germany.
Pain in Autism Spectrum Disorders, Part 1: Sense and Sensitivity
Autism spectrum disorder (ASD) is an umbrella term for several conditions including autism and Asperger’s syndrome. ASD is characterized by social deficits, repetitive or restricted patterns of behavior or interests, and sometimes sensory processing difficulties. It is estimated that one in 160 children worldwide have an ASD, although this is higher in countries such as the UK, where 1.76% of children and 2.21% of U.S. adults are affected.
Understanding how pain is experienced and communicated in ASD is especially important as pain-causing medical conditions are more common in those with ASD than their neurotypical counterparts. Gastrointestinal (GI) disturbances are particularly common, with severity of autistic symptoms correlating with GI symptoms like abdominal pain. In women diagnosed with an ASD or attention deficit hyperactivity disorder (ADHD), a staggering 76.6% reported being in chronic pain. With all this in mind, what key differences in the pain experience in ASD should we be aware of?
One sentence in this article stuck out to me, where a person with Asperger’s syndrome describes how accepting sensory experiences that he found extremely uncomfortable led to him becoming "numbed" to intense cold or pain. By having to bear an unpleasant sensation that most others deem harmless, he also dulled his response to potentially harmful, painful sensations.
While autism can present without sensory abnormalities and vice versa, the vast majority of children and adults with ASD experience them. This manifests as an aversion to certain sounds, textures, smells, or colors. As an example, from Temple Grandin’s book Thinking in Pictures, clothes can feel like sandpaper or rain can sound like gunfire. Multisensory signals are inadequately filtered, so that less relevant information like background noise is not dampened. This reduced "tuning" can also cause sensory perceptions to be more intense.
Pain is a sensory and emotional experience, so what does unusual sensory processing in ASD mean for the processing of pain?
For some time, the misguided notion that individuals with ASD felt less pain was prevalent in research (as discussed and debunked here). This notion was based on clinical impressions and a popular hypothesis of an overactive endogenous opioid system. Many early studies of endogenous opioids in ASD were methodologically flawed, with unsuitably matched control groups. Recent evidence has failed to support this hypothesis, and rather than demonstrating pain insensitivity, found that physiological responses to pain (such as increased heart rate) may actually be higher in those with ASD.
A large proportion of people with ASD have hypersensitive tactile processing, as exemplified by the descriptions by Temple Grandin mentioned above. Several studies have explored how mechanical pain responses may differ due to this, and this research has been reviewed here. Surprisingly, perhaps, findings were inconsistent, with mostly negligible differences between autistic and non-autistic groups.
While reactions to pain by those with ASD may seem unusual from a neurotypical perspective, this is more likely a reflection of diverse communication types than any pain indifference.
Keep an eye out for my blog post next week, where I will talk about how emotional and social components of ASD influence pain.
If you would like to continue this conversation, feel free to contact me by email (sofia.fontana-giusti@reading.ac.uk) or via twitter, @sofia_fg_9.
Sofia Fontana-Giusti, research assistant, University of Reading, UK.
Women and Pain, Part 2: No, Your Patient is Not “Emotional”
Most patients suffering from chronic pain are women, yet most of the research on chronic pain is investigated in male human subjects or male rodents. Last week, in Women and Pain, Part 1, we explored the (deplorable) reasons for such persistence in using male animals in research. You can check out last week’s blog post here.
In addition to a poor consideration of sex differences in mechanisms of chronic pain onset and maintenance, there is also a discrepancy between the clinical experience that men and women receive. In a 2008 study, it was found that women are 25% less likely to receive opioid analgesics than men reporting similar pain scores, and were instead given sedatives. The same study stated that, on average, women who report to the ER with acute abdominal pain wait 65 minutes before receiving adequate analgesics, while men wait only 49 minutes.
So why are women treated so differently in pain treatment and management? This study suggests that implicit biases regarding gender norms contribute to health provider-patient interactions. These biases include the notion that women are more emotional by nature, and that their pain must therefore be of psychological origin. As a result, women receive inadequate treatment and management of their chronic pain, and are likely to withdraw from receiving care.
How can we fight these inequalities that women face in the clinic? Advocacy and representation are key. Healthcare providers, scientists, patients, and their families must be able recognize these biases. The chronic pain research, treatment, and management fields would benefit from more representation of women to help eradicate gender cultural norms. Now if only there weren’t biases against women joining these professions….
Check out this week’s book recommendation for insights on this topic.
Valérie’s Book Club
Do you want to read more about how science communication can impact knowledge and discoveries? Join my book club! Every week, I will be recommending a book that illustrates how collaborations between patients and scientists can have immense contributions on the advancement of science and medicine.
This week’s recommendation is Lab Girl by Hope Jahren (2016). Lab Girl is not about scientists and patients working together toward a common goal. Instead, this book exposes the many challenges that women face in the race to excellence in academia. Hope Jahren shares her compelling story of how she battled her way into a competitive and male-centric universe: the world of scientific research. Despite her tales of anxiety related to limited resources, pressure to publish, and intimidation by the university (male) club, Hope finds fulfilling and inspiring adventures within her passion for plant science. If you are currently a graduate student in need of a different life/career perspective, I recommend this one.
Valérie Bourassa, PhD candidate, McGill University, Montreal, Canada.
“Participants in Pain Studies Are More Than Just WEIRD….”
Most experimental human behavior and psychology studies include participants from WEIRD – Western, Educated, Industrialized, Rich, and Democratic – societies. In fact, “96% of psychological samples come from countries with only 12% of the world’s population….” (read more here). Clearly, this lack of sampling diversity is problematic, as it substantially limits the generalizability of the findings to broader populations. Given that pain is influenced by individual psychological, environmental, social, emotional, and cognitive factors, it is highly likely that experimental pain research involving WEIRD participants is not generalizable and may not even be relevant to all populations.
However, there are many benefits of conducting experimental pain research with healthy human participants: Specific variables (e.g., the nature, location, and intensity of pain) can be selectively manipulated in a controlled manner; psychological manipulations (e.g., a manipulation of threat value) can be selectively added; there is standardized assessment of outcomes (e.g., Quantitative Sensory Testing); and, importantly, it helps to bridge the gap between animal studies and clinical trials. Therefore, I am not suggesting throwing the baby out with the bath water; pain research in healthy human participants is important and useful. Importantly, though, researchers need to overtly acknowledge the limitations in the generalizability of their findings to all populations.
Further, even within WEIRD societies, people who knowingly volunteer for experimental pain research may not be representative of their WEIRD population. Kai Karos and colleagues from Belgium published a fascinating paper investigating sampling bias in pain research. They found that people who volunteered for a pain study were likely to have low levels of fear of pain, and have higher levels of sensation-seeking, than people who volunteered for non-pain-related studies. Therefore, important characteristics that may influence pain outcomes can differ between people who do volunteer and people who do not volunteer for pain studies.
Experimental pain research is useful for researchers to gain insight into the mechanisms of pain and to inform improved treatments. However, pain researchers need to be mindful of the limitations in the generalizability of their findings, and of potential sampling bias. There need to be greater efforts to support and encourage cross-culture research. Further, researchers need to gain a better understanding of the characteristics of participants in their pain studies so that they can control for potential confounding factors. Expanding cross-culture research and thoroughly investigating the characteristics of samples will help make pain research findings more relevant and meaningful.
Gill Bedwell, PhD candidate, University of Cape Town, South Africa. (Contact me on Twitter @Gill_Bedwell or by email at gillbedwell@gmail.com).
Do We Still Need Animals for Pain Research?
Spoiler alert: Yes, even though I do not like it.
A couple of months ago, after the popular and controversial video about Ralph ̶ a mistreated rabbit talking about his life in cosmetic testing ̶ many people started a debate on social media with two common opinions: 1) Animals do not deserve to be in pain, and 2) Animals should not be used for experimental purposes.
Leaving aside the cosmetic industry and its ethical issues about animal testing, these opinions have always hit me hard, since I use animals for experimental pain research.
Given the moral conflict, some people who know a bit of my work just keep telling me that I should not use rats for my research, that I must find another way to do experiments, and that I deserve punishment for all the rodents I have sacrificed. I could answer yes, yes, and yes, but what many people do not know is that absolutely nobody doing any kind of research enjoys causing pain in little animals, even “in the name of science.” And this statement turns darker when you are a pain researcher, since you need to cause pain in order to study it.
And it does not matter that we are following strict protocols/guidelines approved by international and local committees, breeding and taking care of these little animals with affection and respect (but not too much, to avoid treating them like pets), and receiving proper training to handle rodents. I sometimes still feel guilty.
But beyond the animal suffering, the perceived limitations of current animal models of chronic pain, the subjective nature of pain, and the fact that the majority of analgesic drugs proven in rodents are not effective in humans (the failure of translation) are the most important reasons to still criticize the use of rodents in pain research.
In the debate over animal testing, some people have even expressed this opinion: “We have a lot of people in jail who can be used for testing new drugs.” Even though I consider myself a null philanthropist (using everyday phrases such as “I hate humankind”), I think this sentiment is even more unethical than the use of laboratory animals themselves. Moreover, to manage a group of people with different social backgrounds, pathologies, drug consumption, genetics, and many other factors affecting the pain response is much more difficult and expensive, adding the challenge of having a “healthy” control group (for more thoughts on that topic, read this interesting post by Malika Renz, my fellow PRF Correspondent).
For sure, lab rodents do not react the same as we do, but both animals and humans share this feature about pain: It is a subjective experience. So we don’t know how a rat is feeling pain because it can't tell us, but we do not even know how any person feels pain, even when a person says, “Your pain is not my pain.”
However, animal models can offer a fine characterization of the physiology and anatomy that underlie pain conditions, allowing for back-translation. Thus, models are created to replicate pathological conditions seen first in humans, and this leads to an understanding of the analogous mechanisms, molecules, and neuronal circuits regulating pain processing. Surprisingly, animal models have helped with the understanding of behavior considered solely human, such as the placebo effect, as well as empathy for pain relief.
Nevertheless, efforts are made to improve translation from animal models to human physiology using cell lines, computational programs, neuroimaging studies, genetic sequencing, artificial organs, or organs from donors. Although all these tools are already in use, they still need to be complemented with better in vivo studies for a more effective elucidation of chronic pain mechanisms and therapies.
 In short, as long as treatment for chronic pain remains insufficient, we still need a greater understanding of the physiology underlying pain by using animal models (at least until computers can firmly predict biological responses and include their variability).
In short, as long as treatment for chronic pain remains insufficient, we still need a greater understanding of the physiology underlying pain by using animal models (at least until computers can firmly predict biological responses and include their variability).
***Eternal gratitude. The above tattoo is my daily reminder to show respect for all lab rodents I have used in my research. Made by tattoo artist @chrispeste, from Mexico City.***
Yarim De la Luz-Cuellar, PhD student, Center for Research and Advanced Studies, Mexico City.
What Is Central Sensitization?
Is central sensitization (CS) a mechanism/concept to explain changes in the nervous system in patients with chronic pain? Or can we diagnose CS in patients and use it as a treatment target for precision medicine?
