Eight early-career researchers are taking part in the first cycle of the PRF Virtual Correspondents Program. This science communications training program provides participants with knowledge and skills needed to communicate science effectively to a wide range of pain researchers and to patients and the broader public. Throughout the course of the program, the Correspondents will conduct interviews and podcasts with leading pain researchers, provide news and virtual meeting coverage – and blog posts! Take a look at their posts below, which will be published weekly over the course of the next six weeks.
Meet the PRF Correspondents

Week 6: Monday, August 17, 2020
Preparing for Generation COVID: The Long-Term Effects of COVID-19 Infection
Reflecting on the Importance of Feedback and Communication in Pediatric Pain
Pain and Pleasure Share a Lot in Common
Over the last approximately 20 years one population of sensory afferents have been at the forefront of the conversation about pleasant touch. These C-tactile (CT) afferents are low-threshold mechanoreceptors or “touch” neurons that innervate the skin and are optimally tuned to stroking at rates that are deemed pleasurable and at temperatures near those of human skin. Their firing rates also positively correlate with psychological rating of touch “pleasantness.” CT afferents are therefore implicated in affective touch in humans. But what about affective touch that doesn’t involve stroking?
Deep pressure is another type of pleasant touch, perhaps more important for social affiliation as it includes hugs, huddling, massage, swaddling of infants, and the rough handling of offspring we often see in rodents in the lab (stepping and sitting on offspring). Oscillating deep pressure can also be pleasant when removed from a social setting, which may not come as a surprise to anyone that’s ever sat in a massage chair. However, we know far less about how deep pressure is perceived as pleasant than we do about gentle stroking.
A recent study aimed to expand the study of pleasant touch to deep pressure. They designed an oscillating compression sleeve to determine which body part and which pressure level were the most “pleasant,” and then compared the pleasantness of this optimal massage-like compression to their well-established gentle stroking paradigm known to activate CT afferents.
The deep pressure had similar ratings of pleasantness and feelings of calm to that of CT afferent gentle stroking. The activation patterns of the two stimuli, found using fMRI, were also similar in the primary somatosensory cortex, an area that processes the type and intensity of sensory input.
Interestingly, there were differences in activation in the secondary somatosensory cortex (S2), an area involved in higher order functions related to our skin, limbs, and joints, like the formation of tactile memories, and the insula, an area thought to play a role in emotion. Tactile stroking activated bilateral S2 and posterior insula while deep pressure activated contralateral S2 and mid-insula. It is not yet clear what the significance of these differences is, but it might suggest that deep pressure activates a novel pleasant touch pathway.
However, as their oscillating compression sleeve also touches the skin, it would also (at least weakly) activate CT afferents, as they are mechanosensory and fire with pressure on the skin.
The authors suggest that the pleasant deep pressure is not conveyed by CT afferents, as previous research demonstrated that sensations of deep pressure remain with anesthetization of the skin. However, that study did not rate “pleasantness” and the present study did not anesthetize the skin. Perhaps it is a combination of skin surface and deeper tissue stimulation that produces pleasantness.
Melanie Schaffler, PhD student, University of Pennsylvania, US
The von Frey assay is the most frustrating behavioral task I’ve learned since joining the pain field. For readers unfamiliar with this classic pain assay (hi, Mom!), this test involves placing the test subject (a mouse or rat) on a wire mesh rack and confining them to one area (my lab uses little tubes, about 2.5 inches in diameter, for this). After allowing time for the animals to calm down and habituate to their new location, they are individually tested by touching the underside of a hindpaw with plastic filaments – think fishing line – of different diameters. At their threshold, the animals respond by reflexively flicking their paw away from the filament.
While the premise of the von Frey test is simple, its execution is challenging and its interpretation is often wanting. It takes practice to perform the test in a consistent, replicable manner in terms of approach, force, and duration of the filament application, and von Frey test performance can vary greatly between individual experimenters. Deciding what counts as a withdrawal versus regular movement while conducting the test is especially frustrating for novices, and it’s difficult to avoid bias in this subjective test. The presence of a large human experimenter likely influences behavior, too. It’s also likely that testing multiple mice at once – which I certainly do! – could influence results in this assay. In her talk last week as part of the Leading Edge Symposium, postdoctoral fellow Dr. Monique Smith described how exposure to a mouse experiencing acute inflammation can decrease mechanical thresholds in bystander mice in her “social transfer of pain” model. With this in mind, I can imagine that being tested in the same room as other mice could also introduce variability in the von Frey assay.
In addition to its logistical drawbacks, the von Frey assay is not a particularly rich behavioral measure. It only allows for the measurement of reflexive responses, and relies upon a binary, yes or no, classification. Furthermore, changes in mechanical threshold measured with von Frey may not necessarily indicate increased pain, and it is challenging to distinguish if the filament application is innocuous or noxious – important distinctions when considering the translational relevance of our findings. Furthermore, this punctate approach to measuring hypersensitivity and/or allodynia may not effectively model the symptoms that bring human patients into the clinic. Indeed, I am by no means the first person to bemoan the limitations of the von Frey assay – many reviews of the preclinical approaches to studying pain point out these limitations, with some going as far as Dr. Geoffrey Bove, whose 2006 Topical Review referred to the von Frey assay as “the pain field’s ‘Tin Standard.’”
The re-thinking of “classic” behavioral assays is not unique to the pain field. For example, many preclinical researchers studying depression and anxiety are re-thinking their assays (a particularly lively forced swim discussion surrounding a recent ACNP meeting making waves on Twitter comes to mind). The National Institute of Mental Health (NIMH) put out a set of guidelines for behavior in 2019, calling on preclinical neuroscience researchers to consider the research question they are asking; determine if that question is important; and finally identify an experimental system that will allow for that important question to be answered. I think this is a good framework for developing better measures of mechanical thresholds, and ultimately, to measure pain. I think a good assay should assess an aspect of the human condition being studied, in a manner that is meaningful to the model species. The assay should be easily replicated by different labs and individual researchers, the measurement of the behavior should not be so disruptive that the measurement becomes meaningless, and its analysis should be objective. Indeed, Bove’s 2006 article describes a similar wish list for “the ideal mechanical stimulator.” In particular, I think the most important features called for are the experimenter to be “blinded to the force” applied, and for the device itself to make “the decision of whether a trial was acceptable or not.”
While it’s easy to disparage the von Frey assay – people have been discussing its limitations for some time – it has been challenging to develop a better assay. However, new technology such as high-speed videography and machine learning-driven analysis is already yielding promising improvements. A new statistical platform from the lab of Dr. Ishmail Abdus-Saboor at UPenn (and lab of fellow PRF blogger Melanie Shaffler) called PAWS (Pain Assessment at Withdrawal Speeds) allows for the automatic quantification and combination of several behavioral features into a single pain score (see here). Approaches where the experimenter no longer has to make a subjective, real-time analysis of behavior should ultimately yield more replicable results. The next important step for this type of technology is to create a closed-loop system in which stimuli of greater or lower mechanical force can be applied to the subject depending on previous responses – all without the experimenter in the room. It’s exciting to imagine what new findings will be made, and what overlooked past findings will be rediscovered, with less variable behavioral methods for testing and analysis.
Nora McCall, PhD, postdoctoral fellow, University of Pennsylvania, US
Preparing for Generation COVID: The Long-Term Effects of COVID-19 Infection
Of the people who recover from their infectious period with COVID-19, a subgroup report persistent symptoms lasting for months without sign of recovery. The stories of two women in their 30s, reported by the Australian Broadcasting Corporation last month, tell of neurological symptoms like migraine, brain fog, and fatigue lasting at least four months after diagnosis – on top of continuing respiratory issues. Persistent chest, muscle, and joint pain have also been reported by people no longer infectious with COVID-19. Support groups have been set up for people who have spent hundreds of days with symptoms that just won’t subside. With the current focus on a vaccine, treatment, or cure for COVID-19 (and rightly so) to combat the continuation of the tragic loss of life that the pandemic has so far wrought, the effect of these long-term symptoms on otherwise ‘recovered’ individuals is an understandable current blind spot in how its impact has been reported.
