Introduction
Chronic pain burdens many people but access to guideline-based and long-term treatment remains challenging. Contemporary gold-standard treatment is based on an interdisciplinary multidimensional or multimodal therapy. It fosters patients’ empowerment through physiotherapy, psychotherapy, education, and behavioral change. Increasingly, these include broader health considerations e.g., addressing sleep disturbance, weight, stress, and social engagement.
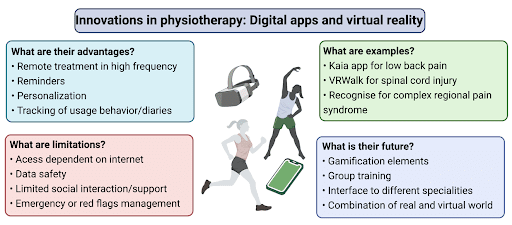
Digital modalities in physiotherapy include medical apps (mHealth apps), telemedicine as well as augmented (AR) and virtual reality (VR) tools. They are promising tools to bring pain knowledge into practice. Delivered though smartphones, tablets, and other digital media, mHealth apps can provide effective interdisciplinary treatment to patients with chronic pain independent of physical location or temporal synchrony with providers (Schäfer A et al. 2018). Supporting their use, a recent meta-analysis of 12 RCTs suggested that mHealth applications have a small positive effect in chronic pain reduction (Pfeifer et al. 2020). However, the quality of evidence was low due to lack of blinding and small sample sizes. Telemedical tools can advance treatment by fostering cooperation among specialists using, e.g., digital tools for clinical decision making in diagnostics and treatment (Toelle et al. 2019; Priebe et al. 2020a).
Virtual reality (VR) also shows initial promising results in clinical studies. VR integrates mechanisms of distraction, behavioral modification, relaxation, and education in an engaging, condition-relevant manner. VR shows substantial efficacy in acute pain relief and – utilizing embodiment capabilities – is increasingly applied in studies for chronic pain conditions, in particular neuropathic pain, and low back pain (Trost et al. 2021a). However, as with digital apps, greater research is needed on long-term outcomes, because current research is limited by non-standardized methodology and small, uncontrolled designs.
Requirements and advantages for digital physio- and multidimensional pain therapy
Patient data security is an obligatory requirement. Secondly, a connection of real and digital world can foster adherence: some apps include online coaching and others combine physical appointments with digital training plans. All apps should provide an emergency management plan – e.g., 24/7 phone numbers to local health care providers or other emergency contacts.
Obvious advantages are high-frequency and remote training options which can be further fostered by digital reminders, gaming, or competitive elements. Treatment diaries can be shared with the physiotherapist. Also, adherence tracking can be included if, e.g., outside activities like Nordic walking or cycling are part of the program. Finally, the use of mHealth apps may enable engagement with broader aspects of pain care e.g., addressing sleep or mood as part of physiotherapy-led pain care.
Barriers and limitations of digital apps in physiotherapy and multimodal pain therapy
While many apps also function offline, most require a robust internet connection. Given their recognized utility, health insurance plans in some countries allow for prescription of apps, thus addressing potential issues of cost. But, physiotherapists’ views of mHealth apps are not unequivocally positive: the lack of contextual factors, manual treatment, and interaction with other patients weaken the alliance between patient and physiotherapist (Martínez de la Cal et al. 2021). Evolving technology is increasingly able to enrich digital intervention with contextual factors such as verbal communication (e.g., paraphrasing and linguistic reciprocity, clear instructions, expression of support) and non-verbal communication (e.g., affirmative head nodding, eye contact, open posture), tailored to the individual patient (Turolla et al. 2020).
The growth of digital and virtual technologies has also facilitated novel interprofessional collaborations between researchers, clinicians, and technology developers (often businesses); such collaborations call for understanding of the benefits and drawbacks of specific design choices with respect to cost, utility, and ease of deployment, as well as intellectual property arrangements.
Empirical Rigor
Despite substantial progress, the field of digital health and pain rehabilitation calls for greater methodological rigor to allow firm conclusions regarding the utility of various modes of intervention. This includes better-powered and appropriately controlled studies, as well as standardized metrics which allow replication and comparison across studies. This is made challenging by rapidly evolving technological capabilities and, in rapidly evolving areas like VR, lack of firm theoretical scaffolding (Trost et al. 2021a).
Examples
The Kaia App successfully implements current treatment guidelines for low back pain with three therapy modules: physiotherapy/physical exercise, mindfulness and relaxation techniques, and back pain-specific education (Toelle et al., 2019; Priebe et al., 2020a; Priebe et al., 2020b). A personalized program uses the patient´s status of knowledge, practice, and progress to constantly adapt exercise. A control system via the camera of the mobile phone catches the movements of the patient, models them in 3D and provides feedback to secure optimized exercise execution.
Home-based VR treatment of neuropathic pain following spinal cord injury employs an immersive, interactive virtual reality walking intervention (VRWalk) as an extension of visual feedback therapies (e.g., mirror therapy). Participants direct their virtual gait using naturalistic arm activity captured by the VR system, allowing them to ambulate through the virtual environment and collect points. This not only decreases neuropathic pain but also shows evidence of reversing neuroplastic changes (Trost Z et al. 2021b).
