Was my treatment helpful, benign or harmful?
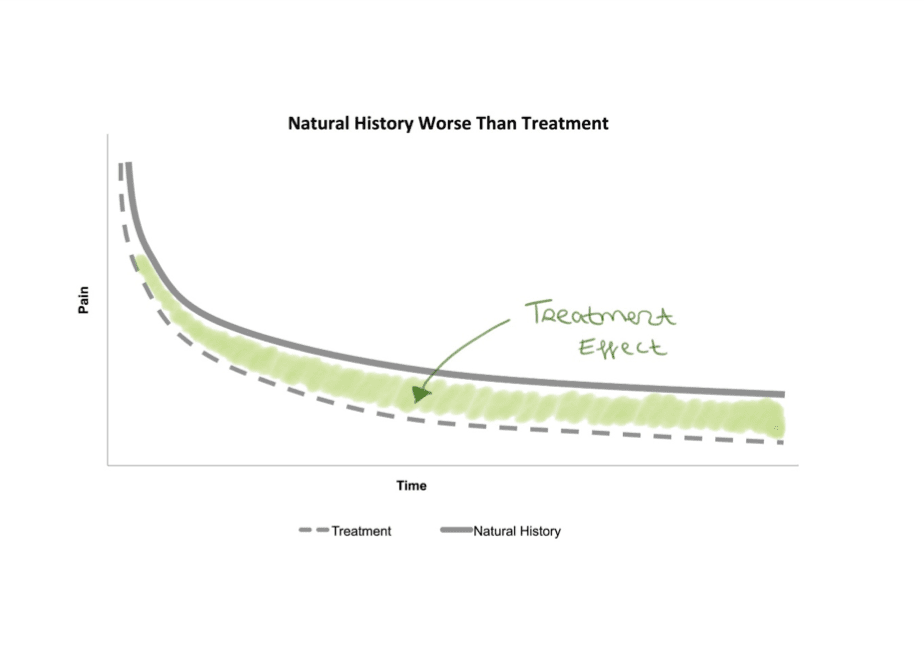
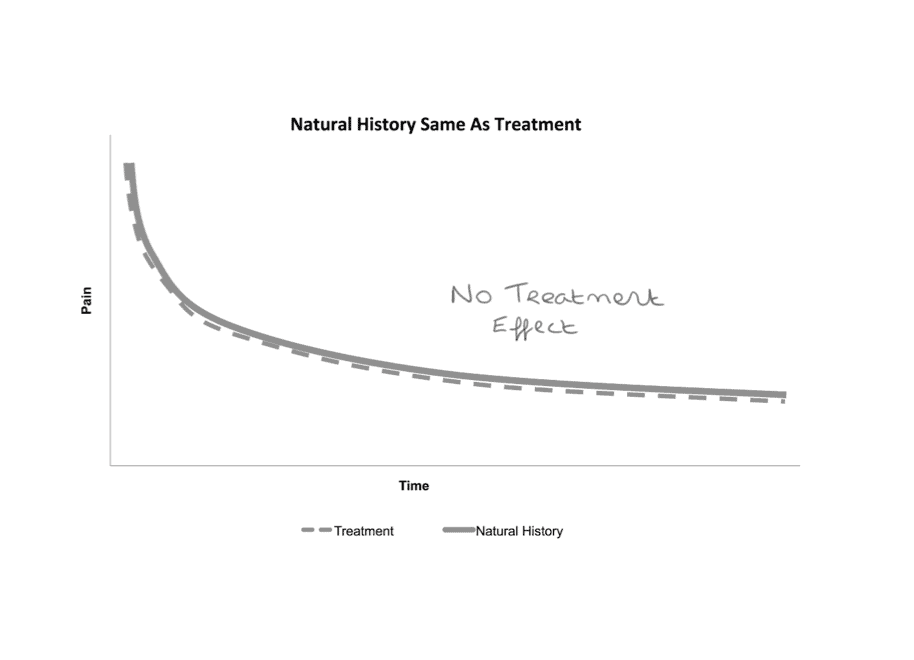
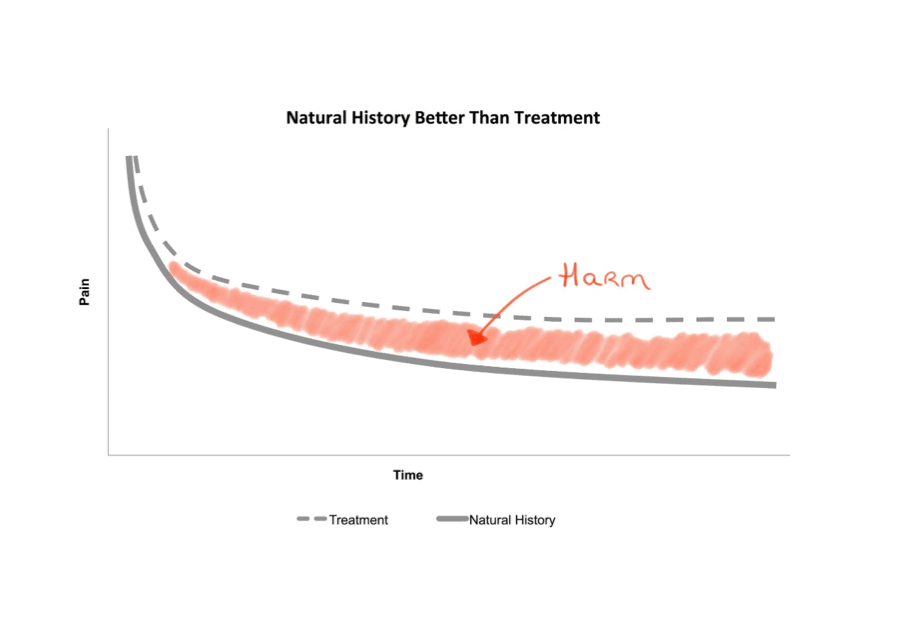
Consider the common clinical scenario – a patient presents complaining of pain. You decide to administer a particular treatment. Over time the patient’s symptoms improve. Do you then succumb to bias and presume your intervention facilitated their recovery? Do you consider the possibility that recovery was entirely co-incidental and independent of your efforts? Or that their trajectory may have been more favorable without your intervention? Each of these potential scenarios are outlined below.
