In general there is a lack of long-term success in treating people with persistent musculoskeletal pain and long-term anterior knee pain or patellofemoral pain syndrome (PFPS), is no exception [1]. It is reported that approximately 25% of patients with PFPS continue to have pain and dysfunction one year or more after physiotherapy, the most frequently used conservative treatment for PFPS [2].
We evaluated the long-term effect of high-dose, high-repetition medical exercise therapy (MET) in patients with PFPS with respect to pain and functional outcomes in a multicenter randomized controlled clinical trial (RCT) with one year follow-up [3].
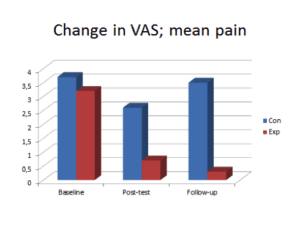
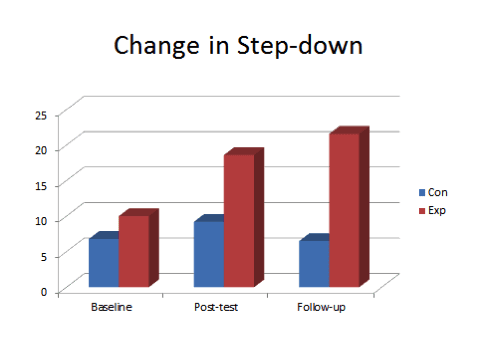
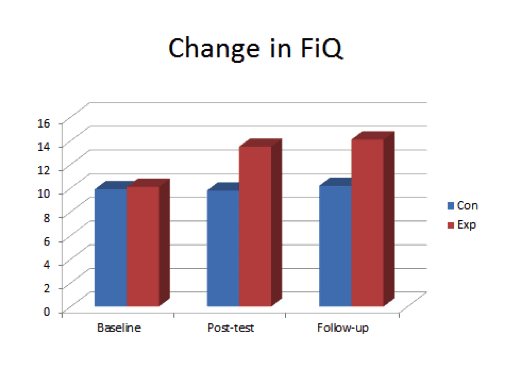
The original RCT evaluated two different therapeutic exercise regimens in patients with PFPS and revealed important (clinically and statistically significant) differences between treatment groups after a 12-week intervention period, indicating that high-dose, high-repetition MET is more efficacious than low-dose, low-repetition exercise therapy in this patient group. The differences between groups at post-test were −1.6 for mean pain (VAS: 0–10 cm) representing an effect size of 0.80, 6.5 for step-down test (numbers of completed step-downs in 30 seconds) representing an effect size of 0.81, and 3.1 for the modified Functional Index Questionnaire (FIQ: 0 points indicates maximal disability, 16points no disability) representing an effect size of 0.89. (Figure 1-3).
The term “high-dose, high-repetition” refers to the higher number of exercises, higher number of repetitions and sets and the inclusion of a substantial amount of aerobic/global exercise using a stationary bike in the experimental group. The exercises in the control group program was termed “low-dose, low-repetition” referring to the lower number of exercises, lower number of repetitions and sets, and the brief sequences of aerobic/global exercises. Dosage parameters in the control group were graded in accordance with traditional strength training principles, commonly prescribed for PFPS-patients [4]. For patients in both groups, load and range of motion were graded in order to make the program appropriate and achievable with as little discomfort as possible. The participants in both groups performed group specific and individually tailored exercises three times a week for 12 weeks, always supervised by the same physiotherapist. The number of exercises, repetitions, sets, and duration of aerobic/global exercises were kept constant in both groups throughout the study.
At one year follow-up the group differences are maintained and even increased with respect to pain and functional outcomes [5]. The results indicate a continuous improvement in the experimental group and a worsening in the control group between post-test and follow-up. In this period there was no intervention applied in the groups. The differences between groups at follow-up were −1.8 for mean pain representing an effect size of 0.9, 4.5 for step-down test representing an effect size of 0.6, and 1.1 for FIQ representing an effect size of 0.3. (Figure 1-3).
The long-term effects seen at one year follow-up draw increased attention towards central and psychological factors. This includes cognitive-behavioural factors, such as health beliefs, self-efficacy and fear-avoidance [6, 7] as well as stress mechanisms (including hypothalamic–pituitary–adrenal [HPA] axis activity), neural sensitization [8, 9] and motor learning [10, 11]. These are long-term mechanisms, some of which evidence suggests proved to be main predictors for treatment outcome on the longer term [6, 12] and to immediate individual reliable change in patients with persistent musculoskeletal pain [13]. There was however no instruments applied in the RCT or follow-up study addressing these possible mechanisms.
