If you’ve recently attended a pain conference, had a glass of wine with a pain boffin or spent time googling ‘pain’ you’ve no doubt come across the terms ‘neuroplasticity’ and ‘central sensitization’. These buzzwords are increasingly used to describe biological changes that might contribute to persistent low back pain. But do they really explain why some people get better after hurting their back while others do not?
An increasing body of work suggests the brain is involved when pain becomes persistent. Researchers have shown substantial anatomical and functional reorganisation of the human brain (‘neuroplasticity’) and increased sensitivity of neurons in the brain and spinal cord (‘central sensitisation’) [see a few examples here (1-3)]. Importantly, because these changes have the ability to maintain pain after the initial injury has resolved they are widely believed to explain, at least in part, why pain becomes persistent(4). But – if this is the case then why can’t we predict who will develop persistent back pain and who will not?
Two major limitations hamper our ability to predict outcome in low back pain. First, although it is clear that brain organisation is altered in persistent low back pain, and these changes appear to relate to symptoms, the literature mostly consists of studies that use a cross-sectional design. In other words, there are lots of studies that examine people with persistent back pain at a specific point in time. There has been very limited e.g.(5) investigation of brain changes in the transition from acute to persistent low back pain – which is precisely when some people are getting better while others are not. Second, a range of other mechanisms (such as genetics, psychosocial factors, hormones) are all likely to interact with brain changes to predict who will develop persistent low back pain and who will not. But the interaction between these different pieces of the low back pain puzzle has not been examined during the transition from acute to persistent pain.
To answer these important questions, we recently received a National Health and Medical Research Council (NHMRC) Project Grant to follow more than 260 people with acute low back pain as they either i) get better or ii) develop persistent pain. Over a period of 12 months we will examine changes in the brain, spinal cord, genetics, hormones and psychosocial factors of each individual to determine whether these factors, and their possible interaction, can predict who gets better after hurting their back and who does not. We hope that the results of our study will have an impact on the way we understand, treat and perhaps even prevent the transition to persistent low back pain in the future.
Passionate about pain and the brain? Want to contribute to our understanding of why some people get persistent back pain while others do not? Join our team!
We are looking for two highly motivated individuals to undertake full-time PhD scholarships (fully funded for 3 years) and one exceptional post-doctoral researcher (fully funded for 4 years). You will join active research groups at University of Western Australia and Neuroscience Research Australia, benefiting from engagement with top researchers in the fields of brain plasticity and pain. You will gain skills and knowledge in transcranial magnetic stimulation to measure neuroplasticity in the human brain, neuronavigation, phlebotomy, central sensitisation and the transition from acute to chronic low back pain. For more information or to apply, please send a CV to s.schabrun@uws.edu.au.
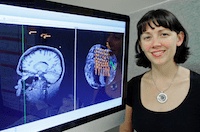
About Siobhan Schabrun
 Siobhan is a NHMRC Clinical Research Fellow and 2014 Fulbright Scholar at University of Western Sydney. After blending a degree in physiotherapy with a PhD in neuroscience, she is passionate about understanding, treating and preventing persistent pain. Her research has a particular focus on that buzzword… ‘neuroplasticity’. Siobhan was the winner of the inaugural Australasian Brain Stimulation Conference joke contest – which says something about her sense of humour… You can find her published research here.
Siobhan is a NHMRC Clinical Research Fellow and 2014 Fulbright Scholar at University of Western Sydney. After blending a degree in physiotherapy with a PhD in neuroscience, she is passionate about understanding, treating and preventing persistent pain. Her research has a particular focus on that buzzword… ‘neuroplasticity’. Siobhan was the winner of the inaugural Australasian Brain Stimulation Conference joke contest – which says something about her sense of humour… You can find her published research here.
References
1. Flor H, Braun C, Elbert T, & Birbaumer N (1997). Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neuroscience letters, 224 (1), 5-8 PMID: 9132689
2. Tsao H, Danneels LA, & Hodges PW (2011). ISSLS prize winner: Smudging the motor brain in young adults with recurrent low back pain. Spine, 36 (21), 1721-7 PMID: 21508892
3. Tsao H, Galea MP, & Hodges PW (2008). Reorganization of the motor cortex is associated with postural control deficits in recurrent low back pain. Brain, 131 (Pt 8), 2161-71 PMID: 18669505
4. Apkarian AV. The brain in chronic pain: clinical implications. Pain Manag. 2011;1:577-86.
5. Baliki MN, Petre B, Torbey S, Herrmann KM, Huang L, Schnitzer TJ, Fields HL, & Apkarian AV (2012). Corticostriatal functional connectivity predicts transition to chronic back pain. Nature neuroscience, 15 (8), 1117-9 PMID: 22751038