Before I started to write my blog post this week, I came across an interesting debate on Twitter with regard to the above questions that are raised in a Lancet Rheumatology paper by Jo Nijs et al. In academia, we can all agree that a debate amongst researchers and scientists is always very engaging, and so my blog post this week will discuss this paper, the debate, and my thoughts on it.
The paper received four responses published in the August issue of the journal, with two of the responses centered on the question of what CS is, which was the crux of the paper. The authors of the paper reviewed evidence on the features of CS in different chronic pain conditions including fibromyalgia and osteoarthritis, and provided evidence that these conditions have different degrees of CS. They defined CS (with a caveat that the definition was being used only for the review article) as “an amplification of neural signaling within the CNS that elicits pain hypersensitivity,” translating to an increase in neural connections/pathways in the CNS, leading to increased sensitivity to pain.
The paper then describes diagnosing CS to classify patients into different profiles using quantitative sensory testing (a battery of tests used to assess sensory function using vibratory, thermal, pressure, and cold stimuli) and questionnaires like the Central Sensitization Inventory (a screening instrument for assessment of symptoms associated with CS). But because of limitations associated with these measures, including but not limited to high variability in responses and an absence of clear diagnostic standards, the authors argue that instead of CS being a diagnosis, it should be used as a prognostic tool. They describe evidence that demonstrates mixed results in using CS as a prognostic tool and then discuss treating CS using pharmacological and non-pharmacological means, but highlight that available data are limited in this area as well.
Lastly, the authors focus on using assessment of CS to provide precision pain medicine (the ability to tailor treatment to an individual patient). Their approach relies on treatment that targets central mechanisms if patients present with features of CS, and treatment that targets the periphery for patients who do not present with features of CS.
Pain researchers were quick to respond with their appreciation of the authors' novel approach, but others were quick to criticize it.
Weisman et al. disagreed with the definition and use of CS, which they believe relies on the idea of enhanced nociception (increased responsiveness of nociceptors in the CNS to noxious or non-noxious input). They strongly oppose the idea of using CS as a clinical tool because there are no studies that use clearly defined and validated criteria to identify CS. Cayrol and van den Broeke had similar reservations about how the authors defined CS, and questioned the description of symptoms and use of the questionnaire to identify CS. They argue that these two measures describe non-painful states and symptoms, and talk about van den Broeke and van den Bergh's work suggesting that a broad interpretation of CS is problematic. The IASP definition of nociception, sensitization, and CS can be found here. Some other papers on CS can be found here and here.
To answer the question I posed at the start, van Griensven et al. published a viewpoint last year that in my opinion provides a very good summary of the current view of CS. They describe CS as a neurophysiological phenomenon and reversible mechanism, but highlight the challenges in its detection in humans due to a lack of available biomarkers. They also say that CS and psychological problems are not identical, and that they shouldn’t be used synonymously. Lastly, we need to have an open mind and allow CS to evolve as a concept.
Bhushan Thakkar, PhD student, Department of Physical Therapy, Virginia Commonwealth University, US.
Week 2: Monday, August 9, 2021
Being in the Cloud – and Creating a New Pain Research Workspace and Hangout
“Healthy Controls”: What Are We Talking About?
Progress in Identifying the 3D Structures of Proteins
Characterizing Multiple Sclerosis Pain in the US
The Evolution of Complex Regional Pain Syndrome: A Brief Historical Overview
A Catalyst to Improve Science Communication and Outreach
“Talking” to the Brain Using WORDS to Manage Pain
A Neanderthal Gene Linked to Pain in Present-Day People
Classifying Pain in Patients With Parkinson’s Disease: A New Mechanism-Based Approach
Complex Regional Pain Syndrome (CRPS): Epidemiology and Risk Factors
Being in the Cloud and Creating a New Pain Research Workspace and Hangout
Postgraduate (PG) students frequently feel lost, alone and uncertain about whether what they are going through is normal. Given that each Masters or PhD research topic is different, the path that each PG student takes is unique. In contrast to undergraduate studies, PG studies have a less concrete structure and often less support. It can be isolating and difficult to gauge whether you are on track or behind with the research project, knowledge and skill development, and research outputs. Further, it is difficult to know whether your project failures (there will be failures) are normal or not.
Urin Alon, a professor at Weizmann Institute of Science, presented an incredible TED Talk on failure during PG studies. He explains that all researchers will experience “being in the cloud” (see figure below). This “cloud” represents what happens when things don’t go as planned: failed projects, personal stressors, supervisor leaves, or a pandemic. Being in the cloud can be distressing, demotivating and uncertain. However, being in the cloud has benefits; the cloud serves as the boundary between the known and the unknown. Once you make it to the other side and arrive at a new unknown destination, you will realize that you have established novel conclusions, which can be far more rewarding for yourself and meaningful to the field than arriving at a known destination.
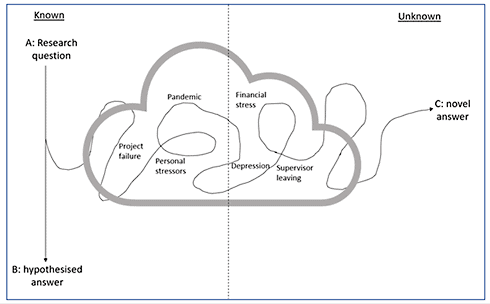
This figure – adapted from Uri Alon’s TED Talk – is a representation of the journey many PG students experience. Initially, PG students start at “A” with a research question and plan to end up at “B” with the hypothesized answer. However, life happens; projects fail and there are personal stressors. This results in PG students diverting off the planned AB path and ending up in “the cloud.” Being in this cloud can be distressing and uncertain. However, the cloud serves as the boundary between the “known” and the “unknown.” Once PG students come out the other side and arrive at “C,” they will realize that they have established completely new and unknown conclusions, which can be far more rewarding for themselves and meaningful to the field than arriving at the already-known B destination.
We need to normalize being in the cloud. PG students need to become comfortable with being in the cloud. For this to happen, I propose that there needs to be a platform where PG students can easily discuss research questions, project failures, administration challenges, course choices, funding applications, and career paths. Through this platform, PG students will be able to share and support each other. In the pre-pandemic era, PG students would meet on campuses to discuss their research project, share challenges, and provide support to each other. However, the pandemic has contributed to PG students being more isolated and feeling more uncertain about their journey.
To mitigate feelings of isolation, maintain motivation and provide support, many other industries have adopted virtual workspaces and “hangouts.” I envision a virtual Pain Research workspace and hangout where PG students with research focuses in pain can “meet” and form a community. On this platform, there will be different channels focused on different aspects of being a PG student: channels for pain-specific scientific discussions, peer review and collaboration, course discussion and recommendations, anything related to funding and grant applications, and of course, a general memes and jokes channel to lighten up moods on difficult days.
My hope is that this platform will facilitate new relationships and future collaborations, and provide support, encouragement and motivation for PG students in the pain world. If you are interested in being a part of developing this platform, contact me on Twitter @Gill_Bedwell or by email at gillbedwell@gmail.com. Here’s to building a supportive, collaborative and international PG Pain Research community!
Gill Bedwell, PhD candidate, University of Cape Town, South Africa.
“Healthy Controls”: What Are We Talking About?
In this week's edition of Private Project Procrastinate, I stumbled across this tweet from Tom Rodebaugh, a professor of psychology at Washington University of St. Louis, US:
Researchers often write that because group X differs from normal controls on construct A, it is important to address construct A in treatment for group X.Yet comparing active treatments rarely (ever?) bears this out.Anyone already described this as a common fallacy?
— Tom Rodebaugh (@drrodebaugh) August 5, 2021
It got me thinking about these normal controls that he mentions. Forget the constructs for now, and the treatment implications, and let's just focus on the groups, because there is a whole story in these two words, “normal controls”!
We can all agree that patients differ from normal controls in at least one way: patients are ill. For instance, my group X, the patients I encounter in my research, are people who suffer either from fibromyalgia or from specific types of chronic pain caused by injury or damage to the joints. And like so many studies, I measure what I am interested in and compare my patients' outcomes to those of a cohort of control participants.
And that is where the trouble begins.
The average patient and the average non-patient who volunteer to be part of a study differ in many, many more ways than only the core diagnosis. Some factors are easy to measure and can be balanced efficiently, like age or gender. But, for the most part, it is not so straightforward. So what exactly am I controlling for here? What kind of normal are we talking about? And why would we even care about normal?
Typically, the ideal participant for a control group is primarily HEALTHY, all capital letters. For my study this means no chronic pain ever, no pain at all in the last three months and under no circumstances any pain during the days of the study. This also means no diabetes, no epilepsy, no tinnitus, no hormonal imbalances that need treatment, no skin conditions, no addictions. No experimenting with drugs. No mental health issues. No mental health issues in your first-degree relatives, ideally. For each and every one of those I could bore you to death with the rationale behind it (picture a brick of a book, maybe leather bound, The Collected Works of Debating Every Little Detail).
My study is not even particularly strict in terms of whom to recruit – contrary to public opinion, PhD candidates do not in general enjoy making their life harder than it already is. Motivating healthy people to donate two days of their time, possibly during their work hours – or worse, during their vacation! –to research that is not lavishly well paying is hard.
It's a very small and self-serving consolation that it has been hard forever. A tremendous amount of research was and is done in students, for one reason only: convenience. Students are generally healthy, smart, compliant and have little money but a lot of time –basically the empty carbohydrates of science. You probably don't need me to tell you that the instant ramen analogue of science is not great science. Or that it is a really bad idea to try and generalize anything when your participants are almost all Western, Educated, Industrialized, Rich and Democratic (aka WEIRD) just because that is how the populace looks like in countries where there is money to spend on science.
But even if all of science finally came together and agreed that from now on, we only fund research with truly representative samples of participants and that no finding based on student samples can be cited anymore – what would an ideal control group look like? What baseline are we controlling against?
The capital-letter Healthy people who have somehow won the genetic and environmental lottery simultaneously?
A norm group with the average ailments of the population, including obesity, trauma, smoking, diabetes, accidents, cardiovascular issues?
The ideally matched group that mirrors my patient group in every respect except for (oh, wait, reality just called to remind me about that one thing where I wanted to not make my life harder on purpose)?
The least dissatisfying answer so far is: it depends*.
On the theories I base my research and on the questions I am trying to answer: Am I interested in singling out the effect that living with chronic pain has on something else? Am I interested in finding possible predisposing or maintaining factors? Or in resources that my patients might have? We probably need to abandon the idea that we can answer all these questions with the same study design.
In the rat race that academia can be, taking this step back might actually be the hardest part. But once we do it, we can focus on the interesting parts: How to measure exactly what we need to, in order to answer our questions. Can we use a dimensional approach and do away with group comparisons altogether for this specific hypothesis? Do I really expect patients with chronic pain to behave and have experiences in a fundamentally different way than everyone else in this phenomenon that I am studying? Or might that just be because they are in pain right now and my controls are not? Can I explicitly model these assumptions and find out which model fits my observations better? And finally, might it not sometimes make sense to recruit controls from the full spectrum of whatever construct I am interested in – physical or mental health issues, injuries and environmental exposures, traumatic experiences, all the things that make our patients more than just their diagnoses?
