Despite a substantial growth in pain research globally and a well-established evidence base, people of all ages continue to experience poorly managed pain. Ensuring that research knowledge moves efficiently into practice is key to effective treatment of pain. Shockingly, it is estimated to take 17 years for new research to reach practice [6], with lags all the way from laboratory research to clinical research and then on to practice and policy. Purposeful and coordinated efforts are needed to reduce this time.
Knowledge translation (KT) is defined as the synthesis, exchange, and application of knowledge by relevant stakeholders to accelerate the benefits of global and local innovation in strengthening health systems and improving people’s health [10]. As defined by the Canadian Institutes of Health Research (CIHR, Canada’s federal health research funding organization), this is considered a “dynamic and iterative process that includes synthesis, dissemination, exchange and ethically-sound application of knowledge…”[1]. How knowledge is implemented is influenced by the type of evidence being shared, how it is shared, for what purpose, and the methods for knowledge translation that are used [8].
There are many different terms used for the concept of KT [8], as well as many different KT theories. Commonly used terms are in Figure 1.
In addition to multiple terms, numerous theories, models and frameworks about the process and adoption of knowledge exist. These help guide processes of translating knowledge into practice, understand or explain influencing barriers and enablers for implementation, and support evaluation efforts. Repositories of such information exists, facilitating access for people who use this knowledge, including people living with pain, family members/caregivers, healthcare professionals, and policymakers [2,5,7]. See the National Collaborating Centre for Methods and Tools website (https://www.nccmt.ca/) for examples of publicly available resources.
One of the most commonly used frameworks is the Knowledge-to-Action (KTA) framework [4,9] to guide implementing knowledge into practice [1]. This planned action framework is based on 30 theories, models and frameworks. Knowledge creation is visualized as a rotating knowledge creation funnel at the centerpiece, while the action cycle visualizes seven change processes to move knowledge into practice (Figure 2). These processes are seen as fluid, interactive, bi-directional and take local evidence, context and culture into account. The KTA can be seen as a roadmap for collective action by any group, from small local groups to large international teams.
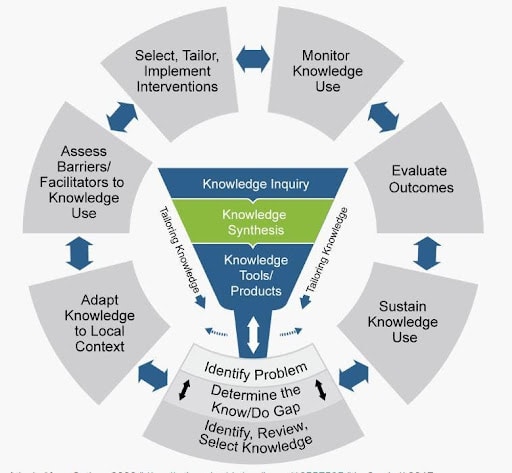
(Adapted from Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13-24. doi:10.1002/chp.47).
The 2022 IASP Global Year for Translating Pain Knowledge to Practice is the perfect opportunity to focus on moving the large body of evidence about effective pain treatment across the developmental and age trajectory into practice, and to highlight the urgency to improve uptake of knowledge to improve health outcomes.
Why does this matter?
Gaps between research knowledge production and practice exist. When knowledge is available but not used, it affects health outcomes, and results in unnecessary burden of pain. Seventeen-year delays have been cited for movement of pain knowledge into action [3]. As IASP members, we have an ethical responsibility to do better.
How to go about it
- Involve knowledge users from the beginning as partners in implementation (see Fact Sheet 2). Involving knowledge users including clinicians and people with lived experience of pain and their families at the beginning and throughout implementation can reduce barriers to using knowledge, increase the likelihood of the knowledge being perceived as of value and subsequently, used in practice and increase impact via effective KT strategies.
- Identify the research-based knowledge to be implemented (i.e. guideline, educational product) and how and where it is to be implemented.
- Identify the target knowledge users (i.e. clinicians, patients, parents of children, caregivers, etc.).
- Identify possible barriers or challenges to implementing the evidence/guideline related to each target knowledge user group (i.e. perceived lack of time or resources, perceived high complexity of the intervention, availability of the product, etc.). Address such barriers throughout the implementation process.
- Monitor (e.g., audits of practices), knowledge use (eg. adherence to a guideline, use of a knowledge tool).
- Facilitate engagement of all knowledge users throughout all implementation processes
- Evaluate implementation (i.e., is there reduced burden of pain, increased use of the knowledge translation tools).
- Co-develop, communicate and widely share resources in different and usable formats. It is important to develop ‘usable’ knowledge in synthesized, user-friendly formats that are appropriately targeted for the knowledge user groups. Examples may include short videos, podcasts, messages on social media platforms, clearly written evidence-based guidelines with algorithms to guide practice, and more.
REVIEWERS
Dawn Richards PhD
Ian Graham MA PhD
Katherine Boydell MHSc PhD
REFERENCES
[1] Canadian Institutes of Health Research. Guide to Knowledge Translation Planning at CIHR: Integrated and End-of-Grant Approaches. Ottawa, ON Canada: Canadian Institutes of Health Research, 2012 p.
[2] Centre for Implementation Science. Implementation Outcome Repository. n.d. Available: https://implementationoutcomerepository.org/.
[3] Chambers CT. From evidence to influence: dissemination and implementation of scientific knowledge for improved pain research and management. Pain 2018;159:S56–S64.
[4] Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N. Lost in knowledge translation: time for a map? J Contin Educ Health Prof 2006;26:13–24.
[5] Melbourne Academic Centre for Health (MACH). Implementation Science Resource Directory. 2021. Available: https://machaustralia.org/resource/implementation/.
[6] Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med 2011;104:510–520.
[7] National institutes of Health. National Center for Advancing Translational Sciences. Transl Sci Spectr 2021. Available: https://ncats.nih.gov/translation/spectrum.
[8] Rushmer R, Ward V, Nguyen T, Kuchenmüller T. Knowledge Translation: Key Concepts, Terms and Activities. In: Verschuuren M, van Oers H, editors. Population Health Monitoring. Springer, Cham, 2019.
[9] Skolarus TA, Lehmann T, Tabak RG, Harris J, Lecy J, Sales AE. Assessing citation networks for dissemination and implementation research frameworks. Implement Sci 2017;12.
[10] World Health Organization. EVIPNet Europe Strategic PlanNo Title. Copenhagen, 2015 p. Available: https://www.euro.who.int/__data/assets/pdf_file/0009/291636/EVIPNet-Europe-strategic-plan-2013-17-en.pdf.



