Ever put down a copy of Explain Pain, or some other highly valuable text, and asked ‘So how do I integrate all this stuff when I assess a patient and plan treatment?’ You might have felt exasperated after reading yet another article on pain mechanisms, or central sensitisation, or cortical reorganisation, and said to yourself ‘yes but how do I know what is driving what?’ If my conversations at conferences and courses is anything to go by, then a whole lot of you will be nodding.
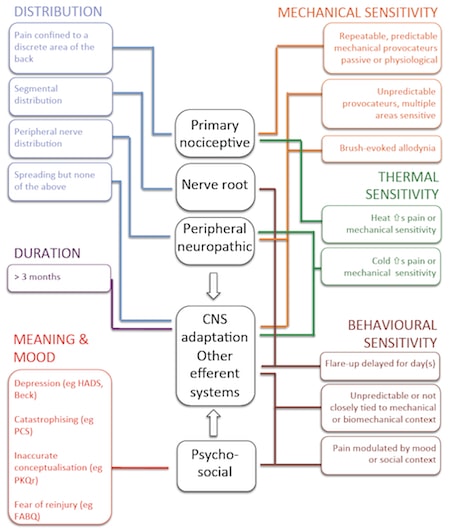
This post is really just to introduce a general guide that we use to interpret how a patient describes their pain. One might go through the different sections (in different colours on this slide) and place a tick next to the relevant mechanism. I hope it is fairly self explanatory – feel free to download General guide to contributing mechanisms and modify it as you see fit. If you do take it into the clinic and use it in a more formal way, then we would love to know about it. Good luck folks!
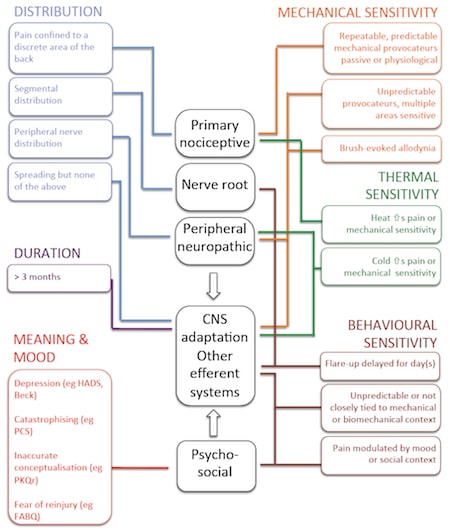
Download high resolution General guide to contributing mechanisms here
About Lorimer Moseley
 Lorimer is NHMRC Senior Research Fellow with twenty years clinical experience working with people in pain. After spending some time as a Nuffield Medical Research Fellow at Oxford University he returned to Australia in 2009 to take up an NHMRC Senior Research Fellowship at Neuroscience Research Australia (NeuRA). In 2011, he was appointed Professor of Clinical Neurosciences & the Inaugural Chair in Physiotherapy at the University of South Australia, Adelaide. He runs the Body in Mind research groups. He is the only Clinical Scientist to have knocked over a water tank tower in Outback Australia.
Lorimer is NHMRC Senior Research Fellow with twenty years clinical experience working with people in pain. After spending some time as a Nuffield Medical Research Fellow at Oxford University he returned to Australia in 2009 to take up an NHMRC Senior Research Fellowship at Neuroscience Research Australia (NeuRA). In 2011, he was appointed Professor of Clinical Neurosciences & the Inaugural Chair in Physiotherapy at the University of South Australia, Adelaide. He runs the Body in Mind research groups. He is the only Clinical Scientist to have knocked over a water tank tower in Outback Australia.
Link to Lorimer’s published research here. Downloadable PDFs here.