*No new info here. I just feel the need to highlight how dissatisfying something has to be in order for “It depends” to be not the worst possible answer. Very dissatisfying.
Malika Renz, PhD student, Central Institute for Mental Health, Mannheim, Germany.
A few weeks ago I came across a case study while scrolling through social media. It describes a young man’s experience after overdosing on 29 capsules he was given as part of a clinical drug trial. He was admitted to the hospital, conscious but drowsy. He had an elevated heart rate (110), and low blood pressure (80/40). An IV was started, and he was given saline to stabilize his blood pressure, while the doctors furiously attempted to contact the clinical trial team to determine which drugs he had received. Four hours and six liters of saline later, the patient continued to be lethargic, with a BP of 100/62. At this point a doctor from the clinical trial arrived with good news: the man had been assigned to the placebo group! Within 15 minutes of being told this, the man was fully alert, with normal BP and HR. But if all he took was placebo pills, why did he have the symptoms of an overdose?
Introducing the nocebo effect!
We have all heard of the placebo effect, but the nocebo effect, or adverse symptoms resulting from a harmless substance or treatment, is placebo's lesser-known dark side. There is some evidence that the nocebo effect may be even larger than the placebo effect. This is theorized to be related to the increased importance that we place on threats (compared to rewards or neutral stimuli), since threats often pose greater danger to our body. As a hiker in Australia, I can relate to this; once I spot a snake in the bush it is all I can look at!
The nocebo effect is common, but what does it look like in practice?
The way we describe treatments can produce a nocebo effect. In this study, women who were in labour and about to undergo an epidural were either told “We are going to give you a local anesthetic that will numb the area and you will be comfortable during the procedure,” or “You are going to feel a big bee sting; this is the worst part of the procedure.” Unsurprisingly, the bee sting group reported higher pain levels during the procedure. The nocebo effect can even be produced by the media! After two media outlets ran a story about a switch to a different generic medication among patients taking an antidepressant, the number of side effects increased – especially the side effects that were highlighted in the media coverage.
Learning about the nocebo effect made me think about the way many pain conditions are covered by both the media and healthcare professionals. Commonly used language, such as “this next test will hurt a bit” or “osteoarthritis means your knee joint is bone on bone, so I wouldn’t expect exercise to help much” are very likely to produce a nocebo effect. This often leads to worse outcomes for people experiencing pain! It’s important to consider the way we communicate both research and clinical findings so we can avoid nocebo effects.
Erin MacIntyre, physiotherapist, PhD candidate, University of South Australia.
Progress in Identifying the 3D Structures of Proteins
Proteins are the backbone of biological life. Every cellular communication, process and interaction relies on a protein, and therefore every physiological process that you can think of – from nerves sending signals, to blood clotting, to wound healing, digestion, reproduction and innumerable others – all rely on protein molecules performing a function. Drug action, in a nutshell, typically works by either activating or inhibiting targeted proteins within the body in order to bring the body back to its more normal, ‘healthy’ state. This occurs by the drug molecules interacting with the 3D structure of the proteins, akin to a key fitting into and engaging with a lock. Consequently, knowing the 3D structure of these proteins is critical as it allows for the design of drug molecules that interact with the proteins in the desired fashion.
Until recently, obtaining the 3D structure of a protein relied on laborious and time-consuming processes such as producing a crystalline solid of the protein and analyzing the way in which electrons were diffracted by the crystal (X-ray crystallography), or by using cryogenic electron microscopy, which involves freezing the protein sample before again using electrons to analyze the structure. There are pros and cons to both techniques, but both involve investment of significant time and resources.
Enter DeepMind – Google’s (or rather, Alphabet’s, Google’s parent company) artificial intelligence division, which in late 2020 created a program called AlphaFold for an annual competition to predict the 3D structure of proteins from only the underlying sequence of amino acids. DeepMind inputted information about the constraints upon amino acids and how they interact and fold, and AlphaFold uses this information, treating each amino acid as a singular building block and working out its orientation in space relative to the other amino acids in the sequence.
The result? Nearly two-thirds of the predicted protein structures were of good enough quality to compete with those of structures obtained experimentally. The greatest victory for biology, however, is that as of July 2021, DeepMind has applied AlphaFold to 98.5% of known human proteins and has made these predicted structures available to all via the AlphaFold Protein Structure Database, along with releasing the AlphaFold source code on GitHub.
Even more amazing than the sudden transparency of Alphabet Inc. is the widespread implications of this hoard of data now available to the scientific community. With the majority of human proteins having a trustworthy structure freely available, with the proteomes (the complete set of proteins) of other species promised to follow, this gives researchers a major jumpstart when attempting to understand fundamental biology, including, obviously, that of pain mechanisms and the many proteins involved in those processes, and in the design of future drug therapeutics.
Alice Gregorie, PhD student, University of Leeds, UK.
Characterizing Multiple Sclerosis Pain in the US
One million people in the United States are living with multiple sclerosis (MS), a chronic nonfatal condition that often results in disability and pain. Pain associated with MS can result from the disease’s physical toll on the nervous system, inflammation, or altered signaling within the central nervous system. The complexity of these different contributors to pain can impact pain treatment outcomes. Therefore, understanding how pain varies among the MS patient population may help guide individualized pain treatments and improve patient satisfaction.
In May 2021, Kratz and colleagues from the Braley laboratory at the University of Michigan published the first description of MS-related pain experiences among the US population. The results of the study included surveys from more than 800 participants and describe the types of pain experienced by MS patients, the presence of additional pain conditions, and how well their current pain treatments manage their symptoms.
Participants completed the painDETECT questionnaire (PD-Q) and the American College of Rheumatology (ACR) 2011 Fibromyalgia Survey (FM) to determine types of pain experienced. The PD-Q assesses symptoms that may be related to nerve damage, referred to as neuropathic pain, and the FM survey assesses the likelihood of pain resulting from altered central nervous system signaling, referred to as centralized pain. Comparisons between the two surveys revealed that about 30% of participants reported a high likelihood of having both neuropathic and centralized pain and were thus labeled with a mixed pain experience. About 20% of participants reported having a high likelihood of centralized pain and 10% of participants had a high likelihood of neuropathic pain. Most participants scored low on both surveys, did not have neuropathic pain or centralized pain, and were labeled as having nociceptive pain (i.e., pain occurring from factors, such as inflammation, that activate nociceptors in the periphery).
When asked about overlapping chronic conditions, the most frequent condition reported was migraine. Participants with a mixed pain experience including both central and neuropathic origins were more frequent to report migraine as an overlapping pain condition.
When participants were asked about their pain treatments, NSAIDs were the most frequently reported and steroids were the least frequently reported. Participants with a high likelihood of having neuropathic pain were more likely to report steroid use for pain relief, whereas participants with a high likelihood of having centralized pain, either alone or in combination with neuropathic pain, reported using medicinal cannabinoids, opioids, and antidepressants to manage their symptoms. Participants reported greater satisfaction with narcotic use followed by cannabinoids for pain relief. Participants with mixed pain reported greater pain relief with cannabinoids compared to participants with neuropathic pain only.
In summary, this novel study is the first to describe the prevalence of different pain experiences across the MS patient population and demonstrates the importance of assessing specific pain experiences in order to improve the outcomes of pain treatments for patients with MS. If you want to learn more about MS, please visit the National MS Society website.
Britt Knight, postdoctoral trainee, University of Connecticut, US.
The Evolution of Complex Regional Pain Syndrome: A Brief Historical Overview
“I think complex is the right word because the pain varies in so many different ways” – 13-year-old male patient. – From Exploring peoples’ lived experience of complex regional pain syndrome in Australia: a qualitative study.
Causalgia, Sudeck’s atrophy, algodystrophy, reflex sympathetic dystrophy (RSD) – these were all diagnostic labels for what is now commonly referred to as complex regional pain syndrome (CRPS). So why all the confusing name changes? In this blog post, I’d like to give a brief historical overview of CRPS and how it came to be. This post is largely inspired by this paper, which you can check out for a more detailed overview.
During the American Civil War, there were case descriptions of what seemed to be CRPS-like symptoms after recovery from gunshot wounds. Typically, this involved a description of burning pain distal from the wound with associated skin disorders. Silas Weir Mitchell, an American physician who dedicated the early years of his career to the care of wounded soldiers, began to describe the trophic changes that he saw as, “red, mottled skin in patches, skin that was firmer, less elastic, tight, glossy and shiny, devoid of wrinkles and free from hair.” Hence, the term “causalgia” emerged from Mitchell’s 1872 book titled Injuries of Nerves and Their Consequences (see here). Causalgia derives from the Greek words, καυσός (heat) and ἄλγος (pain), emphasizing the acute inflammatory and skin changes seen in CRPS.
In 1900, Paul Sudeck, a German surgeon, published a paper titled “Acute inflammatory bone atrophy” (see translated article here), in which he described radiographic findings of bony atrophy and osteoporotic-like changes in different acute inflammatory conditions. A student of Sudeck eventually coined the term “Sudeck’s atrophy,” which the medical community began to accept.
In 1946, an American physician by the name of James A. Evans saw that sympathetic nerve blocks relieved the pain in some individuals with CRPS, which supported the theory that the sympathetic nervous system had a large role to play in CRPS pathogenesis. Evans postulated that excess afferent input from the sympathetic nervous system related to the damaged tissue could start a chain of sympathetic postganglionic fiber activation, leading to arterial spasms, ischemia and increased capillary filtration pressure, resulting in edema and swelling (see here, here and here). Hence the term “Reflex Sympathetic Dystrophy” was coined.
However, the role of sympathetic blocks was called into question since not all CRPS patients' pain resolved (see here and here). This eventually led to an International Association for the Study of Pain (IASP) 1993 consensus meeting in Orlando to discuss criteria for diagnosing CRPS. John Bonica, founder of the IASP, acknowledged that the dystrophy in RSD was secondary to the more clinically significant pain symptoms and there should be an emphasis on the localization of pain in a particular region of the body, rather than pain following a particular nerve root or nerve distribution. Hence the term “complex regional pain syndrome” was born.
That’s it from me! I hope you found this as interesting as I did, and if you’d like to read more check out this post from CRPS Network Australia. There’s a lot more to be discussed, perhaps in future blogs, but if you’d like to reach out you can shoot me a message on Twitter @derick_luu.
Derick Luu, DC, chiropractor, master’s student, McMaster University, School of Rehabilitation Sciences, Hamilton, Canada.
A Catalyst to Improve Science Communication and Outreach
Sometimes, the only way to really be sure where strengths and weaknesses lie is by conducting a stress test. The metal components of an engine, the human cardiovascular system, or even the culture and infrastructure of a society sometimes appear functional during day-to-day use, even though a critical failure may be lurking beyond just a small increase in stress on the system. If we’re wise enough to reflect, our experiences in living through a global pandemic over the last year and a half could be that poignant analysis of what we’ve been doing right … and where we’re lacking.
I'd like to share my perspective, though it may be specific to the US, on how we’ve fallen short and how the impact extends beyond COVID.