The question that interests me most here is this: which of these long-term effects can be attributed to tissue damage during the acute stage of infection, and which might instead point to a more chronic inflammatory response that persists after the period of infection has passed?
Some research is beginning to be published looking at pain and other symptoms that persist after the infectious period ends. One of PRF’s Papers of the Week last week – a study on headache during and after COVID-19 infection in French patients – found that 3.6% of patients reported headache one month after fever remission. The authors suggest that elevated circulating pro-inflammatory cytokines in a subpopulation of patients may be responsible for persistent headache.
Nerve pain has also been noted as a rare symptom of COVID-19 in the acute phase. An early study looking at neurological symptoms in COVID-19 patients from Wuhan found nerve pain in around 4% of hospitalized patients with severe infection. A case report published a few days ago describes a woman with intense bilateral burning pain during her infectious period for which gabapentin was an effective treatment.
It’s too soon to know whether we can expect pain to be a long-term effect of COVID-19 in some people. Current reports seem to suggest it might be. If that turns out to be the case, current knowledge about the role of inflammation in pain states may assist in understanding how it comes about in COVID-19. Conversely, understanding how COVID-19 might shape the immune system to initiate pain states might help to better understand other persistent pain conditions.
We may have more urgent public health, economic, and research priorities as the pandemic rages on in many parts of the world. At some point, though, we may need to reckon with a generation of people wearing the biopsychosocial effects of the illness for years to come. We should identify what those effects might be and prepare to provide relief where we can.
Jayden O’Brien, PhD student, University of Sydney, Australia
I swear this dress is blue, but my husband thinks it’s green. It’s the dress I was wearing when we first met, but this is no rose-colored memory lapse. Even to this day, if I pull out that dress, all I see is blue, but he assures me it’s still green.
How can this be?
I presume it’s because his and my brain delineate the color spectrum slightly differently. Kind of like how Russians see an additional distinct color in their rainbow; both of our brains have evidently learned to draw a threshold between green and blue, forming two separate color concepts, but have done so at slightly different hues.
It’s fascinating to think that these distinctions between colors don’t really exist outside of shared human observation. Similarly, most sensory experiences exist on a continuum (e.g., soft to loud, low to high), so really all linguistic classifications of sensation are arbitrary and based on personal experience and cultural norms.
What about pain though?
Personally, I’ve done a lot of work with pain thresholds, and I’m always surprised by the high variability between individuals. We like to think that these pain thresholds are as clear as sensory thresholds, but, “can you feel it or not?” is a much less loaded question (in my opinion) than, “is it painful or not?”
I also wonder how much of the inter-individual variability we see in pain thresholds is the result of learned differences in linguistic classification. For example, in the days after you returned to do your normal (though now exceptionally challenging)weightlifting routine post COVID-19 lockdown, what did you feel? Aches, soreness, fatigue, unpleasantness, discomfort, niggles, tension, stiffness or pain? We all likely agree that pain is the ‘worst’ of these descriptors, but I highly doubt we all agree on whether this instance constitutes it’s use.
Now, why is this interesting?
Well, we know there’s a lot of language related to sensory input and, as with color, specific use of language can improve an individual’s ability to discriminate between sensory stimuli. There’s also a large vocabulary for emotional experiences, and here specific language also seems to be helpful in distinguishing nuanced emotional experiences, which can then improve emotional regulation. So, maybe by introducing people to more nuanced linguistic classifications of uncomfortable but sub-painful sensations, we can actually change an individual’s perception of pain and improve their ability to self-manage it. And if we can change this for painful sensation, then maybe one day we can get my husband to realize that my dress is actually blue.
Megan McPhee Christensen, PhD Student, Aalborg University, Denmark
How would you feel if you went to the doctor complaining of severe cramping following eating and they told you to try taking one breath mint every morning to help? More importantly, would you hypothesize it would work?
A drug trial from 2010 tested that hypothesis. It was an open-label trial, which means both physicians and patients knew which treatment patients were receiving, and patients were told they were taking placebo.
Placebo is defined as a harmless substance given with no physiologic effect. The “placebo effect” is the finding that inert substances not known to have any treatment value still improved some patient symptoms in trials. In a typical randomized controlled trial, patients would be randomly assigned to a placebo or treatment group, and neither they nor their physician would know which treatment they received. Much of the placebo effect has been attributed to patients believing they are receiving treatment that is sufficient to heal them.
However, in the 2010 trial, patients were told they were taking placebo. Not only that, the placebo effect was explained in detail. Despite this, the placebo still provided adequate relief in 65% of patients, and 30% more patients experience relief when compared to no treatment. Perhaps even more telling is that roughly 35% of patients who received no treatment whatsoever still had relief. These findings prompted a second study, which closed this year, more deeply investigating placebo in this population.
So who are these patients who are now candidates for treatment with inert pills? It was a group of patients diagnosed with irritable bowel syndrome (IBS), most of whom had failed other existing treatments.
What does this all have to do with pain? One of the primary complaints with IBS is cramping following food. Indeed, cramping specifically was something that decreased with the open-label placebo treatment. Cramping is a type of pain often associated with involuntary muscle contraction, but in the abdomen can also be related to gas in the intestine or other causes. Critically for this blog post’s readers, however, it is a type of pain that was successfully treated using open-label placebo.
Many have found the discovery of the placebo effect, and even this study, to be somewhat disheartening. This is because one implication could be that our science-forward treatments may be doing less than we think they are.
But when I read these findings, I get very excited about the future of medicine. Not only could the use of placebo as treatment drastically decrease cost, but open-label placebos are honest and ethical. While surreptitiously giving someone a sugar pill and telling them it’s a treatment would be entirely unethical, explaining that you are giving someone a placebo is entirely ethical. And, since a placebo, by definition, is inert, it is a treatment that carries no risk.
Beyond that, think about the implications this carries for pain and other functional pain disorders similar to IBS. I have said in previous posts that we cannot treat pain if we don’t fundamentally understand what pain is. Instead of degrading the practice of medicine, I believe these placebo findings enhance it. Placebo treatment is clearly unlocking a pathway for people to heal themselves. Specifically, it is helping patients decrease and manage their symptoms, in this case a form of pain, without adding a new chemical to their bodies.
This reconfirms what this blog’s readers may already know: pain is deeply rooted in higher-level, central processing. It also implies a potential new treatment for pains that have no known cause. I write to you today in defense of placebo, and I hope when I become a doctor that I will be able to add this to my arsenal for pain care.
Sage Morison, MD/PhD student, Northwestern University, US
Reflecting on the Importance of Feedback and Communication in Pediatric Pain
Receiving a diagnosis of chronic pain can be an overwhelming experience, especially in childhood. In the case of a diagnosis of pediatric chronic pain, there are important factors to consider in terms of how this information should be communicated with the family. While it is important to clearly communicate the diagnosis with the family and outline a treatment plan, there are nuances in terms of how best to share this information and a responsibility to ensure that each family member, including the child, has understood the information.
Communicating this information can be complex, but as Dr. Neil Schechter and colleagues discuss in a Viewpoint in JAMA Pediatrics, the feedback session following an assessment for pediatric chronic pain can be a vital time to ensure that families feel comfortable and prepared to manage the child’s health. The authors highlight important factors for a successful feedback session, including describing the biopsychosocial nature of pain in the feedback session, clarifying treatment and prognostic information, and engaging families in planning. Key guidelines are also identified to help with a more productive conversation, such as understanding the family’s expectations, explaining the value of the multidisciplinary team, maintaining ongoing connection with the family, and sharing optimism about treatment outcomes where appropriate.