The literature will have the answer
In an era of evidence based medicine we have a responsibility to the public to make informed treatment choices and engage in shared decision making. In order to do so, we turn to the literature for treatment interventions with plausible mechanisms that have demonstrated efficacy in well-designed randomised controlled trials (RCTs)…This should be easy right?
Ideally, the active intervention you wish to implement has been compared to appropriate controls e.g. a credible placebo and a wait-and-see arm (1). Such a study would tell us if the active treatment is better than natural history and if any treatment effect is mediated by mechanisms other than placebo. This type of study is illustrated below.
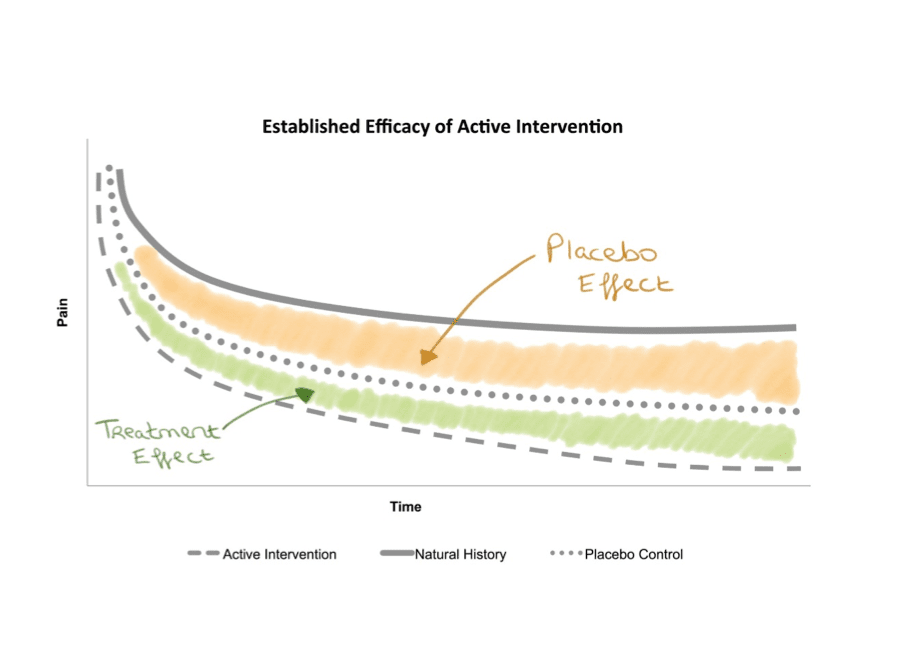
If the study is of high quality, then this result should meaningfully inform treatment selection. However, these types of trials are rare and exceedingly difficult to perform. In particular, for non-pharmacological treatments it is often difficult to introduce a credible sham and accounting solely for natural history is difficult in any circumstances. Who wants to be part of the wait and see arm, right?
So instead, two “active treatments” are often pitted head to head. However, it is important to understand when interpreting the results of such trials that this design does not estimate efficacy, rather, it simply determines whether one approach is superior to another. Outperforming an active control does not necessarily indicate efficacy as it is possible for an unhelpful intervention to appear effective if the control intervention is harmful. An obvious example of this is when corticosteroid injections (known for their long-term deleterious effect) are used as a comparator in tendinopathy trials (2, 3).