With so many people having regular access to the Internet, COVID presented an opportunity to connect the world through data. Reports on the number of infections, hospitalizations, and mortality rates are not only readily available and updated on a daily basis, but the information is on the forefront of media across nearly all platforms in an historically unprecedented display. You don’t have to be particularly savvy to find out exactly how people are being affected by COVID throughout the world. This begs the question: Why is it that we still can’t agree on the reality of our problem, if not our best solution to remedy it?
This is a science blog, so I’ll spare us both the radioactive toxicity of discussing politics (even if I think that open and civil discussion of political differences is not only healthy, but crucial). I do, however, question if scientists have done all we could to prepare our society to process all of the information made available on the Internet. Have we empowered people to not only understand the data, but ask the right questions to evaluate its validity? I don’t think that we have.
The scientific method is taught in school during our formative years. But, with the exception of the few people who move on toward a science-related field, the fundamental principles that govern how we accurately understand our world tend to fade from use. Most careers rely on continuing education requirements to refresh and refine necessary skills, but are scientists willing to take the baton from teachers and provide continuing education for the public? We love to communicate our work to our peers (in fact, our jobs depend on it) but much of the American population doesn’t know what a research article is, much less how it’s formed and where to find it. Instead, we expect that they will simply trust our results … and now we’re seeing what happens when they need to, but don’t.
While the US response to COVID specifically illustrates this problem, it could also be a catalyst to improve our communication and outreach across all scientific fields. It’s time to place a higher priority on sharing our work – not just results – to a wider audience. If we can seek out avenues to improve visibility within our communities, speak in a language understandable to non-scientists, and be as equally open about the shortcomings of our findings as we are of the benefits, then we may be able to provide that source of continuing education for the public.
The PRF Virtual Correspondents Program provides a great opportunity for my cohort and I to improve skills that raise awareness of advances in pain research. But I challenge all researchers to use this as a model for enhancing outreach in their individual space, not only to ensure that the public benefits from better treatment of pain, but to indirectly and proactively improve scientific literacy by exposing more of what we do to the public.
Joshua Crow, PhD, postdoctoral fellow, University of Florida, US.
“Talking” to the Brain Using WORDS to Manage Pain
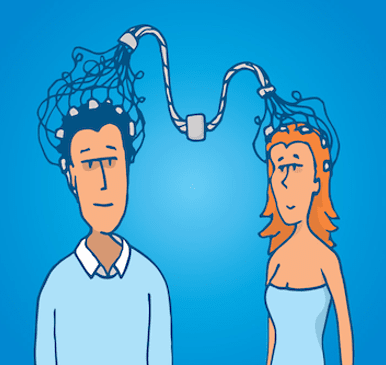
That was the start of Professor Uri Hasson's TED talk in 2016. Hasson, a professor of psychology and neuroscience at Princeton University, shared some exciting research in the field of human communication and storytelling. For one experiment, Hasson's team compared the brain activity of a storyteller to that of a listener, using functional magnetic resonance imagining (fMRI). The researchers realized that the listener's brain activity matched the storyteller's brain activity in the language processing areas and also areas involved in understanding meaning. Interestingly, the stronger the coupling predicted the level of understanding of the story. With these findings, Hasson concluded that the brain is a fantastic device that can record memories, dreams, ideas and transmit them to another brain through communication and compelling storytelling.
What has it got to do with pain?
The brain uses multiple kinds of information to produce the experience of pain, including messages from nerves in the body, expectation, attention, previous experiences, emotional states, social influences, interpretation of an event, and inputs from the sensory channels (e.g., visual, auditory, tactile). Researchers have investigated strategies to manage these cognitive or emotional factors and change the perception of pain. One of these approaches suggests “talking” to the brain using verbal suggestions. Words can transmit meaning, switch people's attention, create expectations, awaken previous experiences, and trigger emotional states. Some people would easily remember the warm sensation in their hands when getting close to a campfire in a pleasant winter. The simple presentation of individual pain-related words (e.g., sharp, sore) just before an experimental pain stimulus can engage more brain areas related to pain than neutral words (e.g., chair, shirt). It makes me wonder what happens in the brain when a patient says, “[the professional] said it is the tendon breaking down, degenerating.”
Some research has tested the impact of more elaborate verbal suggestions on brain activity and the experience of pain. In one study, researchers provided people the following information during a painful experiment: “Although you will continue to experience normal sensation, your experience will seem surprisingly more agreeable … surprisingly more comfortable…. ”The investigators found that these suggestions mainly target activity related to the emotional aspect of pain. In another study, researchers provided a different suggestion: “You may be surprised to notice how much less intense the sensation is and how it tends to feel only warm…. ”These researchers showed that these verbal suggestions might reduce pain intensity or discomfort, depending on the type of suggestions people receive.
We also see the impact of therapeutic approaches such as instructions, education and therapeutic suggestions on some outcomes in clinical trials. For example, teaching people about the anatomy of the back is more threatening than teaching people about how changes in the nervous system are related to chronic low back pain. We are still not sure why it happens, but people who receive information about how their nervous system works commonly say, “My body is actually safe even though it feels so painful.” Can this perception reduce chronic low back pain?
Rodrigo Rizzo, doctoral candidate, Neuroscience Research Australia (NeuRA) and the University of New South Wales (UNSW).
Image credit: curvabezier/123RF Stock Photo.
“To be enlightened is to be aware of total reality in its immanent otherness – to be aware of it and yet remain in a condition to survive as an animal.” – Aldous Huxley, The Doors of Perception

Psychedelics are mind-altering drugs that cause hallucinations and can bring about feelings of deep understanding or expansiveness. They primarily work by amplifying a specific receptor in the brain called the 5HT-2A receptor. This receptor has a role in memory, learning, fear and altered states of consciousness.
The term “psychedelic” was coined in the 1950s by psychiatrist Humphry Osmond, in communication with writer and friend Aldous Huxley who notably wrote, The Doors of Perception about his experience taking mescaline. The term “psychedelic” is derived from the Greek words psychē (soul), and dēloun (to reveal, make visible).
The “mind-revealing” properties of psychedelic drugs propelled neuroscience research into studying the effects of psychedelics on consciousness in the latter part of the 20th century.
Many of those studies lost steam following the global “war on drugs” and amid concerns about psychedelics' safety profile, in particular the danger of drug-induced psychosis or paranoid and disordered thinking in those vulnerable to mental illnesses such as schizophrenia.
A recent resurgence of interest in psychedelics as medicines has been developing since the turn of the millennium. Trials of psychedelic drugs have been refined by combining these drugs with psychotherapy and under medical supervision, along with screening for genetic susceptibilities to unwanted mental reactions, and dose adjustment.
Recently, promising evidence has emerged that psychedelics can improve various psychiatric conditions. The “club drug” MDMA, known as ecstasy, is a stimulant with psychedelic properties that was found to improve severe post-traumatic stress disorder. Psilocybin, the active component of “magic mushrooms,” has gained considerable interest for its ability to improve treatment-resistant depression.
Despite a growing body of research on psychedelics for depression, there is little evidence on how they may affect chronic pain. Some anecdotal evidence and exploratory studies suggest benefits of psilocybin for phantom limb pain in amputees, and for migraines.
It is not clear if amplifying sensory perception would improve or exaggerate pain. However, it may be that psychedelics are effective in treating chronic pain states that persist over many months, rather than acute pain. Chronic pain can continue long after an injury is healed, or from ongoing disease and injury. These persistent pain states are maintained by several mechanisms, from sensitization of peripheral nerves to an increase of nociceptive signaling in the spinal cord and brain.
Resting-state brain connectivity is thought to be elevated in patients with chronic pain, which may be involved in the generation of spontaneous pain. One proposed mechanism for psychedelic action on pain is to “reset” these areas of connectivity, which has been observed in imaging studies of the brains of patients taking psilocybin for depression.
While the sensory-distorting properties of psychedelic drugs may have been emphasized in art forms that were inspired by use of these drugs in 1960s counterculture, it is their mind-revealing properties that appear key to their potential therapeutic value. The ability to break away from neural patterns etched by trauma, grief, or pain could be a very useful adjunct to conventional therapies.
Sofia Fontana-Giusti, Research Assistant, University of Reading, UK.
Image credit: Photo 120783069 © Blkrzyzanek | Dreamstime.com
Women and Pain, Part 1: How One Simple Housekeeping Step Turns Off Researchers From Considering Female Animals
I started my graduate studies by investigating pain mechanisms in a rat model of osteoarthritis in 2014. Back then, I could count on one hand the number of researchers I knew who used both male and female animals to study chronic pain. This tendency was not exclusive to chronic pain; most disciplines use male rats and mice by default for many research initiatives. Why is that? It has been claimed that female research animals have hormonal cycles that can complicate data, especially in a field like chronic pain where behavioral tests are important. The idea is that within one experiment, you may end up with one female in the luteal phase and another female in the follicular phase of the estrous cycle. These two females might react very differently to a stimulus, not because of their pain, but because of their baseline reaction influenced by hormones. Funny enough, no one seems to ever care about testosterone surges in male animals.
One of my dear colleagues specifically chose to tackle sex differences in osteoarthritis pain. It turns out you can sync up the estrous cycles of female rats and minimize variability in baseline measurements by doing this one thing: you recycle dirty bedding from male cages and place it in the female cages on a regular basis. That’s it! No expensive apparatus, no extensive manipulation: you literally only need used bedding that would normally go in the trash. Although it is true that adding female rats to a study will increase the cost of the study (more animals, more drugs, more time, etc.), the benefits of having both sexes represented in fundamental scientific research far outweigh these costs.
So why is there still more research done in male than female animals? Unless challenged, scientists may assume no differences in mechanisms between males and females, and for simplicity, or maybe even by habit, choose to work with male animals only. Ultimately, it is critical to remember that 2/3 of chronic pain patients are women, and for this reason we should encourage a mindset switch in scientists to prioritize sex differences in their research aims.
Check out next week’s post on the Pain Research Forum titled Women and Pain, Part 2: No, Your Patient is Not “Emotional” to learn about more biases that women endure in the field of pain – this time in the doctor’s office.
Valérie’s Book Club:
Do you want to read more about how science communication can impact knowledge and discoveries? Join my book club! Every week, I will be recommending a book that illustrates how collaborations between patients and scientists can make immense contributions to the advancement of science and medicine.
This week’s recommendation is Invisible Women: Data Bias in a World Designed for Men, by Caroline Criado Pérez (2019). Have you ever contemplated the degree to which data and statistics influence our world’s most important decisions, whether it’s about economics, health, or public policy? What if I told you that most data that has been acquired to this day has failed to consider gender, therefore appointing men as the default population, and women as anomalies? Invisible Women explores many instances of biases that have cost women time, money, opportunities, and sometimes their lives.
If you are anything like me, as you read you will grow so increasingly livid at the blatant mistreatment and injustice that women have endured vis-à-vis healthcare, education, and public policy, that you may have to put this book down often to take some breathers. However, it is our responsibility as clinicians, researchers, patients and families to acknowledge and increase the visibility of these biases to improve the treatment and management of chronic pain in women. Sound off in the comment section below if you would like to share your experience with gender disparities in research or treatment of chronic pain!
Valérie Bourassa, PhD candidate, McGill University, Montreal, Canada.
