Poor pain care is an unfortunate reality for many patients, especially those belonging to racial minorities. Many factors have been proposed to explain pain-related racial disparities, but precious few studies have actually tested these hypotheses. My research group recently published a paper that aimed to better understand how provider racial bias and contextual ambiguity influenced providers’ pain care decisions for white and black patients.[1]
Why focus on bias among care providers? Although traditional (i.e., explicit) forms of racism have decreased over time, more subtle forms of racial bias are still with us. Implicit racial biases lie below conscious awareness – they are automatically activated without intent. Interestingly, many people simultaneously disavow racial biases and yet exhibit negative evaluations of black people on implicit measures. (Before you scoff at these bigoted Neanderthals, you might want to do a little self-exploration by taking the Race IAT. WARNING: the results might unsettle you.) Moreover, modern discriminatory behavior is better accounted for by people’s implicit, rather than their explicit, biases. This likely holds true in clinical settings, but we know very little about how implicit biases contribute to healthcare disparities.
What we do know is that certain factors amplify the impact of implicit biases. Ambiguity is one such factor. When asked to make decisions about ambiguous things – particularly when under time pressure – our implicit biases are much more likely to emerge and influence those decisions. You can see where I’m going with this…pain care is frequently characterized by both: pain is often ambiguous in nature, and providers often face intense pressure to see more patients in less time. Not only might providers’ biases and clinical ambiguity lead to disparities in treatment (e.g., analgesic prescription), they may also lead to disparities in the process of care (e.g., the amount of face-to-face time spent with patients).
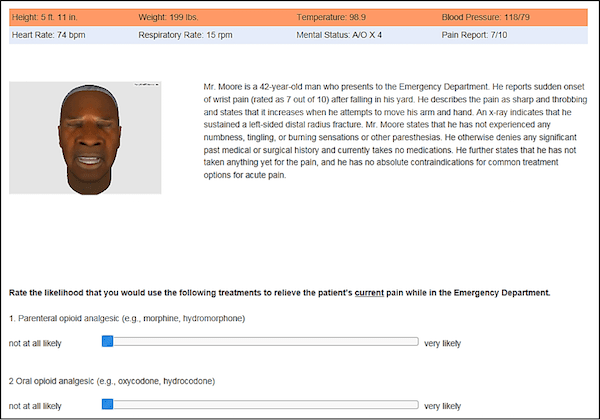
We used our virtual human methodology to examine both possibilities in a study of 129 U.S. physician residents (unfortunately, we did not have enough racial diversity in our sample to examine the interesting question of whether provider race matters). Participants viewed videos and written vignettes of 12 computer-simulated patients that varied by race (white, black) and clinical ambiguity (low, high). The patients presented with acute pain from a bone fracture that was confirmed upon x-ray (low ambiguity) or musculoskeletal back injury that lacked corresponding objective findings (high ambiguity). Also, high ambiguity patients had facial expressions that conflicted with their self-reported pain, whereas low ambiguity patients presented consistently. Participants made pain treatment decisions for each patient, and also completed the race attitude IAT to assess their implicit racial biases. See Figure 1 for an example still frame image of a patient vignette.
For the purposes of this post, I distill the results into a few key bullets:
- There was a significant Race x Ambiguity interaction: participants’ decisions to give opioids varied as a function of ambiguity for white but not black patients.
- In contrast to #1, the amount of time participants spent with each patient varied as a function of ambiguity for black but not white patients. Specifically, participants spent almost 20% more time with low ambiguity than with high ambiguity black patients.
- Participants showed a moderate-to-strong implicit preference for whites over blacks (consistent with U.S. population data), but these biases were not significant predictors of treatment decisions or time spent.
Let’s try to make some sense of these three findings:
- These results lend themselves to two opposing interpretations. One interpretation is that black patients received care that was less responsive to relevant clinical information about the presenting problem, objective findings, and facial expressions. This is consistent with findings that black patients receive less optimal pain care.[2] An alternative interpretation is that black patients received more consistent care, whereas white patients received variable care and may have even been “over-treated.” This is consistent with findings that lumbar surgery rates exceeded normative rates for white but not black workers’ compensation claimants.[3-4]
To test these opposing interpretations, a follow-up study could manipulate ambiguity in less clinically relevant ways. Aversive racism theory suggests that treatment for black patients would vary across irrelevant ambiguity manipulations – specifically, they would receive worse care in high-ambiguity situations despite the fact that these ambiguity manipulations do not provide useful clinical information.
