Introduction
Our life is determined by expectations, fluctuating between hope and fear, but how positive or negative these expectations are largely depends on experiences we have had and remember as well as the context in which they appear. This applies to all areas of life, including medicine, and it is these expectations and prior experiences that patients take with them when they go to a doctor or therapist. The following fact sheet will explain how our brain and body react to placebo and nocebo effects, how expectations can modulate pain and analgesic treatment outcomes and what role the patient-physician relationship plays in this regard.
What are placebo and nocebo effects and how do they contribute to active pharmacological treatments?
The placebo effect is a positive physical or psychological change that occurs after taking medication without an active ingredient such as a sugar pill, or after a sham treatment such as simulated surgery. With respect to pain these effects are called placebo analgesia or hypoalgesia, i.e., pain relief [1]. These placebo effects are driven by a positive expectation that we have regarding a treatment [2]. Importantly, positive expectations can also substantially modulate the efficacy and tolerability of conventionally prescribed, intrinsically effective (e.g., pharmacologically active) treatments. For example, we might react well to a certain pain medication, because we remember that it relieved our back pain in the past (see Figure 2 for an overview of factors influencing placebo and nocebo effects).
On the other hand, treatments can also be influenced by negative expectations, called nocebo effects [1]. If a patient discovers, for example, that a medication has been tolerated poorly by someone they know, the same medication is likely to be less effective or cause side effects in this patient. This is called nocebo hyperalgesia, i.e., an increase of pain.
The potent analgesic remifentanil is a very impressive example of expectation effects (see Figure 1). Positive treatment expectations made it twice as effective at relieving pain, whereas negative expectations, coupled with worry that the pain could get worse, ensured that it lost its effect [3]. Such modulatory effects of expectation have also been shown for many other drugs. Expectation effects can also accelerate healing after surgery, manual therapy, and psychological interventions.
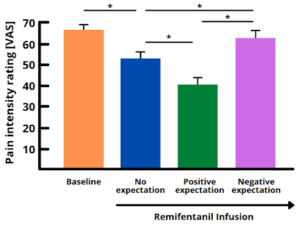
Figure 1. The above bar chart shows the efficacy of the potent analgesic remifentanil in participants with different expectations who received heat pain stimuli. Its effect on pain intensity ratings can vary considerably, depending on whether the patient receives the remifentanil infusion with no expectations (blue), positive expectations (green) or negative expectations (purple) of the medication. Positive, analgesic expectations make it more effective, whereas negative, hyperalgesic expectations can reverse its effect, as if the participant had not taken any medication at all. This figure was created by the fact sheet authors using free designs in Canva (https://www.canva.com/), but is based on a figure from [2]. * indicate significant differences between the mean pain intensity ratings of two conditions. VAS = visual analogue scale.
In some cases, there is even a placebo effect when patients know they are taking a pill without an active ingredient, so-called ‘open-label placebos’ [4]. They are an area of vivid ongoing research, but initial evidence supports the notion that they can support treatment and healing in combination with established and proven gold-standard treatments [5]. Patient-provider interactions are considered only one of many factors contributing to their successful application.
What happens in the brain and body during placebo and nocebo effects?
Expectation effects are no coincidence, but instead based on complex psychoneurobiological processes in the brain [6]. Simply believing that a certain treatment is effective has been shown to activate mechanisms in the body that improve treatment outcome. This can be described as a kind of “internal pharmacy”. Imaging techniques show that certain areas of the brain, e.g., pain relief systems, are activated during this process. For example, if a patient expects a treatment to alleviate pain, pain-relieving substances called endogenous opioids, are released in the brain, and can even alter onward transmission of the pain stimulus in the spinal cord. Placebo and nocebo effects are therefore not only limited to subjective feelings and symptoms such as pain or mood. They can affect many physiological processes from respiration and digestion to the immune system [7].
How can we use the effects of positive and negative expectation (aka placebo and nocebo) to improve treatment?
In clinical routine the power of expectation should be systematically harnessed to maximize the efficacy and tolerability of treatments as well as the compliance of patients to adhere to prescribed treatment regimens [8]. But how can this be done? The expectations a patient develops are modulated by various factors, for example, what the doctor says, what the patient believes, remembers, or observes, as well as how the patient generally reacts to treatments (see Figure 2). Here, health professionals have the chance to crucially influence the way a patient thinks about a treatment when leaving their practice or the hospital.
Figure 2. Patients’ expectations about a certain treatment are shaped by various factors, such as verbal suggestions by physicians and health care professionals, the context in which information about the treatment is communicated, one’s own knowledge, beliefs and past experiences with certain medication and treatments, and one’s dispositional traits. This figure was created by the fact sheet authors using free designs in Canva (https://www.canva.com/).
