The importance of accounting for change over time when investigating how our treatments work
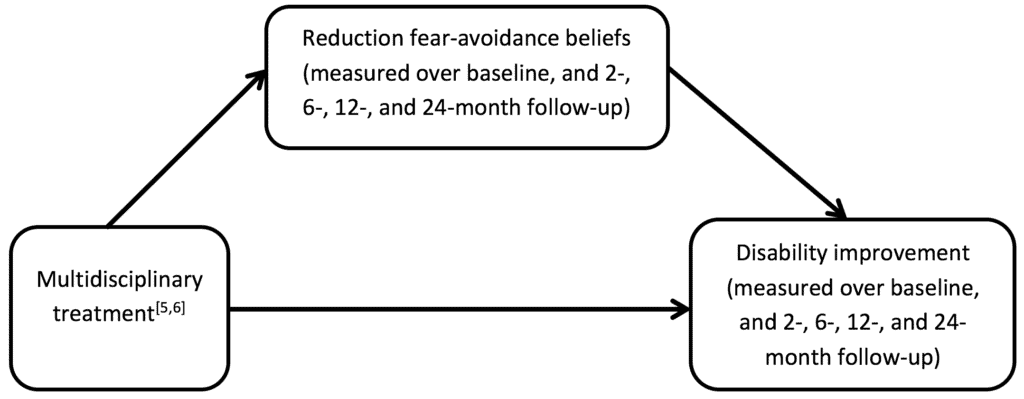
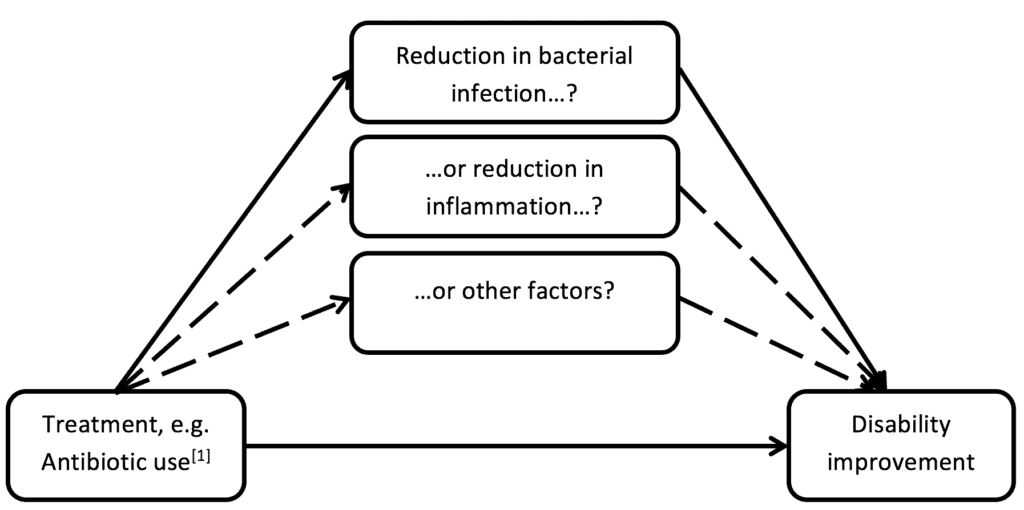
Whenever we test a treatment or intervention in the form of a randomised clinical trial (RCT), we should be interested in how and why it was successful (or unsuccessful) at improving patient outcomes and which specific elements or components of the treatment, if any, led to an improvement in outcome (i.e. what are the mediating factors). For example in the proposed and controversial use of antibiotics for LBP with modic changes[1], it is important to determine whether the improvements in patient outcomes are actually due to reduction in bacterial infection rather than some other mechanism, such as reduction in inflammation (see example hypothesised mediating pathway below). Unfortunately, underlying assumptions are often not formally tested, so we cannot determine empirically which factors should be focused on as mediating factors. Mediation analysis, a statistical technique used to identify the pathways through which a treatment achieves its effects, has been attracting interest within the musculoskeletal pain field and is now being planned within several RCT protocols (e.g.[2,3]).