A Neanderthal Gene Linked to Pain in Present-Day People
Pain is a complex and subjective experience that can be influenced by biological, psychological, social, cultural, and genetic factors. Given different social and environmental conditions, it is hard to believe that the perception of and reaction to pain was the same 50 years ago, 300 years ago or thousands of years ago compared to the present day. Nevertheless, with our genes carrying traces from our early ancestors, it makes sense that we still share some pain features.
Homo neanderthalensis is our predecessor from 500,000 years ago. Recent studies (see here and here) have revealed the presence of Neanderthals in America and even Africa, in contrast with previous literature placing them only in Europe and Asia, So, according to these results, everyone around the world has a bit of Neanderthal DNA in them.
Svante Pääbo, a Swedish geneticist at the Max Planck Institute for Evolutionary Anthropology in Leipzig, Germany, and his colleagues have worked extensively to obtain the complete genomic sequence from three Neanderthal DNA specimens found in caves in Croatia and Russia. Thus, now scientists can compare the Neanderthal genome with human DNA from the present day.
In fact, work led by Pääbo and first author Hugo Zeberg from the Karolinska Institute in Stockholm, Sweden found a mutation in the SCNA9 gene (encoding for the voltage-gated sodium channel Nav1.7) on both chromosomes in the Neanderthal genome. Nav1.7 channels are proteins widely expressed in peripheral sensory neurons – and have a recently discovered and surprising role in the spinal cord! – and are essential for the generation and transmission of electrical signals into the spinal cord and brain. These electrical impulses underlie nociceptive signaling from the periphery to the central nervous system.
It is well known that loss-of-function or gain-of-function mutations in SCNA9 can result in congenital insensitivity to pain or hypersensitivity to pain in painful neuropathies, respectively. Since the Neanderthal SCNA9 codes for three different amino acids compared to the modern human protein, researchers synthesized and inserted this gene into frog eggs and human embryonic kidney cells to determine the function of Neanderthal Nav1.7. The single amino acid substitutions do not affect the function of the ion channel, but electrical stimulation of the Nav1.7 channel that had the amino acid substitutions increased its availability for activation, as well as its probability to remain open for a longer time once activated. This would lower the threshold to generate action potentials in sensory neurons and, therefore, the threshold for detecting painful stimuli, causing heightened pain sensitivity in present-day people.
Moreover, a database analyzis demonstrated that 0.4% of 362,994 British individuals had inherited the Neanderthal SCNA9 with the three different amino acids, and these people reported being more sensitive to pain than people with the current-day Nav1.7 gene.
Certainly, not everyone with a low pain threshold can blame it on the Neanderthals. Other genetic variants or current-day factors can impact people’s experience of pain, so perhaps the effect of the Neanderthal gene is small compared to other mutations associated with chronic pain.
Even though these results suggest that Neanderthals were more sensitive to pain, I am convinced that Neanderthals did know how to deal with pain sensitivity in extreme and dangerous conditions. Since pain is not always a bad thing, perhaps this hypersensitivity could give them an advantage for avoiding injuries and increasing their likelihood of survival.
This study from Pääbo and colleagues is very interesting as it provides insight into how pain physiology has evolved over time.
Yarim De la Luz-Cuellar, PhD student, Center for Research and Advanced Studies, Mexico City.
Classifying Pain in Patients With Parkinson’s Disease: A New Mechanism-Based Approach
Parkinson’s disease (PD) is a neurodegenerative disease. It is also a chronic and progressive condition, with symptoms becoming worse over time, characterized by its most common motor symptoms. These include tremors, stiffness or rigidity, and slowness of movement. PD also involves non-motor symptoms like sleep problems, constipation, anxiety, depression, and fatigue, among others. While there is no cure for PD, there are a number of medications and surgical alternatives that can ease symptoms. The Parkinson’s Foundation in the United States has reported that almost one million Americans are currently living with PD and the condition affects more than 10 million people worldwide. Approximately 60,000 Americans are diagnosed with PD each year.
Another common non-motor symptom in PD is chronic pain. It is a frequent and disabling symptom with significant effects on physical and mental health-related quality of life. Typically, pain in people with PD (usually musculoskeletal pain from other conditions like osteoarthritis or low back pain) is nociceptive in nature, or it is linked to the presence of motor symptoms, or it is neuropathic.
Different studies (see here, here, and here) report varying prevalence rates (40-95%), and pain is typically present at the onset of PD but it is often underrecognized and undertreated (see here and here). Analgesic consumption among PD patients with chronic pain is reportedly lower than in people with chronic pain attributable to other conditions. In older PD patients with chronic pain, it becomes increasingly difficult to diagnose and treat the pain because of co-morbid chronic pain conditions. Some of the contributing factors to the lack of understanding of the relationship between PD pathophysiology and pain include reliance on clinical judgment alone, a lack of standardized tools, inconsistencies in pain descriptions and an inability to determine whether or not a given pain source is considered a feature of PD. It is critical to accurately identify the different phenotypes of people with PD pain, in order to explain underlying mechanisms, which could potentially aid the development of patient stratification models to guide treatment.
Keeping this in mind, more recently, Mylius et al. developed a new rater-based method termed The Parkinson Disease Pain Classification System, with the goal of defining PD-related pain and to distinguish it from pain unrelated to PD using a mechanism-based classification to allow for treatment approaches that target pathophysiology. These researchers used four questions developed from previous pain classification systems to differentiate PD- from non-PD-related pain and then classified the pain into three mechanistic descriptors (nociceptive, neuropathic, and nociplastic). Next, they rated the frequency and severity of pain, and its impact on daily living. The scale can be found here. The investigators tested this measure in 159 PD patients with pain and compared these patients to healthy controls.
The group was able to classify all PD patients with pain and were able to differentiate PD-related pain (77% of PD patients) from PD-unrelated pain (22%). More than 50% patients demonstrated nociceptive pain and 22% were diagnosed with mixed pain syndromes (nociceptive and nociplastic, or nociceptive and neuropathic). While the authors reported difficulties with pain assessment between different raters, the scores on the scale also correlated with other commonly used questionnaires that considered the three mechanistic descriptors of pain. Future studies that validate this measure across different PD patients with pain, and combining this measure with medication, rehabilitation and/or surgical therapies could be a big first step towards developing mechanistically-driven treatment approaches to address the significant problem of chronic pain in PD patients.
Bhushan Thakkar, PhD student, Department of Physical Therapy, Virginia Commonwealth University, US.
About four years ago, in a public toilet, I saw for the first time a poster from the World Health Organization: “How to Handwash.” My immediate reaction was to laugh; I had never considered such an action to be a difficult task that required an infographic. As we touch people, surfaces, and objects throughout the day we accumulate microorganisms on our hands and, indeed, handwashing does not take much time or effort and offers great rewards in terms of preventing illness.
This simple habit plays a major role in protecting our health and in fact it was extraordinarily advertised at the beginning of the COVID-19 outbreak. Throughout the world, famous people started posting videos of themselves washing their hands like it was a new thing to do or learn. It made me think of the history of how handwashing became a relevant, then a mandatory practice in the medical world and also popular in the public realm. It might come as a shock to many, but until the mid-1800s even doctors did not regularly wash their hands.
Microbes were yet to be discovered, and the accepted belief placed the “miasma” – an emanation from rotting corpses, vegetation or sewage – as the cause of disease. While working in an obstetric department in Vienna, a young doctor noticed that women who gave birth in the hospital had a much higher mortality rate for childbed fever than women who had midwives and gave birth in their homes. Childbed or puerperal fever is a bacterial infection of the female reproductive tract following childbirth or miscarriage and was the leading cause of maternal mortality in the 18th and 19th centuries. Ignaz Semmelweis – so our hero was named – noticed that doctors and students would be in the morgue dissecting corpses on the same day that they visited pregnant women or delivered babies and without washing their hands. Accidentally, a colleague and friend of his was cut by a scalpel during a dissection and died, apparently of the same childbed fever the mothers had been getting.
Thus, Semmelweis hypothesized that particles from the corpses on the hands of doctors and trainees were making their way into women’s bodies during childbirth and thus discovered “The Origin of Puerperal Fever,” to quote his lecture. He initiated a mandatory handwashing policy with chlorinated lime (calcium hypochlorite), which led to a drastic fall of the mortality rate for women who gave birth in the hospital.
Unfortunately, doctors felt offended by the suggestion that they could be causing infections because of their dirty hands. Therefore, despite the discovery he made, Semmelweis was poorly received and faced great resistance. He lost both his position and his mental health, and would die in a psychiatric institution.
Semmelweis’ advice on handwashing was more influential and powerful than he realized at the time, even if the scientific explanation behind it came only decades later with the work of Louis Pasteur and Robert Koch, which defeated the “miasma” theory, and Joseph Lister, who advocated for sterile surgery.
Handwashing is a simple yet empowering habit with an intense history behind it. It's fascinating to learn how discoveries were made in the past and “reviewed by peers” in the scientific community.
Federica Franciosa, PhD student, University of Bern, Switzerland.
Complex Regional Pain Syndrome (CRPS): Epidemiology and Risk Factors
Complex regional pain syndrome (CRPS) is a condition I have spent the last three years investigating to understand the mechanisms involved in the transition from acute to chronic pain. It is a misunderstood and misdiagnosed condition, and I wanted to take some time to discuss current epidemiological studies of CRPS and risk factors for this condition.
Epidemiology:
There have been multiple retrospective population-based studies investigating the incidence of CRPS. But the results have varied, warranting a more comprehensive way to reveal the true incidence of CRPS. One study completed in 2003 in Olmsted County, Minnesota, US, found an incidence of 5.5 cases per 100,000 person-years. In contrast, a retrospective cohort study performed in the Netherlands only four years later found an incidence of 26.2 cases per 100,000 person-years. However, in the latter study, the investigators used a sensitive search algorithm to look for a diagnosis of CRPS in electronic health records.
The gap in epidemiological studies lasted for 11 years, until a group in Germany took advantage of the main outpatient clinic serving Erlangen, Germany. The investigators determined an incidence of 13.6 cases per 100,000 person-years based on the population. They suggested this was an underestimate, as CRPS is relatively underdiagnosed.
An additional study in 2018 from the Republic of Korea found an overall CRPS incidence rate of 29.0 per 100,000 person-years. The investigators in Korea had the advantage of using national health insurance data to extract the total number of CRPS diagnoses from 2011 to 2015. However, this study used the persistent disability and assessment guidelines by the American Medical Association rather than the IASP or Budapest criteria for diagnosing CRPS. The variation in these reported incidences shows the regional differences in the presentation or diagnosis of CRPS.
Risk factors:
Common risk factors associated with a higher risk of developing CRPS are peripheral injuries like fracture, sprain, and elective surgery, with spontaneous onset uncommon. Many studies have investigated the association with distal radius fracture as an inciting injury for CRPS. In the most recent study, the incidence of CRPS four months post-injury was 3.8% in the cohort, and a pain score in the first week of 5 or greater was a predictor for the development of the condition.