The child-specific considerations, as identified by Schechter and colleagues, are relevant across clinical areas when it comes to communicating about pain with children. The importance of acknowledging and validating the child’s symptoms is identified as a critical opportunity to signal to the child that their pain is being taken seriously and is not imagined. Emphasis should also be placed on the importance of education and using communicative tools, such as metaphors, to help young patients understand the information provided.
This article is an excellent illustration of how to engage in family-centered care and highlights tangible strategies to draw families into the feedback session. What I perhaps appreciated most of all was the emphasis placed not only on communication with caregivers, but with the child as well. It is important to ensure we are validating the child’s experience of pain, particularly if they have not been taken seriously in the past, but I also appreciated the emphasis on providing education and discussing the care plan in a developmentally appropriate manner. The suggested use of imagery, for example, is not only an excellent way to keep children connected to the discussion, but it may also help put things into terms that parents can comprehend. Not only does this keep all family members on the same page, but it can also give parents additional tools to discuss the information with their child if necessary.
Meaningfully engaging with children and their families in the feedback session can ultimately empower them to take control of the child’s health. By capitalizing on opportunities to validate, educate, and support families, we can take meaningful steps toward making a positive impact in the child’s health journey.
Nicole MacKenzie, PhD student, Dalhousie University, Halifax, Canada
Pain and Pleasure Share a Lot in Common
Author’s note: This blog post is based on a Perspective in Nature Reviews Neuroscience by Irene Tracey and Siri Leknes. A common neurobiology for pain and pleasure. Nat Rev Neurosci. 2008 Apr;9(4):314-20.
The idea behind the concept that pain and pleasure go together is a fascinating one: there is evidence supporting a common neurobiology for pain and pleasure, two seemingly antagonistic phenomena.
First, a wide body of research suggests there is a strong overlap in the brain areas involved in pain and pleasure processing. This research includes, for example, functional imaging studies in humans, which allow us to estimate which brain areas are active at any one time, or in response to a specific stimulus, using different indirect measures of neuronal activity. Additionally, there have also been electrophysiology studies in rodents where one can more or less directly measure neuronal activity in individual neurons or groups of neurons. These and other studies have revealed that some brain areas, like the amygdala, are implicated in both pain and pleasure.
Second, there are also similarities in how these two phenomena are processed at the molecular level. This is particularly striking when we look at the dopamine and opioid systems. Dopamine is a neurotransmitter, that is, one of the chemicals that neurons use to transmit signals to and communicate with each other. Opioids comprise a range of molecules that can be produced either endogenously (by the body itself) or synthetically. Both dopamine and opioids have been shown to play a role in pain (or pain relief) and pleasure.
Finally, pain and pleasure can sometimes actually interact with each other. For example, there have been reports of pain being decreased by pleasant odors or images.
To conclude, pain and pleasure have a tremendous impact on animal behavior, since both pleasure-seeking and pain-avoidance behaviors increase our chances of survival. In fact, as 18th- and 19th-century philosopher Jeremy Bentham put it, “Nature has placed mankind under the governance of two sovereign masters, pain and pleasure.” It is therefore incredibly interesting, although perhaps not entirely surprising, that they should go together.
Elisa Clemente, PhD student, University College London, UK
As is custom during COVID-19, I was recently on a Zoom call to catch up with friends in different parts of the United States. These were friends with diverse clinical backgrounds who I had gone to school with and worked alongside in various capacities. After discussing current events and how our lives have changed over the last few months, inevitably, the topic of work crept into the conversation and specifically, the issue of providing patients with “labels” and the benefits and/or drawbacks of categorizing a patient. I stated that, for research purposes, a diagnostic label assists with components of my work, such as inclusion/exclusion criteria when developing a clinical trial. Yet, others countered and described the pitfalls of pigeonholing patients and the difficulty of communicating labels and diagnoses since some of them carry a negative connotation. Some patients become overly focused on the label given to them and my colleagues felt that other approaches to patient communication regarding pathology create less stigma than using a single label in an attempt to encapsulate an individual.
A recent IASP 2020 Global Year for the Prevention of Pain webinar covered the topic of pain prevention after a musculoskeletal injury. Dr. Geoff Bostick of the University of Alberta, Canada, was one of four presenters and spoke specifically on patient prognostic labels. He stated that prognostic labels can be useful to gauge recovery trajectories following an injury. Interestingly, he then expressed the sentiments of my friends that while helpful, labels can also create stigma. When clinicians hear that a patient is a “catastrophizer” or “fear avoidant”, this may impact patient care, particularly for those who are often marginalized. He further explained the challenges during patient communication when utilizing labels, specifically when the label and the patient’s expectations for recovery are mismatched with those of the clinician.
During my time in the clinic, I encountered individuals with persistent pain who felt frustrated with being bounced around from clinic to clinic. They simply wanted answers as to why they hurt. I can vividly recall an instance of such a patient who was finally provided with a label, or in her case a diagnosis, for her persistent pain and the sense of relief she felt when someone could finally provide an answer.
So, how do we balance our patients’ desire for answers without the oversimplification of a label? There may not be a simple response to that question, but when looking back, I know my friends on the Zoom call were truly advocating for treating the person as a whole, rather than just treating whatever label or diagnosis a patient has received in the past. I’m not quite sure when my next Zoom meeting will be with my friends (hopefully soon), but when I “see” them next I’ll try to get to the bottom of this clinical question.
Andrew Post, PhD student, University of Iowa, US
Week 5: Monday, August 10, 2020
Patient Engagement in Research: More Than Just Food for Thought
"Yet Another Bias in Science?"
Exercise: The Dr. Jekyll and Mr. Hyde for Those with Achilles Tendon Pain?
There’s No Blood Test for Persistent Pain – But Could There Be
Abandoning Home for Abroad: Why Do We Do It?
Depression, Dopamine, and Pain
Chronic pain may actually have adaptive value in mammals?!? When framing my work in the past, I often present pain as a double-edged sword: acute pain is a useful learning mechanism that increases survival due to its rapid association with dangerous experiences; conversely, the sustained negative sensation of chronic pain does not provide an adaptive teaching signal. A new Correspondence in Current Biology from Lister et al. suggests that the adaptive value of chronic pain should not be so easily dismissed.
Each day of this study, food-deprived mice –and thus likely motivated to obtain food –had ten opportunities (i.e., trials) to obtain a food reward (one-quarter of a single Kellogg’s Froot Loop) in an octagonal maze. Here, they faced a choice: to take a long route or short route to the food reward. Clearly, the short route is preferable, as it accelerates access to the food reward. Accordingly, after six to eight days of training in the maze, most mice chose the short route the majority of the time.
However, when the odor of a mouse predator (i.e., fox urine) was blown across the short route, the mice had a new, more complicated choice to make: “Do I continue to get my food more efficiently despite the possibility of predation, or do I play it safe and take the long way around?”
Overall, the mice shifted their strategy in the presence of this danger-signaling scent, choosing the short route fewer times than before. However, mice that underwent a procedure to induce chronic neuropathic pain chose the longer but safer route more often than their sham counterparts. Did being in chronic pain allow these mice to become “hypervigilant” to the potential danger signaled by the predator odor, increasing their adaptive fitness? This hypothesis is consistent with the findings of a clever study in squid, which found that injury without anesthesia decreased the predation of the squid by bass, compared with squid that were anesthetized during injury; thus, nociceptive sensitization appeared to confer adaptive value.
