For some time, patients, clinicians and researchers have tried to understand the causes of back pain. Theories are abundant, and some have been empirically tested. But to date, the only thing clear is that we’re still unsure about what causes back pain. This uncertainty about the causes and mechanisms of back pain stifles the development of effective targeted treatments – which arguably sustains the monumental burden of this condition, worldwide.
But it’s not all doom and gloom. Surveys tell us that most back pain experts believe greater efforts should be directed at understanding the mechanisms of back pain. The response to this call is shown in the graph below. I did a crude search on Google Scholar using a keyword that represents a common statistical method to study mechanisms (‘mediation analysis’) and combined it with ‘back pain’. I then plotted the results over the past decade. Note that the dots represent how many hits there were during that year, not the cumulative sum.
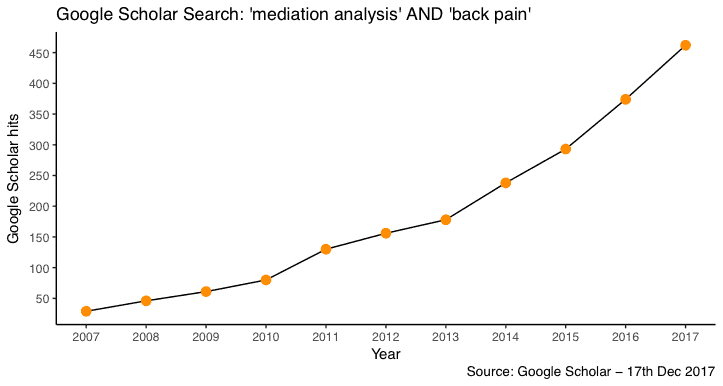
As you can see, productivity is increasing. Whether this increase in the rate of publications truly reflects better understanding and practice… I don’t know! But I think this figure provides some indication that there is increasing interest in this topic. It’s also important to acknowledge that mediation analysis is not the only way of studying mechanisms. Basic science studies can provide biological underpinnings of disease, and some qualitative studies can provide important detail about mechanistic processes. But among these, mediation analysis is probably the method that has seen the greatest methodological and statistical advances over the past decade.
So then, what does the evidence tell us?
In our review, we tried to gather information that would be relevant to both clinicians and researchers. We did so by reviewing mediating factors that may influence the course of back pain, and mediators of common treatments for back pain. We then took a methodological viewpoint and evaluated the quality of mediation studies in the field.
We found a general theme across observational studies and randomised trials – most mediation studies focused on psychological mechanisms. For example, self-efficacy, beliefs, and catastrophizing. It seems that psychological mechanisms explained about 20-33% of the effect of pain on disability. This suggests that certain psychological factors are worthwhile treatment targets to reduce disability for patients in care. This was also reflected among most mediation analyses of randomised trials looking at treatment mechanisms. Perhaps it’s no big news that psychological constructs explain a part of the mechanism. But an important message is that up to 80% of the mechanism could be explained by non-psychological factors. This suggests that it might be time to look broader and consider physical, biological, and social domains that could shed light on unexplained mechanisms. Doing so could generate a new body of evidence that might inform the development of novel treatment strategies for back pain.
As for treatment mechanisms, it could also be useful to look beyond mechanisms that carry positive treatment effects, and also examine mechanisms that might suppress treatment effects (see here for schematic). For example, if spinal imaging is part of a treatment package, it may inadvertently increase the patient’s belief that pain is a sign of tissue damage (mediator), which could lead to increased disability (outcome). Suppressive mechanisms could also be triggered by unintended consequences of an otherwise effective intervention. For example, a group based exercise therapy (exposure) may exert its effects through changes in physical capacity (positive mediator), but incompatible social interactions between participants could increase distress (negative mediator) which may suppress the positive gains of the intervention and reduce the overall treatment effect. These are plausible mechanisms that should feature in clinical reasoning, and of course, tested in randomised trials.
The nitty gritty – and things to be mindful of…
The methodological and technical components of studying mechanisms can be quite complex. There’s too much to cover in this blog, but if there is one take home message, it is that we should think carefully about confounding bias. When we pick up a mechanisms paper, we should ask: have possible confounders been controlled for? And further, would the presence of unmeasured and unknown confounders invalidate the findings of the study? We found that the answer to these two critical questions was a ‘no’ for most of the studies we reviewed – only 53% adjusted for confounders, and none provided sensitivity tests for unmeasured and unknown confounders. Unfortunately, things get worse… we found that the majority (59%) used cross-sectional designs, which opens up the possibility for reverse-causation; and the reporting of these studies was generally haphazard (watch this space). Sadly, in light of all these shortcomings, it is difficult to make any kind of causal inference from the existing studies. Clearly there is lots of room for improvement.
Moving forward…
Recent methodological advances have precisely outlined the assumptions needed for making valid causal inferences from mediation analyses. These new methods have also contributed various sensitivity analysis techniques to see how much the confidence in our ability to make causal inference would change when critical assumptions are violated. If researchers made efforts to measure and control for confounders; and if patients and clinicians were to be mindful about the limitations of mediation studies, our understanding of the mechanisms of back pain would improve substantially.
About Hopin Lee
 Hopin is a NHMRC post-doctoral research fellow based at the Centre for Statistics in Medicine, and Rehabilitation Research in Oxford – Nuffield Department of Orthopaedics Rheumatology and Musculoskeletal Sciences, University of Oxford. A key focus of his work involves investigating the mechanisms of medical interventions and public health strategies. He is also trying to reduce the heterogeneity of reporting of mechanistic evaluations in clinical trials by producing a reporting guideline. His work can be found here, and he occasionally tweets.
Hopin is a NHMRC post-doctoral research fellow based at the Centre for Statistics in Medicine, and Rehabilitation Research in Oxford – Nuffield Department of Orthopaedics Rheumatology and Musculoskeletal Sciences, University of Oxford. A key focus of his work involves investigating the mechanisms of medical interventions and public health strategies. He is also trying to reduce the heterogeneity of reporting of mechanistic evaluations in clinical trials by producing a reporting guideline. His work can be found here, and he occasionally tweets.
Reference



