Introduction
Our recent review, published in “Pain Medicine”, highlighted the measurement properties of quantitative sensory testing (QST) and its clinical utility. QST results have been shown to be related to pain or neural sensitivity. QST has been put forward as a potentially useful tool for monitoring disease prognosis and evaluating interventions, but continued research that uses consistent QST parameters is required to define this role.
Central hypersensitivity has been implicated as a contributor to abnormal pain responses in musculoskeletal pain and has even been implicated in the transition from acute to chronic pain. Early detection of central hypersensitivity might allow clinicians to make more accurate prognostic predictions and to allocate patients to the appropriate management strategies, perhaps targeting these central changes.
Quantitative sensory testing provides one way of measuring such central processes with a psychophysical approach that tests the function of the whole sensory axis using standardised stimuli. QST results can then be compared to norms and be linked to the clinical picture, as shown in Figure 1.
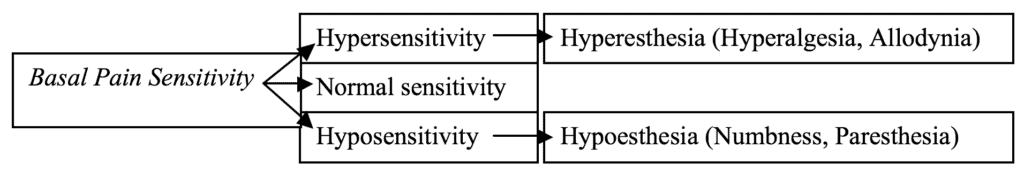
Threshold is a core measure in QST. The threshold at which a stimulus is detected is commonly used to assess nerve function in diseases of the peripheral nervous system. The threshold at which a stimulus is reported as painful is an indicator of basal sensitivity. This ‘basal pain sensitivity’ may be useful for predicting abnormal pain (Figure 1).
Two distinct threshold measuring paradigms/methods (e.g. method of limits and levels) have been developed based on the empirical and theoretical concepts of sensory threshold. Empirically, a sensory threshold is the stimulus level (minimum energy) required to achieve perception. Theoretically, a sensory threshold is a property of signal detection.
The method of limits approach is an empirically developed method in which the intensity of an applied stimulus is increased or decreased until the subject perceives or feels it as painful and stops the stimulus by a button/controller. The threshold values are determined by calculating mean values during a series of stimuli. However, this method clearly involves reaction time, which means that the results are highly dependent on the subject’s motor ability and attention.
The method of levels is based on signal detection theory. In the method of levels, a series of predetermined stimuli is applied, and the subject has to report whether the stimulus is perceived or not or whether it is painful or not for each stimulus. The intensity of the next stimulus in the series of stimuli is systematically increased or decreased based on the subject’s response. This method does not rely on reaction time and may therefore provide more stable responses, but it is a relatively time-consuming procedure.
Rationale for using QST in clinic
The main benefit of using QST in the clinic is probably that it facilitates a mechanism-based approach to diagnosis and management. This appears to hold great potential. QST can be used to distinguish between phenomena such as hyperalgesia (increased pain response), allodynia (lowered pain threshold), wind up (increased pain response in dorsal horn), referred pain (pain felt in a part of the body other than its actual source), and tenderness (local tissue sensitivity). QST results may also be used to define the territory of pain (sensory mapping) and even to identify different sensory phenotypes. Patients could also be categorised into sub-groups according to these sensory phenotypes, with each phenotypic group having a different prognosis. In this way, QST responses could also be useful for predicting treatment outcomes and for tracking responses to treatment, because QST responses should change if treatment influences the mechanisms that are purported to underlie the pain.
Limitations and future directions
There is emerging evidence that suggests a role for QST in pain management. However, the evidence to direct the specific modalities, techniques, diagnostic or therapeutic prediction rules are lacking in many respects. There is a need to continue testing to develop reliable and clinically feasible QST protocols that take less time and that use inexpensive, portable equipment. Future research should also focus on longitudinal prospective studies with a large cohort of patients so as to examine the prognostic and evaluative properties of different sensory modalities and to compare different sensory modalities, assessment protocols, indicators, and decision rules. The implementation of QST in clinical research and practice will also need to be facilitated via a knowledge translation strategy.
About Zakir Uddin
 Zakir is a physiotherapist who obtained his undergraduate degree from the University of Dhaka (Bangladesh), a master degree from Kobe University (Japan) and a doctoral degree from McMaster University (Canada). The article discussed here was initially developed in 2014 as a background chapter of his PhD thesis at McMaster University, under the supervision of Professor Joy MacDermid.
Zakir is a physiotherapist who obtained his undergraduate degree from the University of Dhaka (Bangladesh), a master degree from Kobe University (Japan) and a doctoral degree from McMaster University (Canada). The article discussed here was initially developed in 2014 as a background chapter of his PhD thesis at McMaster University, under the supervision of Professor Joy MacDermid.
Zakir has academic work experience in 5 different countries (e.g. Bangladesh, Japan, Canada, South Korea and UAE). He is currently working as an Assistant Professor at Department of Physiotherapy, College of Health Sciences, University of Sharjah, United Arab Emirates.
Zakir is interested in the hedonic pain-pleasure continuum, psychophysics and quantifying pain/sensation. His research interests are (I) Detection of abnormal pain responses and trying to correlate Executive Function and Conditioned Pain Modulation, (II) Identifying personal and physiological risk factors for development of chronic musculoskeletal pain, (III) Justifying outcome measurement and optimising better intervention in rehabilitation. His clinical interests focus on minimising pain and disability in patients with chronic musculoskeletal disorders.
References
Uddin Z, MacDermid JC. Quantitative Sensory Testing in Chronic Musculoskeletal Pain. Pain Med. 2016;17(9):1694-1703. http://dx.doi.org/10.1093/pm/pnv105
Commissioning Editor: Carolyn Berryman; Associate Editor: Tory Madden