Complex Regional Pain Syndrome (O’Connell et al. 2013) and phantom limb pain (Batsford et al. 2017) can be treated with graded motor imagery: The Recognise App implements the first two stages: left/right discrimination and motor imagery. Especially in high frequency training intervals with therapy tools like pictures, mHealth apps can provide a manageable all-day training possibility.
The future
Many patients are quite excited when apps are introduced into the treatment – especially when they are easy to use (summarized in Figure 1). However, motivation and adherence are also challenges in the real world. Group training – possibly combined with gamification elements or real-world classes – could utilize the best of both worlds. The integration of augmented or virtual reality can increase motivation and adherence in a growing digital generation. These new technical devices use distraction and embodiment into various Avatars to create new behaviors and increase training efficiency (Lindner et al. 2020). In the future, interdisciplinary health care teams could use the data together with the patient to plan the treatment and integrate other modules from medicine and psychotherapy to “live” the biopsychosocial model of chronic pain.
AUTHORS
Janosch A. Priebe & Thomas R. Toelle, Center of Interdisciplinary Pain Medicine, Department of Neurology, Klinikum rechts der Isar (MRI), Technical University of Munich, Germany
Niamh Moloney, Macquarie University, Sydney, Australia
Zina Trost, Virginia Commonwealth University, Richmond, VA, USA
Axel Schäfer, University of Applied Sciences and Art, Hildesheim, Germany
Stefan Lindner & Heike L. Rittner, Center for Interdisciplinary Pain Medicine, Dept Anesthesiology, University Hospital of Wuerzburg, Germany
REFERENCES
- Batsford S, Ryan CG, Martin DJ. Non-pharmacological conservative therapy for phantom limb pain: A systematic review of randomized controlled trials. Physiother Theory Pract. 2017 Mar;33(3):173-183
- Lindner S, Latoschik ME, Rittner H. Virtual Reality als Baustein in der Behandlung akuter und chronischer Schmerzen [Use of Virtual Reality as a Component of Acute and Chronic Pain Treatment]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2020 Sep;55(9):549-561.
- Martínez de la Cal J, Fernández-Sánchez M, Matarán-Peñarrocha GA, Hurley DA, Castro-Sánchez AM, Lara-Palomo IC. Physical Therapists’ Opinion of E-Health Treatment of Chronic Low Back Pain. Int J Environ Res Public Health. 2021 Feb 16;18(4):1889
- O’Connell NE, Wand BM, McAuley J, Marston L, Moseley GL. Interventions for treating pain and disability in adults with complex regional pain syndrome. Cochrane Database Syst Rev. 2013 Apr 30;2013(4):CD009416
- Pfeifer AC, Uddin R, Schröder-Pfeifer P, Holl F, Swoboda W, Schiltenwolf M. Mobile Application-Based Interventions for Chronic Pain Patients: A Systematic Review and Meta-Analysis of Effectiveness. J Clin Med. 2020 Nov 5;9(11):3557
- Priebe JA, Haas KK, Moreno Sanchez LF, Schoefmann K, Utpadel-Fischler DA, Stockert P, Thoma R, Schiessl C, Kerkemeyer L, Amelung V, Jedamzik S, Reichmann J, Marschall U, Toelle TR. Digital Treatment of Back Pain versus Standard of Care: The Cluster-Randomized Controlled Trial, RiseuP. J Pain Res. 2020 Jul 17;13:1823-1838
- Priebe JA, Utpadel-Fischler D, Toelle TR. Less Pain, Better Sleep? The Effect of a Multidisciplinary Back Pain App on Sleep Quality in Individuals Suffering from Back Pain – a Secondary Analysis of App User Data. J Pain Res. 2020 May 20;13:1121-1128
- Schäfer AGM, Zalpour C, von Piekartz H, Hall TM, Paelke V. The Efficacy of Electronic HealthSupported Home Exercise Interventions for Patients With Osteoarthritis of the Knee: Systematic Review. J Med Internet Res. 2018 Apr 26;20(4):e152
- Toelle TR, Utpadel-Fischler DA, Haas KK, Priebe JA. App-based multidisciplinary back pain treatment versus combined physiotherapy plus online education: a randomized controlled trial. NPJ Digit Med. 2019 May 3;2:34
- Trost Z, Anam M, Seward J, Shum C, Rumble D, Sturgeon J, Mark V, Chen Y, Mitchell L, Cowan R, Perera R, Richardson E, Richards S, Gustin S. Immersive interactive virtual walking reduces neuropathic pain in spinal cord injury: findings from a preliminary investigation of feasibility and clinical efficacy. Pain. 2021a May 20
- Trost Z, France C, Anam M, Shum C. Virtual reality approaches to pain: toward a state of the science. Pain. 2021b Feb 1;162(2):325-331
- Turolla A, Rossettini G, Viceconti A, Palese A, Geri T. Musculoskeletal Physical Therapy During the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys Ther. 2020 Aug 12;100(8):12601264