Considering the expected trajectory / usual clinical course of low back pain
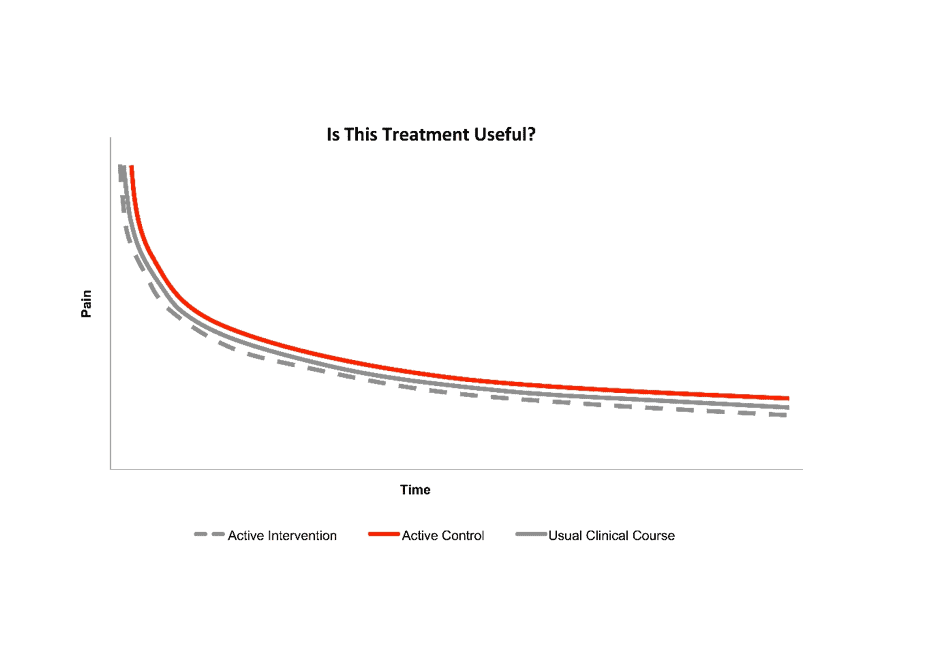
Understanding and considering the expected trajectory / usual clinical course may give some context in which to evaluate the true value of a treatment. The example below highlights this issue in low back pain (LBP) trials.
A recent RCT utilised a head to head design to compare “individualised physiotherapy” (active intervention) against “advice” (active control) in a group of patients with mixed-duration LBP (4). Importantly, the authors concluded that both treatments were effective with the pathoanatomically informed individualised physiotherapy offering additional benefit beyond pathoanatomically informed advice (4). However, as described above it is entirely plausible that this treatment effect is a function of the control arm faring poorly when natural history is unaccounted for.
In order to further explore the performance of the control arm and to give context to these findings we plotted the trajectories of both arms of the example RCT alongside the usual clinical trajectory of a large cohort of LBP patients with overlapping pain durations obtained from a recent meta-analysis of inception cohort studies (5, 6).
Of course, it is impossible to perform direct statistical comparisons between the datasets. Nonetheless it was very interesting to observe that neither arm of the RCT seemed to convincingly outperform the usual clinical course derived from a large cohort of people with LBP. This raises questions about the clinical utility of the treatment approach involved.
For the full story, please read our article (6).
How should this be interpreted by the end user?
The outcomes and recommendations drawn from clinical trials that utilise an active intervention as a control need to be interpreted with caution. In particular, the performance of the comparator requires scrutiny and should be considered in the context of what could reasonably be expected of that cohort (either via natural history or usual clinical course). The purpose of this exercise is to encourage clinicians to account for the comparator used in head to head RCTs before considering a treatment approach as any treatment for back pain can appear to be effective… it might just depend on what you compare it with.
About Mervyn Travers
 Merv is a physiotherapist who trained at University College Dublin, Ireland. He moved to Australia in 2008 to pursue further studies and he completed his PhD at Curtin University, Perth, Australia in 2014.
Merv is a physiotherapist who trained at University College Dublin, Ireland. He moved to Australia in 2008 to pursue further studies and he completed his PhD at Curtin University, Perth, Australia in 2014.
He now works as a researcher at The School of Physiotherapy at The University of Notre Dame Australia in Fremantle. He also works as a lecturer at the School of Physiotherapy and Exercise Science, Curtin University.
His research interests are in pain where he is currently working on projects in the realms of low back pain, period pain and Achilles tendinopathy.
References
[1] Chan A, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ (Clinical research ed). 2013;346.
[2] Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet (London, England). 2010;376(9754):1751-67.
[3] Gosens T, Peerbooms J, van Laar W, den Oudsten B. Ongoing Positive Effect of Platelet-Rich Plasma Versus Corticosteroid Injection in Lateral Epicondylitis. The American journal of sports medicine. 2011;39(6):1200-8.
[4] Ford JJ, Hahne AJ, Surkitt LD, Chan AYP, Richards MC, Slater SL, et al. Individualised physiotherapy as an adjunct to guideline-based advice for low back disorders in primary care: a randomised controlled trial. British journal of sports medicine. 2016;50(4):237.
[5] Menezes Costa LC, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LOP. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ : Canadian Medical Association Journal. 2012;184(11):E613-E24.
[6] Travers MJ, Bagg MK, Gibson W, O’Sullivan K, Palsson TS. Better than what? Comparisons in low back pain clinical trials. British journal of sports medicine. 2018.