I was surprised by the sham control mice choosing the short-but-dangerous-smelling route around seventy percent of the time; this seems like a bad life choice. It is possible the control mice were unable to alter their approach learned during training sessions. Another possibility is that these mice initially avoided the short route during the test trials. Then, over multiple trials of experience, they learned that the predator odor did not actually correspond to a present threat, allowing them to safely revert to their “fast-to-the-Froot-Loop” strategy. If this is the case, it would suggest that while chronic pain might have increased hypervigilance, it made it more challenging for those mice in chronic pain to change their strategy as the trials with fox urine progressed. Indeed, work from the lab of Ted Price in 2018 found that mice that underwent the same chronic pain-inducing procedure had difficulty shifting their strategy to obtain a food reward. Looking at route choices trial-by-trial could be useful in figuring out if shifts in strategy, as well as vigilance, contributed to overall performance in this insightful behavioral task.
I am excited to see what directions the authors take this work! Would enduring chronic pain for longer time periods erode this potential evolutionary advantage? Are the brain circuits that underlie this hypervigilance engaged by other prolonged negative experiences, such as chronic psychological stress, or are they specific to chronic pain? Are there other ways that chronic pain could confer an adaptive advantage? How does this finding reframe your perception of chronic pain?
Nora McCall, PhD, postdoctoral fellow, University of Pennsylvania, US
Patient Engagement in Research: More Than Just Food for Thought
Picture this: you are at a gourmet restaurant, looking forward to ordering a meal prepared by an expert chef. However, you are never shown a menu and the waitstaff do not take your order. Instead, you are served a chicken dish with peanut sauce. The meal is perfectly cooked, but there is a problem: you are vegetarian and you have a nut allergy. On paper, this is a gourmet meal that was prepared by an expert and should be delicious, however, because you were never asked about your preferences or dietary concerns, you cannot eat it.
The situation described above is a lot like what happens when we do not engage patients in research that is intended to benefit them. The dish served in the story is the research we publish, conducted by experts (the chef) and presenting robust findings. However, the dietary restrictions are the real-word concerns of patients, which can be mismatched with the research evidence when not considered. In order to link research efforts and findings with what is relevant to patients, research is turning more and more to patient engagement to ensure this connection is made.
Patient engagement means including patients in all stages of the research process to ensure their real-world perspective is accounted for, and the goal of this process is to ensure that research evidence is relevant to the groups it concerns (for more on patient-oriented research, see the Canadian Institutes of Health Research’s page on patient engagement here). While all researchers may agree that generalizability of their research is important to them, there is much work to be done in terms of researchers learning about how to approach patient partners, meaningfully engage patients in research (see the Chronic Pain Network’s tip sheet for recommendations), compensate patients for their time (check out Patient-Centered Outcomes Research Institute’s guidelines for patient compensation for some considerations), and acknowledge their contributions to published work (see Dr. Dawn Richards’ and colleagues’ article on guidance on authorship in patient-oriented research).
While patient engagement may be uncharted territory for some, through my own experiences with patient partners, I have learned that they have been extremely valuable in navigating the process with me as I have learned how to collaborate with patients as colleagues. Through these experiences and seeking learning opportunities, I have learned that the keys to successful patient engagement include communication, collaboration, and commitment to working together. If we can bring these elements to the table, we can be confident that we have set the stage for a respectful and meaningful collaboration.
It behooves researchers to engage with patients to ensure that pain research is conducted in a way that also addresses patient concerns so that evidence can be understood and utilized by all knowledge users. In order to bring the right dish to the table, dialogue and collaboration with patient partners is key.
Nicole MacKenzie, PhD student, Dalhousie University, Halifax, Canada
Last week, The New York Times, Reuters, and numerous other news and “news” sources have posted articles with headlines along the lines of “Star Wars Inspires Scientists to Create Artificial Skin That Can Feel.” Upon first seeing this, I thought, “what is this clickbait/pop science BS?” and hunted down the original research. The headlines aren’t so far off.
It was actually the principal investigator on the project, Dr. Benjamin Tee, who initially made the Star Wars connection. “Heavily inspired” by Luke’s robotic hand in The Empire Strikes Back, the Singapore research group has developed a “neuro-inspired artificial peripheral nervous system” called Asynchronously Coded Electronic Skin (ACES). This work, published in July of last year, made news again this summer as the lab presented their experiments with some new updates at the Robotics: Science and Systems virtual conference in July.
In conjunction with ACES, their new NeuTouch fingertip sensor is able to mimic rapidly-adapting mechanoreceptors (mechanically-sensitive peripheral neurons that fire at the onset and offset of pressure or indentation) like those of a human fingertip. At the robotics conference, they discussed their work that expanded upon touch sensors: their “visual-tactile spiking neural network.” When the NeuTouch sensor is used with a camera and the neural network, it allows for “visual-tactile sensation,” which is what we use when we look to grab something out of the fridge, for example, and is more accurate at recognizing objects than visual or tactile information alone.
This is not the first tactile-sensitive electronic skin, but it has improved upon some of the issues with previous ones. Tee’s team continues to make improvements based on the notion that an ideal e-skin should 1) allow for rapid and continuous sensory feedback to support decision-making based on sensory perception, 2) be scalable to cover larger areas and be distributed with variable spatial densities without overly complicated wiring, and 3) remain functional while being subject to harm. The lab has also developed a type of “self-healing electronic skin.” These technological advances could allow for people with prosthetics to better interact with their environments and improve their quality of life.
Anyone else laugh when Halle Berry explained that brain-healing foam in Kingsmen: The Golden Circle? Maybe in 40 years someone will be presenting something very similar at a conference.
Melanie Schaffler, PhD student, University of Pennsylvania, US
"Yet Another Bias in Science?"
Women in STEM (Science, Technology, Engineering and Mathematics) have been through a long history of struggles. From being denied access to higher education for centuries, to seeing the credit of their work go solely to their male supervisors, this has not been an easy ride. As we work through and fix most of these issues, new ones arrive and we become more aware of old ones. My latest personal favorite: survivorship bias.
Survivorship bias is the logical error of focusing on the people or things that "survived" some selection process and overlooking those that didn't. Because you ignore the failures, this bias can lead to very optimistic (often inaccurate) beliefs. A common example of this is Bill Gates (who dropped out of university and went on to become an extremely successful entrepreneur and, well, a billionaire) being hailed as an example of how ingenuity and hard work can be worth more than a university degree. What everyone seems to ignore is the millions of people who dropped out of university and did not end up a billionaire (they also seem to ignore he dropped out of Harvard). This, you may think, is not necessarily a big issue. After all, we can definitely still learn something from Bill Gates.
But it can be a big issue. The typical example of how problematic survivorship bias can be is that of someone assuming that an airplane crash wasn’t particularly dangerous because everyone they spoke to afterwards was alive. By ignoring the possibly dozens of people who did not survive the crash (whom we would obviously never be able to speak to), we can misevaluate the severity of the accident, which can prevent us from taking measures to make planes safer in the future.
Are we doing the same thing when we look at women in STEM?
If you attend a careers seminar targeted to female scientists, you will find speakers are likely to be extremely successful female professors. They will tell us about their experience and offer advice. This is great – I am sure we can all, men and women alike, learn from excellent scientists. But if our aim is to overcome the problem of underrepresentation of women in STEM research, I wonder if it is enough to look at the ones who have broken through this invisible barrier and succeeded.
As of 2010, women comprised 45% of doctoral students in the EU but only one-third of career researchers. So, in our path towards gender equality in STEM, maybe it’s just as important to focus on the female scientists who don’t make it, in order to figure out why that happens and how to fix it – but that’s probably an issue for several more blog posts…!
Elisa Clemente, PhD student, University College London, UK
Exercise: The Dr. Jekyll and Mr. Hyde for Those with Achilles Tendon Pain?