Immobilization of an injured limb might also be a risk factor. In a recent study, healthy human volunteers subjected to immobilization developed mild signs of CRPS. However, perceived cast “tightness” has been suggested as a risk factor for developing CRPS and should be considered in post-injury immobilization.
Visit here for more comprehensive knowledge on CRPS.
Nolan Huck, MD/PhD student, University of California Irvine, US.
Week 1: Tuesday, August 3, 2021
The Influence of Someone Who Believes in You
Well, That’s One Way to Do It….
When I Realized What I Would Become
One Door (or Six Doors) Close and Another Opens
Studying the Mechanisms of Chemotherapy-Induced Peripheral Neuropathy
From Textiles to Scientific Research
A Biomedical Engineering Approach to Developing New Osteoarthritis Treatments
Can We Enhance Existing Treatments for Pain?
From Potential Zombie Creator to Chronic Pain Researcher
The Influence of Someone Who Believes in You 
Hi PRF Readers!
My name is Nolan Huck, and I will be starting the Medical Scientist Training Program at the University of California, Irvine on August 9, where I will be pursuing both an MD and PhD degree. I just left Stanford University, where I've spent the last three years investigating the mechanisms of the transition from acute to chronic pain, and I hope to continue pain research in my graduate studies.
My first exposure to pain occurred at a young age. I grew up in warm and sunny Cloverdale, California, a small town of 6,000 people. As a child, I vividly remember a man lying bed-bound after a horrific car crash. He had recently undergone a C5-C6 spinal fusion that resulted in his being engulfed in a cervical support halo, making him unrecognizable. As a three-year-old, I timidly walked over to the bed's side, scared by what I saw. Once I got closer, the man became recognizable: It was my dad. His hand slumped off the bed, and I stood on my tippy toes and embraced him, gripping his arm firmly, and while looking up at him, I said, “I love you.” In that short moment together, the pain that had been visibly displayed on his face vanished.
As I grew older, medicine masked my father's pain, as he was quickly transitioned to powerful opioid drugs to control his pain. While the opioids were just a “band-aid” that hid the true nature of his injury, the thought of his pain faded. As a first-generation student, I went to the University of Oregon, received a degree in biochemistry in 2016, and was set on pursuing medicine, as my scientific interests were derailed during my undergraduate studies.
Thankfully, my dad transitioned from his powerful medication to another one, due to the opioid epidemic, but the new medicine no longer cloaked his pain. I met my principal investigator (PI) at a Stanford summer program and learned about opioid and pain research. It was the first time I had thought about the mechanisms underlying my dad's condition and the potential to help families like mine. I was given an opportunity and a belief in my abilities as a scientist. My PI reinvigorated my passion for science, which changed my career trajectory. I fell in love with science and the harmonious balance of being a physician-scientist, hence pursuing an MD and PhD.
My interest in science communication stems from my family's lack of information as we navigated my dad's injury. I hope to develop the ability to communicate to scientists but also to make information accessible to the larger general public. As a scientist, future physician, and member of the general public, I plan to use the Correspondents program to do just that and then continue contributing to science communication throughout my career.
Outside of science, I am a self-proclaimed sommelier and connoisseur of wine. Growing up in the wine country of California had a significant influence on me. On a community level, I am a proponent of mentorship in science and medicine to provide diversity and representation in these fields.
I am looking forward to contributing to PRF with my fellow Virtual Correspondents and engaging with this amazing community. Follow me on Twitter: @Nolan_A_Huck.
Nolan Huck, MD/PhD student, University of California Irvine, US.
Well, That’s One Way to Do It …. 
Getting through college can be tough, but at least there’s a time-honored structure and reassurance in knowing that countless others have blazed a trail to follow – unless, of course, you’re a “non-traditional” student.
My current postdoctoral fellowship at the University of Florida Pain Research and Intervention Center of Excellence (PRICE) is funded by an NIH training grant, and I have access to both considerable resources and mentorship by unbelievably brilliant scholars. However, despite my current good fortune, I was a non-traditional student. I used to be embarrassed to admit it, until I learned to embrace the skillset that is a unique product of my journey. I hope that by proudly wearing this moniker, I might encourage other non-traditional students to lean in, persevere, and have confidence to blaze their own unique trail as well.
As a first-generation college student with no family examples of what lay ahead of me, I didn’t know what I didn’t know. Though I had the emotional support of my parents, my finances ran out in just my second year of college. I had to work (with the shame of being a dropout, no less) to save enough money to return to college. When I finally did resume my degree, it was as the older guy, with no real peer group – a moot point, as most of my time out of class was spent at work to stay in college this time.
I took my degree, along with a passion for teaching and athletics, and became a high school teacher and coach. It only took a few years into my career to realize that I wanted more: more education, more answers, and maybe even a platform to ask more questions. Not knowing where it would lead, I left my career to earn a master’s degree in applied physiology and kinesiology. Under the tutelage of a clinical exercise physiologist during my graduate assistantship, I helped sub-acute cardiac rehab patients find their freedom and confidence through exercise. I used individualized assessment and exercise prescription to empower patients in their battle with movement disorders. I celebrated the small victories as stroke patients rediscovered function, balance, and mobility. And I was motivated and uplifted as people three times older than me simply refused to act their age.
It was a life-changing experience.
The power of movement to impact the quality of life, physical health, and mental/emotional well-being in older adults was undeniable – and yet there were SO MANY questions that remained unasked. I earned my PhD in biobehavioral science to do something about that. Now I study interactions between chronic pain and mobility in older adults with knee osteoarthritis and attempt to discover more effective implementation of exercise interventions. I didn’t know this is where my education would take me, but as non-traditional as it was, I see no other way to have ended up here. I’m exactly where I belong.
I look forward to sharing my work and my perspective on pain and aging research with you all!
Joshua Crow, PhD, postdoctoral fellow, University of Florida, US.
Hello, PRF readers. My name is Derick Luu and I am an early-career clinician and researcher from Toronto, Canada. I’d like to introduce myself by telling a story about my mom, because she is a big reason for what I am doing. My mom suffered a work injury when I was 12 years old, and since my parents, who immigrated from Vietnam with less than a high school education, barely spoke English, my role as the eldest son was to attend my mom’s medical appointments to help with translating. Pain, as we know, is a complex and subjective experience, so in trying to translate such an experience to different medical professionals, I began feeling lost in translation.
After unjustly losing her job as an assembly line worker due to the injury, making no progress with physical therapy, and being in a state of constant pain, my mom felt a strong sense of injustice and eventually hired a work injury lawyer. Due to language barriers, I had to act as the liaison between my mom and her lawyer by exchanging emails, having phone calls, and attending appointments, which caused me to miss classes while I was in high school and undergrad.
I’d like to acknowledge that this is unfortunately a common situation for children with immigrant parents who lack the language skills needed to live in another country.
Eventually this began affecting my mom’s mental health and social life – with the stress of the lawsuit, the constant pain that kept her up at night, and all the pain medication she was on, she started seeking psychiatric help. Amongst her psychiatric diagnoses, my mom eventually saw a physiatrist and was diagnosed with complex regional pain syndrome (CRPS). She eventually started seeing improvements in her physical and mental health, but this journey took more than 10 years. Throughout those years, I learned that pain was more than something just physical, and I had a lot of unanswered questions, so I began to cultivate an intense curiosity to learn more about this thing we call pain.
A little about me (I’m not as exciting, I promise): I completed my undergrad in kinesiology and recently graduated with a doctor of chiropractic degree from the Canadian Memorial Chiropractic College. I will be starting my journey into clinical practice and academia as a master’s student in the rehabilitation sciences program at McMaster University, where my research will focus primarily on CRPS and knowledge translation. I was also a competitive powerlifter and previously held a national record a couple years ago – although in life perhaps the heaviest things we lift aren’t weights, but our feelings.
I am grateful to have been selected to take part in this cycle of the PRF Correspondents program, and I hope that you will find something of interest to you in reading these blogs from myself and my fellow colleagues.
Derick Luu, DC, chiropractor, master’s student, McMaster University, School of Rehabilitation Sciences, Hamilton, Canada.
When I Realized What I Would Become 
“Scientist” is a word used to define a specific group of people who conduct experiments to advance scientific knowledge in an area of interest, who hold a degree to prove it, and who may or may not continue in the journey called academia. At first, one is more likely to learn under the direction of supervisors working in their own lines of research. Then, depending on the mentorship, one receives training in an extremely specific area and is assumed to be ready to “fly” in science.
How does one come to feel like a scientist? It can start with being a curious child, or with realizing one’s ability do well in scientific topics in school, or with a special event in one’s life that directs interest and passion toward nature and science.
I come from a relatively ordinary religious family from the south of Italy. Each Sunday my mother would arrange my hair in a certain way to look pretty in the eyes of God. In church, I learned to keep quiet. One was not really allowed to have opinions, or at least to express them out loud. For me, the priest was an unequivocal figure with an impressive outfit. He would not speak to anyone in particular. He assumed that the Sunday lecture was what anyone standing there at the moment needed.
At eight years old, I could not really formulate an opinion on such a method of teaching. But as I got older, I was instead afraid that I could still not have my say because the priest's form of lecturing left me empty. It didn't even allow me to have questions. Fortunately, when I started high school, I had a great book to look at, with colorful figures and explanations – my first biology book. It was a wonder. I studied it with hunger, and the other topics in school suddenly became uninteresting, almost irrelevant. The chapter on evolution was at the end of the book, meaning that the school year, too, was coming to an end, but not the church year, because as the priest says: “God does not go on vacation.”
So I brought the biology book with me to a Sunday mass. The priest would have his own big fancy Bible, and I asked him at the end of the ceremony to help me make sense of what was written in Genesis versus what was beautifully illustrated in my book. He did not give any explanation whatsoever, but instead listened to everything I said and then said to me: “To my knowledge, a gospel according to you does not exist, Miss.” I felt arrogance in his statement, but I did not feel defeated or humiliated. He did not know it, but he had just lit a match.
That moment for me was the special event. So now, here I am. My name is Federica, and I am an experimental neurobiologist. My fascination in natural phenomena led me to study biology and then neuroscience. Questioning everything, with a healthy dose of skepticism, has always been crucial to what my life as a researcher and a person has become.
Thanks to the PRF Virtual Correspondents Program, I have this great opportunity to share my thoughts and considerations. I hope you will enjoy reading these blog posts as much as I enjoy writing them. Until next time!
Federica Franciosa, PhD student, University of Bern, Switzerland.
Hello, PRF and RELIEF readers!
My name is Erin MacIntyre, and I am one of your new PRF virtual correspondents!
To briefly introduce myself: I was born in Canada, near the Rocky Mountains, and grew up hiking and skiing. In my early twenties, I was fortunate enough to be able to travel abroad (hoping to escape the Canadian winter!), ending up in Australia where I have been living ever since. I spend my free time hiking and camping, taking full advantage of the warm weather. I moved to Adelaide last year to start my PhD, and I am enjoying living in and exploring a new city.
I am also a PhD candidate, pain researcher and physiotherapist. Before starting my PhD, I worked as a physiotherapist with a special interest in helping people with persistent pain. My experience as a clinician is what motivated me to start my research career. As a curious (and slightly nerdy) clinician, I was constantly keeping up with the latest research. However, I found that the questions that I most wanted to be answered simply weren’t being asked.