In this regard, especially the patient-physician interaction is a powerful modulator: Communication affects whether and how well medication works and how well it is tolerated. Patients who are convinced by a treatment usually benefit more from it. It is therefore important for physicians to take the time to build trust and explain the objectives and benefits of a treatment. Likewise, just the way a doctor phrases something plays a key role. You can either tell the patient that “10% of people experience side effects” or that “90% of people tolerate the medication very well”. It is not about withholding or sugar-coating information, but instead sharing it in a way that makes patients less anxious.
How does a physician, physiotherapist or nurse inform the patient about a treatment? What are their exact words? How crucial are gestures and facial expressions? Table 1 summarizes some of the strategies that physicians and health care professionals can pay attention to when interacting with patients and communicating treatments.
| Strategies for physicians and health care professionals to manage patients’ expectations. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Table 1. This table shows some of the strategies that physicians and health care professionals can pay attention to when aiming to promote positive expectations (leading to placebo effects) and avoid negative expectations (leading to nocebo effects). This table was created by the fact sheet authors, but based on the information in [2].
Challenges and future directions
Individual expectations and experience of patients are particularly important. In the future, health care professionals should pay more attention to these when selecting and communicating treatments [9]. The aim must be for patients to start a treatment with positive expectations and to avoid negative expectations. These ‘default’ expectation settings could reduce the required dose of a medication and therefore minimize the risk of side effects.
These findings are also of interest to the pharmaceutical industry when developing new treatment approaches, and this applies to active ingredients, form of administration (e.g., pill, cream, or injection), dosage and patient information.
Placebo and nocebo effects work, but individual response varies as a function of symptoms, disease state, treatment, and person-centered factors, such as genetics and personality. Some people are inherently optimistic and open-minded, whereas others are more anxious and skeptical. Furthermore, expectations can vary with the existing condition, for example, if a person experiences chronic vs. acute pain. Physicians and clinicians could therefore pay more attention to characteristics of individual patients before inducing certain expectations about a treatment, be they positive or negative [10]. Expectations should always be tailored to the individual patient and their history.
Current research efforts aim at identifying psychological and neurobiological factors that allow for the prediction and individually tailored use of expectation effects to optimize treatment outcomes in a personalized manner [2]. Such strategies may prevent or reduce the burden of unwanted side effects and misuse of analgesics, particularly of opioids.
ACKNOWLEDGEMENTS
This fact sheet has been inspired and supported by SFB/TRR 289 Treatment Expectation funded by the German Research Foundation (Project-ID 422744262). For the interested reader please see www.treatment-expectation.de.
REFERENCES
[1] Colloca L, Barsky AJ. Placebo and Nocebo Effects. N Engl J Med 2020;382(6):554-561.
[2] Bingel, U. Placebo 2.0: the impact of expectations on analgesic treatment outcome, Pain 2020;161:48-56.
[3] Bingel U, Wanigasekera V, Wiech K, Mhuircheartaigh R, Lee MC, Ploner M, Tracey I (2011) The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Science Transl Med (3)70:70ra14.
[4] Belcher AM, Cole TO, Greenblatt AD, Hoag SW, Epstein DH, Wagner M, Billing AS, Massey E, Hamilton KR, Kozak ZK, Welsh CJ, Weintraub E, Wickwire EM, Wish ED, Kaptchuk TJ, Colloca L. Open-label dose-extending placebos for opioid use disorder: a protocol for a randomised controlled clinical trial with methadone treatment. BMJ Open 2019;9(6):e026604.
[5] von Wernsdorff M, Loef M, Tuschen-Caffier B, Schmidt S. Effects of open-label placebos in clinical trials: a systematic review and meta-analysis. Sci Rep. 2021;11(1):17436]. Sci Rep. 2021;11(1):3855.
[6] Petrie KJ, Rief W. Psychobiological Mechanisms of Placebo and Nocebo Effects: Pathways to Improve Treatments and Reduce Side Effects. Annual review of psychology 2019;70:599-625.
[7] Skyt I, Lunde SJ, Baastrup C, Svensson P, Jensen TS, Vase L. Neurotransmitter systems involved in placebo and nocebo effects in healthy participants and patients with chronic pain: a systematic review. Pain 2020;161(1):11-23.
[8] Enck P, Bingel U, Schedlowski M, Rief W. The placebo response in medicine: minimize, maximize or personalize? Nat Rev Drug Discov 2013;12(3):191-204.
[9] Crum A, Zuckerman B. Changing Mindsets to Enhance Treatment Effectiveness. Jama 2017;317(20):2063-2064.
[10] Schedlowski M, Enck P, Rief W, Bingel U. Neuro-Bio-Behavioral Mechanisms of Placebo and Nocebo Responses: Implications for Clinical Trials and Clinical Practice. Pharmacol Rev 2015;67(3):697-730.