The apparent new state of healthy self-regulation occurring in the patients completing high-dose, high-repetition MET is valuable and cost-efficient on the individual level, but probably also to society. Measured as reduction in work absence costs, this is demonstrated in patients with long-term subacromial pain, finding high-dose, high-repetition MET to be more efficient than low-dose, low-repetition exercise [14]. Additonally, a presumed healthier state of self-regulation might make people more independent of treatment and health care services, as well as less dependent on social financial support. Although speculative, it is possible that several of the mechanisms behind the long -term clinical effects seen in this current patient group, could be relevant in other persistent musculoskeletal pain conditions. Long-term effects of high-dose, high-repetition MET have been demonstrated in patients with persistent subacromial pain [15]. However, the high-dose, high-repetition MET-approach might be most appropriate in certain rehabilitation phases in people with persistent musculoskeletal pain.
Future research is needed to explore the mechanisms behind the clinical effects as well as test the usefulness of these interventions more extensively.
About Berit Østerås
 Berit is a physiotherapist, Msc. and Associated Professor at Sør-Trøndelag University College, Faculty of Health Education and Social Work, Department of Physiotherapy, Trondheim, Norway.
Berit is a physiotherapist, Msc. and Associated Professor at Sør-Trøndelag University College, Faculty of Health Education and Social Work, Department of Physiotherapy, Trondheim, Norway.
Since 2004 she has combined her clinical physiotherapy practice with teaching and scientific work. In her clinical work she sees an increasing number of patients presenting with persistent musculoskeletal pain. Her scientific work and studies have addressed different patient populations in the long-term pain category.
References
[1] Davis IS, & Powers CM (2010). Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat, April 30-May 2, 2009, Fells Point, Baltimore, MD. J Orthop Sports Phys Ther, 40 (3) PMID: 20195028
[2] Piva SR, Fitzgerald GK, Irrgang JJ, Fritz JM, Wisniewski S, McGinty GT, Childs JD, Domenech MA, Jones S, & Delitto A (2009). Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil, 90 (2), 285-95 PMID: 19236982
[3] Østerås B, Østerås H, Torstensen TA, & Vasseljen O (2013). Dose-response effects of medical exercise therapy in patients with patellofemoral pain syndrome: a randomised controlled clinical trial. Physiotherapy, 99 (2), 126-31 PMID: 23219636
[4] Chiu JK, Wong YM, Yung PS, & Ng GY (2012). The effects of quadriceps strengthening on pain, function, and patellofemoral joint contact area in persons with patellofemoral pain. Am J Phys Med Rehabil, 91 (2), 98-106 PMID: 22248804
[5] Østerås B, Østerås H, & Torsensen TA (2013). Long-term effects of medical exercise therapy in patients with patellofemoral pain syndrome: results from a single-blinded randomized controlled trial with 12 months follow-up. Physiotherapy, 99 (4), 311-6 PMID: 23764516
[6] Piva SR, Fitzgerald GK, Wisniewski S, & Delitto A (2009). Predictors of pain and function outcome after rehabilitation in patients with patellofemoral pain syndrome. J Rehabil Med, 41 (8), 604-12 PMID: 19565153
[7]. Woby SR, Urmston M, & Watson PJ (2007). Self-efficacy mediates the relation between pain-related fear and outcome in chronic low back pain patients. Eur J Pain, 11 (7), 711-8 PMID: 17218132
[8]. McFarlaneAC. Stress-related musculoskeletal pain. Best Pract Res Clin Rheumatol 2007;21(3):549–65.
[9]. Riva R, Mork PJ, Westgaard RH, & Lundberg U (2012). Comparison of the cortisol awakening response in women with shoulder and neck pain and women with fibromyalgia. Psychoneuroendocrinology, 37 (2), 299-306 PMID: 21764519
[10]. Fu M, Yu X, Lu J, & Zuo Y (2012). Repetitive motor learning induces coordinated formation of clustered dendritic spines in vivo. Nature, 483 (7387), 92-5 PMID: 22343892
[11]. Kida T, Kaneda T, & Nishihira Y (2012). Dual-task repetition alters event-related brain potentials and task performance. Clinical Neurophysiol, 123 (6), 1123-30 PMID: 22030141
[12]. Meeus M, Nijs J, Van Mol E, Truijen S, & De Meirleir K (2012). Role of psychological aspects in both chronic pain and in daily functioning in chronic fatigue syndrome: a prospective longitudinal study. Clin Rheumatol, 31 (6), 921-9 PMID: 22349876
[13]. Asenlöf P, & Söderlund A (2010). A further investigation of the importance of pain cognition and behaviour in pain rehabilitation: longitudinal data suggest disability and fear of movement are most important. Clin Rehabil, 24 (5), 422-30 PMID: 20442254
[14]. Østerås H, Arild Torstensen T, Arntzen G, & S Østerås B (2008). A comparison of work absence periods and the associated costs for two different modes of exercise therapies for patients with longstanding subacromial pain. J Med Econ, 11 (3), 371-81 PMID: 19450093
[15]. Østerås H, Torstensen TA, & Østerås B (2010). High-dosage medical exercise therapy in patients with long-term subacromial shoulder pain: a randomized controlled trial. Physiother Res, 15 (4), 232-42 PMID: 21110409