Clinical trials are, of course, important; they can help tell us if a treatment works. However, they often don’t tell us how it works. And the how is also incredibly important. As clinicians, if we don’t know how a treatment works, we can’t predict who it will work for, how it is best implemented, or how to optimize the treatment. These are basic questions that clinicians face every day when seeing patients. These same questions are also what has inspired my own career, where I hope to explore some of the mechanisms behind the treatments that we offer people with persistent pain.
Why PRF? Because science communication is essential. Years ago, I read this study, which found that on average it takes 17 years for new research to filter down to clinical practice, illustrating how big the gap is between researchers and clinicians. Having been on both sides of this gap, I know that this is a complex issue that will take systemic change to fix. However, on a personal level, I want to be part of the solution! I plan to make science communication a focus of my career. As a young researcher, I hope to use my time at PRF to develop my skills as a communicator and a pain scientist.
I am so excited to have the opportunity to be a part of the Virtual Correspondents Program. I can’t wait to engage with the pain science community, learn from my fellow correspondents, and share some of my thoughts over the coming weeks!
Erin MacIntyre, physiotherapist, PhD candidate, University of South Australia.
One Door (or Six Doors) Close and Another Opens 
Hello, PRF readers! My name is Gill Bedwell and I am a South African PhD candidate investigating the physiological mechanisms underlying the association between childhood adversity and persistent pain in adulthood. Previously, I never considered doing a PhD, let alone embarking on a career in academia. Here is how I got here:
At age 17, an awful knee injury ruined my dreams of becoming a professional dancer and exposed me to the medical professions. Despite this being the toughest time in my life, I am grateful to have experienced it. My multiple surgeries and rehabilitation sessions inspired me to pursue a career in healthcare, specifically physiotherapy. My injury played a huge role in who I am today.
After high school, I enrolled in a BSc physiotherapy degree. I was ecstatic about becoming a physio! However, after a year of physio studies, I felt unsure about my career choice. I couldn’t shake this feeling that there was something missing, something that physiotherapy was not fulfilling. This uncertainty motivated me to seek out other career options. I decided to apply to study medicine. At the time, I thought that medicine would provide me with more career opportunities and fill this void (of unknown origin). However, after multiple application attempts, my goal to study medicine failed (this still stings the ego!).
I got to the end of my physiotherapy degree, and still felt unfulfilled and lost. My options for the subsequent year were: 1) study medicine (I was on the waiting list this time), or 2) complete my community service year (see note below). I decided to seek advice from one of my undergraduate lecturers whom I admired and looked up to – Professor Romy Parker. Given that I had previously expressed a fascination in pain physiology, she suggested I consider postgraduate studies in pain neuroscience. She introduced me to Dr. Tory Madden, who later became my (INCREDIBLE) masters and now PhD supervisor. Romy planted the seed for becoming a pain neuroscience researcher, and through her, and Tory's fantastic supervision and mentorship, I have flourished. I found my calling, and what was contributing to that void; it was research that had been missing. I had never considered postgraduate studies and a career in research until speaking to Romy.
I want to leave you with some words of encouragement. Firstly, it is OKAY to be rejected from a program – let’s normalize this! Rejection does not define you. Secondly, seek advice from those who you admire. People are inherently eager to help! Thirdly, be open to new ideas and options. You never know where it might lead you. Lastly, find a great mentor and never let them go (sorry Tory, you are stuck with me!).
Note: In South Africa, all healthcare professionals are required to complete a compulsory community service year after finishing their degree, in order to become a licensed practitioner. For this year, you are placed to work somewhere in the country at a hospital and/or clinic. It is a fantastic initiative, since our public healthcare system relies heavily on community service healthcare workers.
Gill Bedwell, PhD candidate, University of Cape Town, South Africa.
Studying the Mechanisms of Chemotherapy-Induced Peripheral Neuropathy 
Hello, and welcome to my first blog post as a PRF correspondent! I’d like to start by introducing myself. My name is Sofia, and I’m from London, UK. I’m also of Serbian, Italian, and French descent. Thanks to my upbringing I am multilingual and love to learn about different cultures – and the people from them. Some of my favorite things to do include creating art, listening to jazz on rainy afternoons, and getting out of the big city to fall in love with nature.

I studied pharmacology at the University of Glasgow and then as a master’s student at University College London. In between the two I worked in a hospital, where I was struck by how important pain research is. This may seem like an exceedingly obvious statement, as pain is something we readily recognize as an unpleasant consequence of injury and disease. But what was striking was seeing how new, effective painkillers are some of the most desperately needed items in a clinician’s toolkit.
Developing new painkillers is an important task, but how do we know if they’re working?
People communicate pain differently, as influenced by factors such as social conditioning and communication style. For patients with delirium or those with intellectual difficulties, it is even harder to describe the intensity or nature of their pain. Learning about the diverse ways in which people communicate their needs can help, while improving behavioral testing of laboratory animals is key to developing new treatments.
I work as a research assistant with Dr. Maria Maiarú at the University of Reading. We are looking at a type of pain that can develop from cancer treatment, called chemotherapy-induced peripheral neuropathy (CIPN). Chemotherapy prolongs life by killing cancer cells, but sometimes also damages peripheral nerves. Symptoms such as pins-and-needles, disrupted balance, and burning or shooting pain develop in the hands and feet. On top of being unpleasant, CIPN is the most common reason for stopping chemotherapy early, impacting cancer treatment.
There is no effective pain relief for CIPN, as the mechanisms behind this pain state require further research. We test various pain-related behaviors in mice that have been injected with a chemotherapy drug and take a closer look at the peripheral nerve and spinal cord. Our research focuses on whether a disruption in autophagy – a process where old or unnecessary parts of a cell are digested – is involved in this type of pain.
When people from different backgrounds share ideas and knowledge, we can progress and come up with novel solutions. Scientific communication is vital for this, especially when researchers and those outside of the field share their thoughts and experiences, each imparting their own wisdom to the other.
Over the next six weeks, my posts will cover varied and hopefully interesting topics. There is a lot to talk about concerning pain, as it is not solely sensory but also an emotional experience felt uniquely and individually. How can you scientifically pin down such a phenomenon? We can start by talking about it.

Sofia Fontana-Giusti, Research Assistant, University of Reading, UK.
From Textiles to Scientific Research 
Hello, PRF readers! My name is Alice, and I am a second-year PhD student at the University of Leeds, although in a neighboring parallel universe I am currently a costume designer for theatre productions and films, with a view to specializing in large-scale fantasy productions.
To explain myself, back in sixth form (ages 16-18 in the UK), my plan was to continue studying art-textile and design at A-level (a qualification in the UK that can lead to university, roughly equivalent to a US high school diploma), following on from two years of the subject at GCSE (General Certificate of Secondary Education), which I had absolutely adored, and from volunteering for a summer in a local theatre’s costume department. This would then continue to a university course in costume design or an apprenticeship in a theatre, and eventually some very poorly paid job surrounded by beautiful costumes. My A-level choices, being biology, chemistry, physics, and textiles, did raise a few teachers’ eyebrows, but, credit to the sixth form, they arranged the timetable and the year began.
Three weeks later I switched from textiles to maths A-level for a variety of reasons that are too tedious for here, and thus my scientific career began. The point I am trying to make, for anyone still confused, is that although many scientists live and breathe their subject, and have always known that they would embark upon a PhD, some do not. Don’t get me wrong: I am incredibly happy in the field I have ended up in and with the work I undertake. Scientific research is tough, with a never-ending to-do list, but when it (eventually) goes right and there’s a completed dataset in front of you, I challenge you to find anything that is more rewarding. But not knowing that’s where you’ll end up from the beginning of your university career or even earlier doesn’t mean that you’ll be any less passionate for your subject or any less of a scientist.
So after having made the decision at whatever stage in your life to pursue science, my advice is to follow what you find fascinating. Throughout school I read and loved popular science books – think Ben Goldacre’s Bad Science and Bad Pharma, and Professor David Nutt’s Drugs without the Hot Air (can you see the link I’m making with science communication yet?), which led me to study the sciences at A-level and pharmacology at the undergraduate level, which then introduced me to electrophysiology (the recording of electrical currents across cell membranes). I loved this technique so much that I asked a researcher at the university who specialized in this if he would take me on for my master’s degree. Fast-forward two years and here I am, studying pain-based neurotransmission in the peripheral nervous system, learning countless new things every day, and strongly advocating for science communication to be brought more to the fore of the goals of the scientific community, as you never know who may be inspired to embark upon their own journey into scientific research.
Alice Gregorie, PhD student, University of Leeds, UK.
Hurling this greeting out into the world is usually one of the first things you do when learning a new programming language. And in a way, that is the very thing I'm trying to do right now – only instead of communicating with a rather stupid machine, I am communicating with you, my reader on the other side of this screen.
Oh, there is also, of course, the small matter of our topic – instead of making you quickly calculate in your head many very simple things, I actually want to “communicate,” a word that comes from the Latin word communicatus, which means “ ‘to share, communicate, impart, inform,’ literally ‘to make common,’ related to communis ‘common, public, general.’ ” And that is a whole different story.
I am 28 years old and grew up in an area of Germany where people are very money conscious. I always felt that the best value for money I ever got on anything was ibuprofen. Mind you, I never had much pain in my life – just a few mild episodes of migraine when I was a teenager, and the random assortment of bruises and sprained ankles and infections – but my pains were and are all-so-very temporary. It wasn't until I made chronic pain my PhD research topic two years ago that I noticed just how extraordinary that is – how unbelievably lucky I am. When I'm in pain, I pop a pill and can be sure my aches will be gone in a few minutes. I don't have to come to terms with suffering from pain or suffering from my analgesics' side effects. I can be sure that tomorrow, or in a week or in a month, I will be back to normal again. No one shared with me what it was like to be in pain each hour of every hour. Or maybe I just never listened.
But now, I want to listen. Now I want to know. I have so many questions; I understand so little! My early background is in psychology, and later on in neuroscience, so I was amazed to learn that it is considered bad form to speak of “subjective pain” or to suggest that pain is all in the head. Well, of course it is! And of course, it absolutely is not. Pain is intimate and raw and visceral in a way that few things can be. From a scientific viewpoint, all that is just plain evolution. But for the human being? It is existential. It shapes the concept of self. I never knew it before starting to speak to patients who come to the hospital to participate in my study. Wrong – before starting to listen.
And now, as a Correspondent for the Pain Research Forum, I want to “make common” again, to listen more, this time by writing and by reflecting. I feel strongly about science communication being a two-way street. It is not about us scientists squeezing a tiny bit of time out of our oh-so-busy schedules to educate what is often inaccurately described by others as a clueless public. It is about the public educating us. It is about us sharing our questions. We do not have all the answers. But we might have some of the right questions.
I have so many questions, and I am eager to share them with you. And if I am very lucky, you might want to share some of yours with me?
So Hello, World – tell me everything!
Leave a comment below, drop me a line by email (malika.renz@zi-mannheim.de) or on Twitter (@vagemutig). And don't worry; not all my posts are going to be semi-sentimental pieces that dreamed of becoming poetry. There will be lots of cool, hard science as well!
