Physical Activity and Exercise Defined
Physical activity is defined as any bodily movement produced by skeletal muscles that requires energy expenditure [1] and includes purposeful activity performed with daily routines and structured exercise programs devoted to the improvement or maintenance of fitness, health, and wellness. Exercise is a type of physical activity that is planned, structured, and often associated with repetitive movement. Physical activity and exercise play a key role in the prevention, management, and rehabilitation of multiple disease processes in conjunction with other healthy lifestyle behaviors and medical treatments.[2] Evidence supporting the benefits of regular physical activity in the prevention and treatment of chronic diseases has prompted increased integration and promotion of physical activity as a standard part of disease prevention and medical treatment.
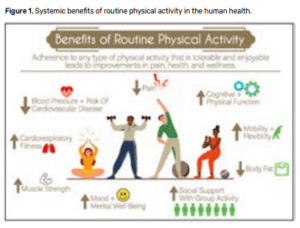
Exercise can improve cardiorespiratory (aerobic) and muscular fitness, mobility/flexibility, and body composition.[1-3] Multiple components are considered when prescribing an individualized exercise program including the frequency (how often), intensity (how hard), time (duration or how long), type (mode or what kind), and progression (exercise advancement or regression). However, the optimal type or amount of exercise for pain management will vary by individual. Not all individuals respond to exercise intervention in a similar manner, and some with chronic pain may experience pain exacerbation following an acute bout of exercise. A short-lived, mild increase in pain after an acute bout of exercise may be expected, particularly in those who are inexperienced with exercise. This expectation should be discussed with patients and managed by the integrative pain care team. In addition, accommodations to the exercise plan should be considered depending on individual characteristics such as health status, physical ability, age, and clinical conditions rather than ceasing treatment. Predictors of poor outcome include high pain Intensity, longer pain duration, multiple-site pain, previous pain episodes, anxiety/depression, higher distress, poor coping strategies, lower social support, older age, higher baseline disability, greater movement restriction, high pain catastrophizing and high fear of movement/pain.[4-7] Individuals with these characteristics may require additional support and may benefit from a slowly progressing program. It is important to mention that physical activities or exercise programs can be done individually or in groups with other people with similar conditions, which adds a social component and tends to increase motivation and create a more encouraging environment.
Mechanisms of Action of Physical Activity and Exercise
Exercise elicits multimodal effects across the biopsychosocial spectrum. Research in animals indicates exercise may lead to alterations in both the peripheral and central nervous system, peripheral tissues, and immune system.[8,9] The human literature corroborates these findings as those who partake in regular physical activity demonstrate reduced pain, less inflammation, and improved tissue healing.[9-12] In addition, regular exercise has been shown to improve psychological comorbidities (fear of movement, anxiety, depression), mood, sleep quality, physical and cognitive function.[1,2,13]
Clinical Evidence for the Effect of Physical Activity and Exercise on Pain
Increasing physical activity through exercise is recommended as a preventive measure to reduce risk of developing chronic pain and as a front-line treatment to reduce pain and improve function and quality of life in people living with chronic pain (see Figure 1).[14]
Prevention: Physical inactivity and sedentary behavior are detrimental to health [13,15] and are risk factors for the development of chronic pain; for example, those who exercise regularly report less pain over a 12-month period and are less likely to develop chronic pain compared to sedentary individuals.16 In addition, regular physical activity and exercise helps to prevent other noncommunicable diseases such as heart disease, stroke, diabetes, several cancers, mental health, quality of life and well-being.
Treatment: Several reviews have demonstrated physical activity and exercise lead to favorable improvements in self-reported pain, physical function, psychological function, and quality of life across multiple pain conditions including, osteoarthritis, low back pain, fibromyalgia, and others.[13] While variable outcomes and effect sizes exist in the literature, inconsistencies can be potentially attributable to small sample sizes, underpowered studies, limited long-term follow-up, and adherence and duration of exercise intervention.