Chronic Achilles tendon pain is one of the most common overuse injuries in the lower extremities and is commonly referred to as Achilles tendinopathy. Hallmark symptoms include local pain at the Achilles tendon that worsens with activity. Similar to other pain conditions, it does not discriminate against who it affects. While Achilles tendinopathy is often associated with active individuals such as endurance runners, it can also impact sedentary individuals and everyone in between. The precise cause of Achilles tendinopathy is unknown, but a multitude of both intrinsic and extrinsic factors likely contribute to the development of symptoms.
During my time treating individuals with Achilles tendinopathy, I have noted symptom duration for some patients that extends beyond multiple years. When imagining an individual with persistent musculoskeletal pain, we may picture a person with diffuse and widespread symptoms. Interestingly, those with Achilles tendinopathy frequently report pain localized to just a portion of their tendon. The greatest level of evidence for rehabilitation of Achilles tendinopathy is exercise. I found, particularly with distance runners, the paradoxical relationship of exercise creating pain, yet the standard of care is additional exercise to decrease the pain. So, why do these individuals who experience pain for such a long duration demonstrate such pinpoint symptoms? Surely there must be a large amount of central nervous system sensitization occurring, right? Perhaps the answers to these questions may be embedded within what originally caused their symptoms – exercise.
Recent research has demonstrated limited evidence of central nervous system alterations in lower extremity tendinopathy [see here] and at the Achilles tendon specifically [see here]. This seems to contradict what we know about symptom duration and involvement of the central nervous system in pain processing. However, we also know that regular exercise (a possible contributing factor to Achilles tendinopathy) may provide a whole slew of benefits to help provide relief to those with persistent pain [see here]. Additionally, it may also help protect against the development of central nervous system involvement with chronic tendon pain. So, is exercise playing a dual role by being responsible for symptoms but also providing a protective mechanism for those with Achilles tendon pain? It is probably difficult to establish a definitive answer. However, these are the challenges that clinicians and researchers face which will require further exploration of this unique patient population with a seemingly contradictory harmful yet protective mechanism of injury.
Andrew Post, PhD student, University of Iowa, US
There’s No Blood Test for Persistent Pain – But Could There Be
Many people with persistent pain encounter profound difficulties in receiving a diagnosis. Part of the reason for this is purely practical: a diagnosis of chronic pain requires several tests to rule out other possible conditions causing the pain, a process that can take months or even years to complete. Unfortunately, too many patients also receive a lack of support from some healthcare professionals who may use the lack of visually observable features of the condition to deny care.
It’s often said, like many invisible disabilities, that ‘there’s no blood test for chronic pain,’ a phrase sometimes used more figuratively than literally to make the point that there are few ways outside of self-reporting to diagnose the condition. Of course, people who cannot self-report, such as young children and people with dementia, can’t rely on communication to relay their discomfort.
But could we take the phrase at face value, and make a blood test for chronic pain a reality?
A 2019 study, led by Alexander Niculescu at Indiana University School of Medicine, used a panel of 65 blood-borne biomarkers to detect chronic pain in patients. PRF published a news article on the study, which can be read here. To summarize, there were several markers that were highly sensitive to chronic pain, but the full panel of markers failed to describe a unique signature for the condition.
This is a problem we can expect to run into often – pain can be triggered by a dizzying variety of damage- and pathogen-associated molecular patterns that engage similar intra- and extracellular machinery in each case. Dramatic differences in how female and male immune systems are involved in pain onset and persistence adds further complexity to the issue.
There is certainly mounting evidence for distinct blood-borne signatures in different pain states. For example, recent work shows differences in the kynurenine and tetrahydrobiopterin pathways and in T cell and dendritic cell populations in people with complex regional pain syndrome. I am currently involved with similar studies looking at serum and whole blood to characterize type 1 diabetes patients with and without diabetic neuropathic pain, about which a paper is currently in press. Diabetic pain is a particularly difficult case since diabetes is already associated with widespread blood-related dysregulation compared to healthy controls. And while this work did not set out specifically to ‘create a blood test’ for pain, the idea that specific biomarkers of pain exist is critical to explore if we will identify better treatment targets.
I would be surprised if no combination of blood-borne biomarkers exists that is both necessary and sufficient to selectively diagnose a chronic pain condition. But a lot of work remains to figure out what the composition of this signature may be.
Jayden O’Brien, PhD student, University of Sydney, Australia
Abandoning Home for Abroad: Why Do We Do It?

A Brazilian, an Irishwoman, an Australian, and a Dane walk into a pub…. That could be the start of a great joke, but instead it’s just a casual Friday evening after a long week in the lab. Where I work, there’s a 50/50 policy, meaning roughly 50% of our academic staff are “internationals” (myself included), most of whom have relocated to Denmark exclusively for work.
Reflecting on this made me wonder: why do people move so far away from home for a job?
“Even before starting my masters, I could see the limitations for pursuing a scientific career in my own country: a lack of funding, a lot of bureaucracy and all too much politics. Don’t get me wrong, there are many good scientists back in Brazil, but they have all trained abroad,” reflects Priscilla Wittkopf. Priscilla therefore chose to move to England, where she got a handle on the English language, completed her PhD and a subsequent research assistant contract at Leeds Beckett.
Of course, personal interest and experience also comes into it. “I’d always wanted to live abroad and loved England. I also had an English teacher who had worked there, who could connect me with different people and tell me how the system worked,” says Priscilla.
After five years in England, Priscilla moved to Aalborg, Denmark, where she now works as a post-doc at the Center for Neuroplasticity and Pain (CNAP). “Now that I had international experience, this move was mainly for career progression’s sake – I wanted to go somewhere dedicated to my field [pain] where I could learn to use new equipment and methods among a good group of researchers…and CNAP ticked all those boxes.”
So, it seems the allure of greater opportunity, personal interest, building on social connections and career progression is what will make people (at least Priscilla and I) abandon their home nation for work. That, along with the fact that international experience is almost essential for an academic career these days. However, the past months have put a dampener on researcher mobility and have certainly reminded us “internationals” of the sacrifices that come with relocation.
“It’s already not a very stable period of your career,” Priscilla rightfully points out. Young researchers abroad are constantly on short-term contracts, often have the added stress of visas and new cultural expectations, and obviously have to leave things and people behind with each move…and now there’s the added uncertainty of this pandemic. Only time will tell whether international experience will continue to be a right-of-passage for scientists in the wake of the COVID-19 crisis, but for now, we’ll just sit back and enjoy our Friday beer in good multicultural company.
Megan McPhee Christensen, PhD Student, Aalborg University, Denmark
Depression, Dopamine, and Pain
At my institution, it is commonly cited that over 80% of chronic pain patients will have comorbid depression. Even more worrying is that on the inpatient psychiatric floor clinicians say that untreated pain is the number one indicator a depressed patient will attempt suicide.
Yet, when we study new chronic pain treatments, people with “comorbidities” tend to be removed from the population under investigation. Some comorbidities, like kidney disease, are primarily excluded for the safety of those involved in a trial. But comorbid psychiatric diagnoses, such as depression or anxiety, are also excluded. In a bid to treat pain alone, perhaps we are missing the point.
Numerous reviews and primary articles have set out to address potential underlying molecular, cellular, and circuit-level pathologies associated with this common comorbidity. The concept of dual-targeting exists in the pain field, as does prescribing off-label, but there has not been a combined effort to address treatment specifically of the pain-depression comorbidity. Perhaps we are witnessing that 17-year gap between original research and its implementation in medical practice, but this is a tragic and massive population to miss.
Outside of my microcosm, the action of midbrain dopamine, especially as it projects to the prefrontal cortex, has been implicated in depressive states. More specifically, there are calls to investigate increasing the dopamine in these synapses to improve depressive symptoms. Indeed, it is partly by this mechanism that serotonin-dopamine reuptake inhibitors, a class of antidepressants, are proposed to work.