Malika Renz, PhD student, Central Institute for Mental Health, Mannheim, Germany.
A Biomedical Engineering Approach to Developing New Osteoarthritis Treatments 
I’m Britt Knight, a postdoctoral trainee in Dr. Lakshmi Nair’s lab at the Connecticut Convergence Institute at the UConn Health branch of University of Connecticut in Farmington, CT. My scientific training spans the fields of psychology and neuroscience, and currently I’m learning about the field of biomedical engineering. Specifically, my research focuses on the design and application of biomaterial drug delivery systems for localized pain treatments using animal models of osteoarthritis.
Osteoarthritis is a prevalent condition that results from degeneration of the cartilage or soft tissues between joints, and is a major contributor to pain and disability among older adults. Current estimates suggest that by 2030, 25% of the adult population with have an arthritic diagnosis. Common strategies used to manage joint pain include lifestyle changes (e.g., diet or physiotherapy), therapeutic injections (e.g., peripheral nerve block, corticosteroids, or hyaluronic acid), and joint replacement surgery. While these treatment strategies are beneficial for treating pain in the short term, repeated exposure to therapeutic doses of many pain-relieving drugs can result in adverse effects such as addiction and/or physical damage (i.e., toxicity to various organ systems). Therefore, as the patient population and the burden of pain associated with osteoarthritis increase, the need for treatments that can provide safe, effective, and sustained pain relief is critical.
Beyond conducting experiments and mentoring students in the laboratory, I also help lead a career development seminar series, referred to as Beyond the PhD, for upper-level undergraduates and graduate students in STEM (science, technology, engineering, and mathematics). In my free time I enjoy bike riding, playing Frisbee, and finding new books at my local library. Also, a fun fact is that I am a huge nerd when it comes to movie scores and soundtracks, and I love to listen to these themes when I write. For instance, I listened to John Powell’s soundtrack album from Call of the Wild (2020) while I wrote this article. As a scientist, I believe that science communication is an excellent way to share your voice and expertise with audiences beyond the immediate reaches of your research community.
Britt Knight, postdoctoral trainee, University of Connecticut, US.
Can We Enhance Existing Treatments for Pain? 
I am thrilled to take part in the PRF community. I am currently a doctoral candidate at Neuroscience Research Australia (NeuRA) and the University of New South Wales (UNSW). I have been interested in pain communication for several years.
As a clinician, I had a simple but impactful experience that influenced my interest in pain communication. Some years ago, in the middle of a treatment session, a patient looked into my eyes and said, “Do you know the worst thing about having pain?” I did not know what to say, and he continued, “The worst thing about having pain for years is feeling lost.” At that time, I realized that I should devote my attention to developing communication skills to inform diagnosis, prognosis, and pain management in a clear, realistic, and empowering way.
I was so lucky! Some clinicians and researchers had been dedicating their lives to understanding and developing effective strategies to communicate about pain to different audiences. I wanted to learn more to treat my patients and perhaps contribute to the science of pain. I found a great supervisor in Brazil, Leo Costa, who was happy with my research proposal. Inspired by the work of Mark Jensen and Lorimer Moseley, I proposed a study to investigate the effect of embedding additional communication skills into pain science education. My supervisor and I worked together on this project for two years. This experience opened a new chapter in my life.
To learn more about science and how treatments work for pain, I came to Australia to do my PhD with two inspiring supervisors, James McAuley and Sylvia Gustin, at NeuRA. My PhD is centered on optimizing treatments for low back pain using process evaluation. I believe that we can enhance the effectiveness of pain treatments by identifying important features in existing and new interventions for low back pain. Randomized controlled trials and systematic reviews are published every day to show WHETHER and to what extent an intervention affects pain and disability. However, traditional analyses in clinical trials do not show anything about HOW these treatments work. In my PhD, I use quantitative and qualitative methods alongside clinical trials to understand how treatments achieve their effects for chronic pain.
In the field of research, we are always finding interesting pieces of this amazing puzzle called life. I hope to share with you some exciting things about pain research. I hope to keep in touch with you through these posts and maybe also on Twitter @rodrizzo_pain.
Rodrigo Rizzo, doctoral candidate, Neuroscience Research Australia (NeuRA) and the University of New South Wales (UNSW).
From Potential Zombie Creator to Chronic Pain Researcher 
“Are you responsible?” I received this message from a couple of friends last year, after the Mexican government announced the lockdown and new security measures when the COVID-19 pandemic reached our country. So my answer was, “Nope, you know my pandemic will be about zombies.”
To be honest, the Resident Evil video game series was truly my first approach to science. The idea of a virus causing a zombie outbreak completely blew my mind when I was seven years old. Thus, I wanted to know everything about cell biology, chemistry, microbiology…. That was the first step to become a nerdy wannabe-scientist, and that is why my close friends still joke about my potential to create and release a zombie virus:
You wanted to destroy humanity with zombies, but now you are trying to help everyone who is suffering from pain!
Well, I first need to understand all about the neurobiology of pain in order to develop painless, ravenous creatures (wink, wink).
My interest in pain research started when my mom was diagnosed with fibromyalgia. When I moved to Mexico City to obtain my bachelor’s degree in biological and pharmaceutical chemistry, I could not find too much information about this rare disease affecting my mother, even with free access to the Internet and an enormous library. Fibromyalgia was barely known and still classified as a psychiatric disorder.
Then I started my journey as a graduate student in the neuropharmacology and experimental therapeutics program at the Center for Research and Advanced Studies (Cinvestav, in Spanish) in Mexico City. With unknown etiology and few animal models available, fibromyalgia syndrome is quite challenging to study. My first investigation concerned the participation of spinal and peripheral α5 subunit-containing GABAA receptors and chloride homeostasis in a reserpine-induced fibromyalgia-like model in rats.
My current research as a PhD student is focused on pharmacological, molecular, and electrophysiological approaches – still working on the last – to evaluate the role of spinal dopamine receptors in the same animal model of fibromyalgia. This type of pain has always been my main interest, but I am also interested in other pain disorders such as neuropathic pain, migraine, stress-induced pain, and diabetic neuropathy. And sure, I would like to investigate gene therapy (maybe with viruses!) for chronic pain in the near future.
With all the misinformation about the pandemic invading global media, I believe science communication is an essential part of a researcher’s duty. I am thrilled to be part of the PRF Virtual Correspondents Program, as this is the perfect opportunity to learn about communication, improve my skills, share information, reach a broad audience, and have some fun!
Stay tuned! You can follow me on Twitter @atarii_cuellar.
Yarim De la Luz-Cuellar, PhD student, Center for Research and Advanced Studies, Mexico City, Mexico.
Hello, PRF readers. I am Bhushan Thakkar, a PhD student in the Department of Physical Therapy at Virginia Commonwealth University (VCU), where I am working with Dr. Edmund Acevedo in the Department of Kinesiology and Health Sciences. I received my bachelor’s degree in physical therapy (PT) in India and then my master's degree in PT at the MGH Institute of Health Professions in Boston, which also marked my first time coming to the US.
After working a few years as a PT, I decided to come to VCU to get my PhD. My journey in graduate school at VCU has been a long and arduous one, changing mentors and research topics twice but apparently the third time is the charm, and I am fortunate to be working in the areas of non-invasive brain stimulation and chronic pain. I have been fascinated with the mechanisms that drive chronic pain and how biopsychosocial determinants of health intersect in the development of chronic pain, which is a complex problem not just nationally but globally. I strongly believe that despite significant advancements in the understanding of the neuroscience underlying chronic pain over the past few decades, the translation of these advancements into clinical interventions that are feasible for clinicians and patients continues to lag. Effective dissemination of information to patients, public health officials, and healthcare professionals is a critical first step to address this gap.
My current research focuses on using transcranial magnetic stimulation as a treatment to alter pain perception in chronic pain patients with diabetic neuropathy. My career goals are to further advance the translation of the neurophysiological, neurochemical, and psychophysical mechanisms underlying chronic pain, specifically neuropathic pain, into clinical interventions that are feasible for clinicians and patients.
I am also a research coordinator investigating the role of biological and psychosocial factors during recovery in pregnant and postpartum women with substance use disorders in the IVY (In Recovery) Lab at VCU, led by Dr. Caitlin E. Martin.
Although my wife and family reside in India, I am in great company with my cat, Roxie. I am an avid runner, having run three marathons and training for the fourth one in December of this year. I love to bake, and Linkin Park is my favorite music band.
Personally, I am an avid reader of the PRF correspondent blogs, and PRF and RELIEF newsletters, webinars, and podcasts. I am excited and looking forward to being a part of the PRF Correspondents Program, which will give me a platform to engage with the international scientific community. In doing so, I intend to dive deeper into various pain research areas and network with key stakeholders. Stay tuned for some content I am developing on topics and issues that are interesting to me, and some that don’t always get the spotlight in pain research that I am excited to share with you.
Bhushan Thakkar, PhD student, Department of Physical Therapy, Virginia Commonwealth University, US.
Bonjour! My name is Valérie Bourassa, and I am a PhD candidate in neuroscience at McGill University, Montreal, Canada. For a few years now, I have been investigating mechanisms that contribute to chronic pain in osteoarthritis under the supervision of Dr. Alfredo Ribeiro-da-Silva.
I am quite passionate about science communications and science education. During my graduate studies at McGill, I have been involved with the Office of Science Education as a science education fellow to train and teach instructors and graduate student teaching assistants how to best communicate with their students and to improve their science teaching practices.
Now that my doctoral studies are near completion, I have enrolled in the Chronic Pain Management Certificate at McGill University to expand my expertise in pain to clinical practice. Joining as a fundamental scientist, I immediately noticed barriers in communication and diverging perspectives with my clinical colleagues. As my professional goal is to pursue the study and management of chronic pain as a clinician in an interdisciplinary pain clinic, I actively seek to improve my practices and those of my colleagues regarding science education. I am delighted to have the opportunity to participate in the Pain Research Forum Virtual Correspondents Program to improve, solidify, and increase the visibility of those practices.
When I am not doing science, you can find me on Twitter @ValerieBourass1, or enjoying some quality time with my two cats, Wesley and Rogelio.
Valérie’s Book Club
Do you want to read more about how science communication can impact knowledge and discoveries? Join my book club! Every week, I will be recommending a book that illustrates how collaborations between patients and scientists can make immense contributions to the advancement of science and medicine.

This week’s recommendation is Hidden Valley Road: Inside the Mind of an American Family, by Robert Kolker (2020). When Don and Mimi Galvin moved to Colorado in the 1940s to live the American dream, they couldn’t have imagined that their family would become the most-studied genetic pool in mental illness research. Between 1945 and 1965, Don and Mimi had 12 children, including 10 boys and two girls. Over the years, six of their boys would receive the diagnosis of schizophrenia. Why did this happen to them? Hidden Valley Road shares the emotional and physical battles of a family suffering in a society and healthcare system unable and unwilling to treat mental illness, and how their tenacity contributed to progress in mental health diagnosis and treatment.
Valérie Bourassa, PhD candidate, McGill University, Montreal, Canada.