Practitioners that Promote and Prescribe Physical Activity and Exercise
Many practitioners educate patients about the benefits of physical activity and exercise for pain management and health, while others actively prescribe, modify, and progress specific exercise recommendations to patients as part of their plan of care (physical therapist, chiropractic, physical education professionals, others). Integration of physical activity and exercise as part of a comprehensive management plan requires all practitioners to encourage physical activity and exercise as an intervention and to understand the need for an individualized and person-centered approach. It is important to reinforce that a therapeutic exercise program should have some professional supervision to select activities that are meaningful, achievable, and enjoyable for each person and to reduce the chance of adverse effects such as pain exacerbation, overload, or muscle/joint injury.[3,17]
Physical Activity and Exercise within an Integrated Care Approach
All clinicians that are part of integrated health teams should understand the benefits of physical activity and exercise intervention and that the response to an acute bout may vary among patients. The integrated pain care team must address general and specific barriers for engaging in physical activity and exercise including pain with activity, fatigue/tiredness, not knowing what dosage or type is optimal, activity preference, individual beliefs, and negative expectations of physical activity and exercise from prior experiences. While some patients will experience a reduction or no change in pain, others may experience increased pain after performing a single bout of physical activity or exercise. Pain in response to initial exposure to activity and exercise presents a barrier to adherence and many find it difficult to maintain routine physical activity and exercise prescribed by health care professionals. The pain response to acute activity and exercise should be anticipated and managed by the integrated care team. Use of motivational strategies, behavior change interventions, social support, goal setting, individually paced exercise, education, and individual preference enhance exercise adherence.[18] Additional therapeutic modalities provided as part of an integrative pain management model may also assist in managing exercise-induced symptoms including transcutaneous electrical nerve stimulation, manual therapies, acupuncture, thermal therapies and others. Periodic follow-up appointments during a supervised period of exercise may allow for troubleshooting and recommendations to minimize barriers affecting exercise progression and exercise behavior maintenance as even small amounts of physical activity are beneficial.[19]
A comprehensive pain treatment program should incorporate a person-centered exercise program that is tailored to the individual needs, expectations, and ability of the patient and helps reduce barriers to increased physical activity – specifically pain with exercise. The treatment goal should be to establish a long-term exercise program that leads to long-term benefits of improved pain, function, mood, and quality of life. To promote compliance and achieve longterm goals, patients should receive complementary pain treatments to address discomfort with exercise, and the education and expectations from all practitioners of the integrated pain team should be consistent. Receiving congruent clinical opinions, narratives of realistic expectations, and exercise prescription modifications among the integrated pain team will help promote compliance and reduce negative beliefs associated with exercise intervention.
References
- WHO Guidelines Approved by the Guidelines Review Committee. WHO Guidelines on Physical Activity and Sedentary Behaviour. WHO Guidelines Approved by the Guidelines Review Committee. Geneva: World Health Organization 2020.; 2020.
- American College of Sports Medicine Guidelines for Exercise Testing and Prescription. 10th Edition ed: Wolters Kluwer; 2017.
- Thompson WR, Sallis R, Joy E, Jaworski CA, Stuhr RM, Trilk JL. Exercise Is Medicine. Am J Lifestyle Med. 2020;14(5):511-23.
- Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30(1):77-94.
- Shaw WS, Means-Christensen AJ, Slater MA, Webster JS, Patterson TL, Grant I, et al. Psychiatric disorders and risk of transition to chronicity in men with first onset low back pain. Pain Med. 2010;11(9):1391-400.
- Lewis GN, Rice DA, McNair PJ, Kluger M. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. 2015;114(4):551-61.
- Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. The journal of pain : official journal of the American Pain Society. 2016;17(9 Suppl):T70-92.
- Lesnak JB, Sluka KA. Mechanism of exercise-induced analgesia: what we can learn from physically active animals. Pain Rep. 2020;5(5):e850.
- Sluka KA, Frey-Law L, Hoeger Bement M. Exercise-induced pain and analgesia? Underlying mechanisms and clinical translation. Pain. 2018;159 Suppl 1(Suppl 1):S91-S7.
- Nieman DC, Wentz LM. The compelling link between physical activity and the body’s defense system. J Sport Health Sci. 2019;8(3):201-17.
- Wun A, Kollias P, Jeong H, Rizzo RR, Cashin AG, Bagg MK, et al. Why is exercise prescribed for people with chronic low back pain? A review of the mechanisms of benefit proposed by clinical trialists. Musculoskeletal science & practice. 2021;51:102307.
- Beckwée D, Vaes P, Cnudde M, Swinnen E, Bautmans I. Osteoarthritis of the knee: why does exercise work? A qualitative study of the literature. Ageing Res Rev. 2013;12(1):226-36.
- Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;1:CD011279.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain–United States, 2016. JAMA. 2016;315(15):1624-45.
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219-29.
- Landmark T, Romundstad PR, Borchgrevink PC, Kaasa S, Dale O. Longitudinal associations between exercise and pain in the general population–the HUNT pain study. PLoS One. 2013;8(6):e65279.
- Ferreira GE, Howard K, Zadro JR, O’Keeffe M, Lin CC, Maher CG. People considering exercise to prevent low back pain recurrence prefer exercise programs that differ from programs known to be effective: a discrete choice experiment. J Physiother. 2020;66(4):249-55.
- Meade LB, Bearne LM, Sweeney LH, Alageel SH, Godfrey EL. Behaviour change techniques associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain: Systematic review. British journal of health psychology. 2019;24(1):10-30.
- Coleman CJ, McDonough DJ, Pope ZC, Pope CA. Dose-response association of aerobic and muscle-strengthening physical activity with mortality: a national cohort study of 416 420 US adults. Br J Sports Med. 2022.