All of which led me to reflect once again on my own focus. After a grant rejection, reflection is always important. In the dopamine field, we talk a lot about reward and potentiation of circuits. The addiction potential of opioids has led us and others to search for a quality analgesic that does not have the same dopamine surge.
Yet when I reflect on the efficacy of certain antidepressants in chronic pain states and the way depression and pain seem to potentiate each other, I question if this is fundamentally possible. If pain (or depression) is modeled as a chronic aversive state, do you not require reward to alleviate it? Could you have reward but not addiction or habit formation?
As we further investigate treatments as well as systems neuroscience, I invite readers to continue to bring these questions to the fore. It may be that in examining the comorbid state we will better understand the two individual states, as we may compare across all three groups. Additionally, as we search for better treatments for pain, reflecting on our underlying presumptions of which targets exist, or may be possible to separate, will be critical in progressing.
Sage Morison, MD/PhD student, Northwestern University, US
Week 4: Monday, August 3, 2020
Oxytocin Neurons: Why “Air Hugs” Are Just Not the Same
When Patients Are Excluded From Knowledge Generation, Peer-Led Care Means Little
What Are We Measuring and Treating in Our Model Systems?
Oxytocin Neurons: Why “Air Hugs" Are Just Not the Same
Oxytocin, often affectionately referred to as the “love hormone,” is both a neuropeptide and hormone that plays an important role in social bonding, reproduction, childbirth, and lactation. It’s made in the hypothalamus, a small brain region that interacts directly with the endocrine system, receiving information from circulating hormones and, in turn, regulating hormone release. Most (97%) oxytocin neurons in the hypothalamus are large (magnocellular) and directly project to the pituitary gland to cause the release of oxytocin into the blood. Small (parvocellular) oxytocin neurons, representing the other 3%, transmit signals to their magnocellular counterparts.
Despite all of the evidence that oxytocin promotes various types of social behavior and is released into the bloodstream in various social contexts, the activity of oxytocin neurons during social interactions remained unexplored until now. A recent study in rats by Tang et al. found the following:
1. Oxytocin neurons are activated during social interaction, which may not come as a surprise. Many studies have shown that oxytocin is released into the extracellular fluid during social interaction, but this is the first time that activity of the oxytocin neurons themselves has been recorded during social behavior.
2. Social behavior with physical contact increases oxytocin neuron activity more than interaction without touch. Interestingly, even touch that isn’t social (air puff to the back) activates oxytocin neurons.
3. The parvocellular oxytocin neurons 1) respond to touch stimuli and 2) control magnocellular oxytocin neuron activity. Further, parvocellular neuron activity appears to alter social motivation, as activation or inhibition increased or decreased the amount of time of social interaction, respectively.
The authors propose that it is the parvocellular neurons that take somatosensory information and send it to the magnocellular neurons to release oxytocin to promote social interaction.
This paper not only suggests that gentle touch promotes social interactions, but also provides the basis of a circuit for how. If touch from a friend activates parvocellular oxytocin neurons, and this activity promotes social behavior, are friendships formed without touch bypassing an important circuit that would strengthen the friendship? Now that most of our social communication is virtual or six feet away (or should be, United States), are you noticing a decrease in your social motivation? Do you feel your existing social bonds weakening without touch?
Melanie Schaffler, PhD student, University of Pennsylvania, US
When Patients Are Excluded From Knowledge Generation, Peer-Led Care Means Little
People with lived experience of persistent pain increasingly play an active role in delivering patient care. These peer-led models involve chronic pain patients or carers delivering pain management programs to other patients, in the place of healthcare providers. Examples of this approach include a trial of a peer-delivered cognitive behavioural therapy program for people with diabetic neuropathic pain, a peer mentoring program for adolescents living with chronic pain, and many others.
The approach is often marketed, in the peer volunteer case, as a cost-efficient way to increase the availability of care. More pertinently, the approach recognizes the patient as an expert in their own experience, and therefore as indispensable in assisting others with similar experiences. The rationale is a sensible one – who would have a better knowledge of how to assist people in pain than those who have spent years managing their own?
A recently published clinical trial by Matthias and colleagues investigated the efficacy of a peer volunteering program for improving pain management skills in persistent pain patients. They reported no significant difference in pain outcomes between treatment and control groups. The authors explained this by noting that only 13% of patients contacted their peer volunteer the minimum recommended number of times. It seems like engagement on both ends – patient and peer – was difficult to guarantee.
Why might this be the case? Consider that in these trials, the peer volunteers have been trained in a program whose contents were designed without input from the peers themselves. When people with lived experience deliver programs developed without reference to that lived experience, where is the opportunity for their experience to meaningfully inform care?
This is a problem that is not limited to the pain field. In my five years as an advisor to a large youth mental health service in Australia, the advisory process was, by design, compartmentalized away from any aspect of how clinicians were actually providing their care. Even with the introduction of peer workers – people with lived experience in paid employment to assist other patients – these patients were nevertheless receiving their primary care from a clinician without that kind of knowledge. Though psychological care must, of course, be delivered by appropriately qualified professionals, the information upon which clinicians base their practice has been largely assembled without meaningful reference to the experiences of the patients they seek to assist.
The most efficient way to utilize lived experience in the care of chronic pain patients is to explicitly include the patient voice not just in knowledge delivery, but in the production of clinical knowledge itself. Initiatives to involve patients in all stages of the research process are few, but steadily increasing in number. PRF has previously published a podcast on the importance of meaningful patient-researcher partnerships. I could certainly do a lot more to prioritize this in my research.
Clinical knowledge itself must be patient oriented. Otherwise, we are proceeding with one hand tied behind our backs.
Jayden O’Brien, PhD student, University of Sydney, Australia
Let they who’ve never said this incredibly annoying catchphrase cast the first stone.
“No pain, no gain” must be one of the most widely recognized exercise mottos. Wikipedia tells me it became popularized in the early 1980s, through Jane Fonda’s workout videos, but a variation of it (“According to the pain is the gain”) has apparently been seen as early as the second century CE, in the classic Jewish text Ethics of the Fathers. Along those lines, we have the chorus of Kelly Clarkson’s song, “Stronger (What Doesn’t Kill You),” which drew inspiration from Friedrich Nietzsche’s “What does not kill me makes me stronger” (which, by the way, is objectively inaccurate: A broken arm will neither kill you nor make you stronger). Finally, the idea that making personal sacrifices (for others, God, or a “Greater Good”) is something to aspire to seems prevalent across time and cultures.
But where does everyone’s obsession with pain come from? Why this notion that there is some sort of moral value in enduring suffering?
Here’s my (not particularly evidence-based) theory: The perceived moral value of enduring pain comes from the fact that this behavior is against our nature. I’ll explain.
There is a saying that goes “self-preservation is the first law of nature,” that is, living organisms prioritize their survival over everything else. Most decisions taken by animals aim to meet different physiological needs, with survival as the ultimate goal. (An exception to this occurs when the survival of the individual “undermines” the overall chances of survival of the species – in which case you may see parents sacrificing themselves for their younger, healthier offspring, for example).
Pain clearly plays a crucial role in this self-preservation. After all, it is pain that prompts us to avoid potentially harmful stimuli, protect affected body parts during healing, and avoid similar dangerous situations in the future. Its unpleasant nature means most animals do their very best to avoid it at all times.
It seems that we (humans) are an exception to this rule. While most of us don’t actively seek extreme pain, we routinely put ourselves in situations where some degree of suffering is involved. We ignore this basic survival instinct and rationally decide that accomplishing some particular goal outweighs the unpleasantness of the pain required to achieve it. Other animals don’t really do this. If a zebra keeps running despite feeling its muscles ache, it’s usually because a lion is hunting it – not because it wants to get “beach body ready” (whatever that actually means).