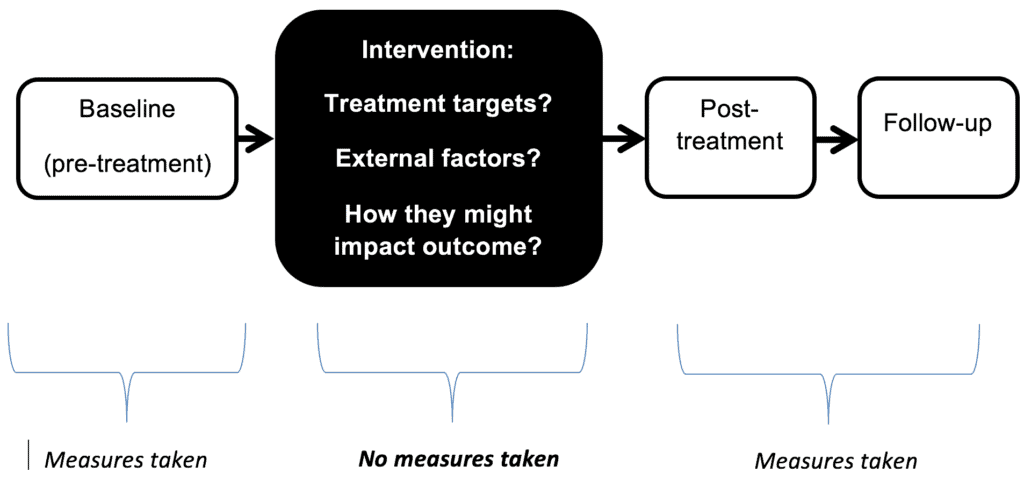
In order to identify these pathways, measures are needed at key time points. This is important for two reasons: firstly, knowing when a potential mediating factor changes is helpful in telling us whether the factor may have been actually affected by the intervention; and secondly, it helps to establish the hypothesised causal links between the factor in question and outcome. Although baseline and follow-up measures are often included, very few trials measure factors during treatment[4]. This is important, because change that would have occurred as a result of treatment (in both the outcome of interest and any potential mediator) might have already happened by post-treatment, making it impossible to establish what comes first, and conclusively establish the link between the potential mediator and the outcome. If the measurement points fall outside the treatment period, we end up with a “black box” where we know very little about how the components of a treatment actually lead to patient improvement (see image below).
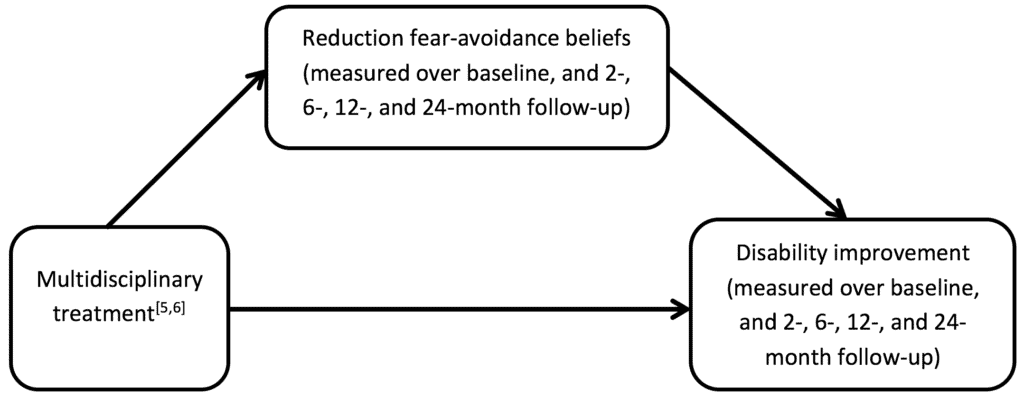
To try to illustrate this point, let us look at an example of a study we recently conducted,[5] which was one of the first to investigate change over more than two time points in a musculoskeletal pain clinical trial. The original trial[6] compared improvement in function between a multidisciplinary intervention (involving psychologists and physiotherapists delivering different components) and treatment as usual. The intervention had three main components; addressing fear-avoidance beliefs, setting activity/exercise goals, and setting a timeframe for the patient to resume their normal activities. As the study included measures of one of the assumed mediators (fear-avoidance beliefs) and outcome (functional disability) at five time points (baseline, then at two-, six-, 12-, and 24-months follow-up), it provided an opportunity to test a type of statistical mediation analysis (latent growth modelling [LGM]) which can incorporate multiple time points (e.g.[7,8]). While this study did not include any assessments taken during the treatment period, which would have been ideal to see whether changes in fear avoidance beliefs came before changes in functional improvement, the analysis did allow us to test the feasibility and value of conducting this more complex form of mediation analysis. The results of the study found an effect of change in fear-avoidance beliefs as a mediating factor through which the multidisciplinary intervention was showing benefits over the usual treatment care in terms of change in physical function, and demonstrated that conducting mediation analysis in this way is feasible and valuable.