- If time = “investment in care,” one might expect participants to spend more time with white patients, as found in some previous studies.[5,6] However, if time = “interrogation of patients,” one might expect participants to spend more time with black patients (especially in ambiguous situations), of whom they are more suspicious of things like drug diversion.[7,8] Generally speaking, our results are more consistent with “time as investment,” although we must be cautious in our conclusions at this point. This was one of the first studies to examine time in the context of pain care. Much remains to be known. One of our next steps is to actually manipulate time to test hypotheses about how time pressure interacts with provider and contextual factors to influence pain care.
- Our finding that implicit racial biases were not significant predictors of pain care, while counter to our hypotheses, is consistent with at least two other studies.[9,10] Perhaps the most parsimonious conclusion is that provider bias is not important. Another possibility concerns the level of specificity. The three studies conducted to date assessed general racial attitudes rather than specific stereotypes that might have a stronger bearing on care. Other, non-clinical studies suggest that the implicit belief that blacks are less capable of experiencing uniquely human emotions (just so we’re clear, this belief has no scientific or rational basis), such as anguish and remorse (emotions that are familiar to many a pain patient), may have a more pronounced impact on pain care. We are testing this hypothesis in a current study.
Stay tuned…
About Adam Hirsh
 Adam is a clinical health psychologist and Assistant Professor in the Department of Psychology at Indiana University – Purdue University Indianapolis. His lab conducts research on pain judgments and decision-making, perceptions of injustice in children/families dealing with chronic pain, and individual differences in pain expectations and coping. In addition to pain science, his lab spends a lot of time contemplating the wonders of dogs (canine, not hot), craft beer, and pastries
Adam is a clinical health psychologist and Assistant Professor in the Department of Psychology at Indiana University – Purdue University Indianapolis. His lab conducts research on pain judgments and decision-making, perceptions of injustice in children/families dealing with chronic pain, and individual differences in pain expectations and coping. In addition to pain science, his lab spends a lot of time contemplating the wonders of dogs (canine, not hot), craft beer, and pastries
References
[1] Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K. (2015). The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain, 16, 558-568.
[2] Meghani SH, Byun E, Gallagher RM. (2012). Time to take stock: A meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med, 13, 150-174.
[3] Chibnall JT, Tait RC, Andresen EM, Hadler NM. (2005). Race and socioeconomic differences in post-settlement outcomes for African American and Caucasian workers’ compensation claimants with low back injuries. Pain, 114, 462-472.
[4] Chibnall JT, Tait RC, Andresen EM, Hadler NM. (2006). Clinical and social predictors of application for social security disability insurance by workers’ compensation claimants with low back pain. J Occup Environ Med, 48, 733-740.
[5] Chen LM, Farwell WR, Jha AK. (2009). Primary care visit duration and quality: does good care take longer? Arch Intern Med, 169, 1866-1872.
[6] Olfson M, Cherry DK, Lewis-Fernández, R. (2009). Racial Differences in Visit Duration of Outpatient Psychiatric Visits. Arch Gen Psychiatry, 66, 214-221.
[7] Becker WC, Starrels JL, Heo M, Li X,Weiner MG, Turner BJ. (2011). Racial differences in primary care opioid risk reduction strategies. Ann Fam Med, 9, 219-225.
[8] Hausmann LR, Gao S, Lee ES, Kwoh CK. (2013). Racial disparities in the monitoring of patients on chronic opioid therapy. Pain, 154, 46-52.
[9] Haider AH, Sexton J, Sriram N, Cooper LA, Efron DT, et al. (2011). Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA, 306, 942-951.
[10] Sabin JA, Rivara FP, Greenwald AG. (2008). Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care, 46, 678-685.