In short, undergoing pain for reasons other than survival tells us apart from (probably) every other animal species – and that makes us feel special! This, I argue, primarily explains the moral value we attribute to overcoming it.
So next time someone tells you “no pain, no gain,” feel free to ask them whether this sense of superiority over other species in the Kingdom Animalia (which includes, for example, termites, which eat one another’s faeces) really is worth the pain!
Elisa Clemente, PhD student, University College London, UK
COVID-19 has brought about quite a bit of change to our world. It has impacted research, how students and instructors approach education, and healthcare delivery, and by now everyone is all too familiar with Zoom meetings. My friends and family from around the country have all reported changes to their lives due to the current pandemic. These experiences vary from person to person, with each individual having a unique perspective on how the pandemic has touched their life over the past few months.
So how does this relate at all to pain? In 2019, Roos et al. published an article in the British Journal of Sports Medicine titled, “It is good to feel better, but better to feel good….” The authors examined data from an article in the New England Journal of Medicine that examined individuals with anterior cruciate ligament (ACL) tears and outcomes for two intervention groups: exercise plus early ACL surgical reconstruction versus exercise and delayed ACL reconstruction. The original article from NEJM reported no significant difference between the groups at two-year follow-up. But Roos et al. examined the data for subtleties in outcomes related to patient-perceived satisfaction and posed the question, “What is successful treatment?” The authors found a proportion of participants who did not meet cut-off scores that those participants would deem as satisfactory, with a smaller group thinking that their treatment had failed. From these findings, the authors suggested the use of questions about patient perceptions of their care and current status in combination with standardized outcome measures, as this may provide a richer understanding of the overall effect of treatments in clinical trials.
All the participants in the original study had the same diagnosis: an ACL tear. Yet the perceived experience and satisfaction were not uniform. Similarly, we are all going through the COVID-19 pandemic together, but our experiences during this time vary. This may parallel patients we treat with persistent pain; the diagnosis may be one that we have seen before, yet the individual’s pain experience is unique to that person and shaped by a multitude of factors. The patient may also achieve a score on an outcome measure that we deem as a “minimal clinically important difference,” but the patient’s perception of this change may not agree. Thus, similar to the title of the BJSM article, we may consider reframing our idea of clinical improvement by asking questions to explore if someone not only feels better, but if they feel good about that improvement.
Andrew Post, PhD student, University of Iowa, US
It’s been said that a picture is worth a thousand words. When it comes to pain research, however, what are actual patient words worth when it comes to understanding this sensation?
One of the primary goals of quantitative research is to describe trends in data and find consistencies in them. We look for ways to predict how one variable will behave in the presence of another and typically, when a data point diverges, though we explore it, that data point is excluded. The fact is, however, that the behavior of people in the real world cannot be explained with a single trend or line of best fit. There is nuance in human experience and perspective in the real world that we are limited in understanding when doing quantitative research.
Qualitative research allows us to explore these nuances, and when it comes to pain, qualitative methodologies can allow us to explore the diverse range of the human experience of pain. Consider, for example, a research question regarding a patient’s cancer pain. While the aspects of the diagnosis and symptoms may be correlated with or predict pain ratings, that data do not explore the experience of pain and how it was influenced by frequent procedure pain, the intensity of treatment side effects, and fear of cancer returning. Both sets of findings hold great relevance to the patient’s pain related to their cancer, but the themes explored in the qualitative results present a much richer and more nuanced exploration of the patient’s experience that could actually further explain or contextualize the quantitative findings.
Conducting research with a qualitative methodology can not only bring lived experience to research but also a great deal of clinical relevance. Not only are participants able to contextualize their responses and perspectives through their own clinical experiences, but this also creates illustrations where researchers and healthcare providers can see themselves in the data and how they may relate to the experience of the participants. Qualitative methods may be particularly relevant in pain, especially with the recent emphasis on the definition of pain, where the individual’s experience and report of pain must be respected, and because of the clinical reliance on self-report of pain. Given the value of one’s experience of pain clinically, conducting research where individuals describe these experiences can meaningfully further our understanding of factors that may influence that experience of pain. The human element of qualitative data is therefore a rich component of this methodology and situates data within a “real world” context.
While qualitative research can provide a rich and diverse method through which to explore human experiences and perspectives, it may not always be the most appropriate technique to address every research question. Qualitative methods allow researchers to look at a range of experiences, to which each participant will bring a unique perspective. Exploring a full range of experiences may not always be an appropriate or desirable approach to answering one’s research question. However, if one is interested in understanding how individuals experience a phenomenon or how specific occurrences may relate to the experience of pain, it is an appropriate and valuable method to answer these types of questions.
In sum, qualitative methodologies can offer rich descriptions of lived experiences and are particularly valuable when it comes to describing pain-related experiences that can be nuanced and complex. Harnessing the power of lived experiences and sharing direct quotations from participants, qualitative research can weave together a story that describes a real-world clinical matter and injects a human element into the research process.
Interested in reading more about qualitative research in pain? Check out the Canadian Journal of Pain’s special issue on this topic, launching next month.
Nicole MacKenzie, PhD student, Dalhousie University, Halifax, Canada
As I was flicking through my emails, I stumbled upon an alert about this article, which looks at how an empathetic interaction can increase pain inhibitory capacity and analgesic responses to manual therapy. In the clinic, we know that a strong, compassionate therapeutic alliance can do wonders for treatment success. However, reading this article made me think, How much can the experimenter-participant relationship influence our results in non-clinical work?
We human beings are social creatures by nature. That means we, often unconsciously, adapt our behavior to suit the social context in which we find ourselves. Many have explored the effects of different concrete interpersonal factors on pain and other outcomes in experiments, finding that experimenter gender and appearance can influence results. Despite these findings, it’s rare to come across an article that specifies "experimenter characteristics" in as much detail as those of the participants.
Perhaps this is because researchers are already good at being consistent – using the same people, the same equipment, the same environment, even the same standardized script for every participant from the moment they enter the room. I know this is what I strive to do, but even if this is the case, participants can be unpredictable, especially during experimental pain testing. For example, some participants are anxious about what you’re going to do to them, some are eager to try everything (preferably all at once), others are excessively talkative and want to chat about everything except what you’re currently doing, and some barely say a word the entire session. It’s near impossible to respond to all of these different behaviors in a standardized manner, but it seems our response, whether that be to ignore, interact, or intervene, may have an influence on what we find.
Unfortunately, I have no great solution to propose, but I do think this is important to keep in mind. Unless we make everything computerized and take the experimenter out entirely, there will always be some level of confounding influence from the experimenter-participant interaction. And you know, maybe this is why, despite clear impairment upon meta-analysis, I personally couldn’t find evidence for lacking of pain inhibition among patients with chronic low back pain in my most recent work – perhaps I’m just too nice?
Megan McPhee Christensen, PhD Student, Aalborg University, Denmark
What Are We Measuring and Treating in Our Model Systems?
It’s after hours, the lab is quiet and dark, and I finally have time to sit and read a review. As soon as the shelter-in-place orders started rolling in globally, my lab started joking that someone was going to have to start a journal just for all the review papers. With everyone sitting at home indefinitely, individuals and the field at large have had time to think, and to write.
I actually love to read reviews. To me, they are the scientific equivalent of a pointillism painting. Reviews are the space for experts to propose their thoughts about how diverse, intricate data fit together to make a more complete picture.