To conclude, optimal methods for mediation analysis are continuing to be developed and hold the promise of increasing our understanding of how treatments are actually working, providing information on mediating factors for both patients and their treating clinicians which may help the design, development and implementation of increasingly efficacious treatments.
About Gemma Mansell

Gemma works as a post-doc Research Associate at the Research Institute for Primary Care Sciences, Keele University, UK. Her main research interests are around behavioural interventions and specifically investigating how they work through conducting mediation analysis, which was the focus of her PhD. She plans to continue with this work to help improve the design of trials to better allow for the evaluation of mediating effects. Most of her spare time and money is spent on music, going to gigs and consuming more coffee than is probably healthy.
References
[1] Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): A double blind randomized clinical controlled trial of efficacy. European Spine Journal 2013; 22:697-707.
[2] Lee H, Moseley GL, Hübscher M, Kamper SJ, Traeger AC, Skinner IW, McAuley, J.H. Understanding how pain education causes changes in pain and disability: Protocol for a causal mediation analysis of the PREVENT trial. Journal of Physiotherapy 2015; 61(3):156.
[3] Lonsdale C, Hall AM, Williams GC, McDonough SM, Ntourmanic N, Murray A, Hurley, D.A. Communication style and exercise compliance in physiotherapy (CONNECT). A cluster randomized controlled trial to test a theory-based intervention to increase chronic low back pain patients’ adherence to physiotherapists’ recommendations: Study rationale, design, and methods. BMC Musculoskeletal Disorders 2012; 13:104.
[4] Mansell G, Samper SJ, Kent P. Why and how back pain interventions work: What can we do to find out? Best Practice and Research Clinical Rheumatology 2013;27(5):685-697.
[5] Mansell G, Hill JC, Main C, Von Korff M, van der Windt, D. Mediators of treatment effect in the Back In Action trial: Using latent growth modelling to take change over time into account. Clinical Journal of Pain 2016; EPub ahead of print.
[6] Von Korff M, Balderson BHK, Saunders K, Miglioretti DL, Lin EHB, Berry S, Moore JE, Turner JA. A trial of an activating intervention for chronic back pain in primary care and physical therapy settings. Physical Therapy 2005;113(3):323-330.
[7] Cheong J, MacKinnon DP, Khoo ST. Investigation of mediational processes using parallel process latent growth curve modelling. Structural Equation Modeling 2003; 10(2):238.
[8] Witkiewitz K, Donovan DM, Hartzler B. Drink refusal training as part of a combined behavioral intervention: Effectiveness and mechanisms of change. Journal of Consulting and Clinical Psychology 2012; 80(3):440-449.
Senior Commissioning Editor Neil O’Connell; Associate Editor: JP Caneiro