On the docket tonight is a review on neuropathic pain. IASP defines neuropathic pain as “Pain caused by a lesion or disease of the somatosensory nervous system,” in other words, pain that originated in nerve damage. Yet in the rodent models I and so many others use, “neuropathic pain” essentially means “known hypersensitivity to foot poking, especially if we have cut, crushed, or constricted the nerve.” It’s a telling translation, which focuses more on non-pain symptoms, as it must. Pain at this time is a state and experience that must be self-reported.
In discussions of translational science regarding psychiatric pharmacology, many have come to focus on our inability to appropriately assess the inner state of a mouse – how difficult it is to try to develop treatments for an inner state in humans when we cannot ask a mouse how it’s feeling. As I was reading through this review of the field I was reminded that we are shifting our focus in neuropathic and chronic pain to central, higher-level processing.
More importantly, many first-line treatments for neuropathic and chronic pain states are psychiatric pharmacology. For example, serotonin-norepinephrine reuptake inhibitors were developed to treat depression but have strong, evidence-based use in chronic and neuropathic pain. While our definition of neuropathic pain remains somewhat peripherally focused, treatments have become increasingly central. As we move forward, then, it is increasingly critical to ask ourselves what symptoms we are truly measuring and alleviating in our model systems.
I have said before that I view pain as an unexplored window into human perception, and it is clear as we take our science into medical practice that attending to that perceptive state is critical in healing people with pain disorders.
Sage Morison, MD/PhD student, Northwestern University, US
Over a year into my postdoc, I am finally starting to recover from the fatigue induced by defending my dissertation. Indeed, adjusting to a new field and my lab role as a postdoc feels like it’s taken Longer Than It Should Have. Despite this, I think my biggest change since starting my postdoc has been an improvement in my ability to respond to feelings like this one that result from imposter syndrome: the feeling that one is unqualified despite evidence to the contrary. I think I’ve been able to make this change as I’ve become more comfortable with being vulnerable about my struggles.
As scientists, it is easy to feel like we must know everything about our field and do everything perfectly all the time, right from the beginning, and that there is little room for imperfection. Two particularly challenging imposter syndrome situations for me are comparing myself to high-achieving peers – “She started her postdoc after me and already has a grant!” – and berating myself for not knowing What I Should Already Know – “I should already be an expert in setting up this piece of equipment; I shouldn’t have to ask for help.” In these instances, I think that my postgraduate school fatigue has helped me, surprisingly, by making it easier for me to realize that I cannot be perfect at everything, all the time, without burning out (and burnout is both unpleasant and inefficient!). This perspective has helped me pause my negative thoughts, talk to a friend or colleague, and reframe the situation. Rather than berate myself for being “behind,” I am trying to look at others' successes and see what parts of their approach to success might help me. Rather than “freeze” because I have forgotten a detail – a very big problem for graduate student Nora! – I am getting better at jumping to Google or asking a friend without feeling ashamed. Now, am I perfect at implementing these things? Absolutely not! However, being vulnerable enough to talk about my struggles has gotten easier with practice, and this has made my progress as a postdoc much smoother.
While I am still dealing with my imposter syndrome, I am proud of my progress, and I am excited to keep improving. This pride in my ability to change my opinion of myself is possibly the biggest shift in my perspective since starting graduate school. As I become a mentor myself, I want to prioritize teaching trainees how to recognize and confront imposter syndrome in ways that work for them. For me personally, Twitter has been instrumental for learning I am not alone in my struggles or imposter syndrome, and that there are many different ways to be a good postdoc. If you experience imposter syndrome, how do you manage it? Have you found vulnerability has helped you?
Nora McCall, PhD, postdoctoral fellow, University of Pennsylvania, US
Week 3: Monday, July 27, 2020
How Do Children Fit Into the Definition of Pain?
Creating Meaning in Our Patient Education
#SoMe: Generating Impact or Inflating Indices?
Just Because You Can Doesn’t Mean You Should
A Boost of Dopamine to Ease Pain?
The Boring Stuff in Research? Get a Computer to Do It
The COVID Nasal Swab: A Timely Example of Sensation
I am a scientist. I am a strong advocate for human rights. I do stand-up comedy and satire writing. For many people, these three statements look incompatible: How can you have a funny, humane scientist? (We're assuming, for the sake of argument, that I'm funny and a real scientist – both of which are debatable).
People outside science, particularly children, often don't think of scientists as “real people,” as just like everybody else. For example, a Portuguese science outreach program, "Cartas Com Ciência" (Letters with Science), challenged 8- to 12-year-olds to submit questions they would like to ask a scientist. One of the top two most asked questions was, “What do scientists do in their free time?” I was disappointed but not surprised. Not in those children; it’s not their fault – but in us, the scientists.
These children’s interest in learning about what scientists spend their free time doing is, in my opinion, a testament to the image they have of us: crazy, serious, white old men in lab coats, running experiments for no real reason other than to satisfy their (often times, largely unhealthy) curiosity, showing a great disregard for ethics, the rest of society and, even, the law. Essentially, a mix between Albert Einstein and nearly every scientist in a sci-fi movie. So how could they have normal hobbies?
More importantly, however, if this is how we are perceived, how are young people supposed to know that science is for everyone – that science could be for each one of them, too?
It would be only too easy to blame this on the movie industry and its stereotype-based misrepresentation of scientists, and to demand change to come from them – but Hollywood has far more pressing representation issues to solve. It’s up to us, scientists, to fix this one. We must step down from the ivory tower of academia and interact with the people who, ultimately, benefit from and fund a lot of our work: everyone else.
While there is still much room for improvement, I feel hopeful. In the UK, for example, public engagement activities are becoming increasingly important in academia, often working as a factor to weigh in when considering promotions and grants. A number of science communication initiatives, such as Pint of Science and Soapbox Science, have spread to dozens of countries all over the world, and there are wonderful charities, like The Brilliant Club, working tirelessly to increase the number of pupils from underrepresented backgrounds progressing to university.
Finally, there is also a wave of people using comedy (e.g., Science Showoff, Bright Club) to get an even wider reach – and why not? It’s true that humor is subjective, but laughter is contagious and “the best medicine”! Is there a better way to show that scientists can be approachable and down-to-earth, while also communicating our work, than through comedy?
For example, a book title and author you’ll never see:
Elisa Clemente, PhD student, University College London, UK
How Do Children Fit Into the Definition of Pain?
The revision of the definition of pain was 40 years in the making, spanning a period of time during which the study and treatment of pain changed dramatically. Consider, for example, that in 1979, when the original definition was published, it was not yet widely known that infants could even feel pain and were still undergoing surgery without proper anesthesia. Fortunately, the field of pain has advanced substantially since then, including an increased focus on pediatric pain. The revised definition of pain not only reflects how our understanding of pain has developed generally, but the definition and its key notes may also have important implications for our youngest patients.
One of the key notes that is particularly relevant to pediatric pain is the statement that individuals learn the concept of pain. This learning not only has implications for how children physically experience pain, but how they conceptualize it as well. Through observation of other’s responses to their own pain, children begin to learn how to react to pain, whether pain is something to fear, and if their pain is something that will be taken seriously. Therefore, the statement that pain is learned is more than simply a recognition about how a sensation is learned over time, but rather encompasses the experiences and cognitions associated with pain in this learning process. There is significant evidence to show that children react to, and learn from, psychological and social aspects of pain, such as memories and parent reactions. This phase of the lifespan is therefore particularly relevant to this key note, as the opportunity to make learning about pain a constructive and positive experience in childhood is paramount. This key note is thus an important reminder of the importance of appropriately managing pain experiences early in life.
Given how dynamic the experience of learning the concept of pain is in childhood, the formal recognition that pain is a biological, psychological, and social experience is critical to opening important avenues to understanding and treating children’s pain. Recognition that pain can influence, and be influenced by, psychosocial processes should afford greater possibilities for seeking psychological or other relevant services for the child. By sharing the conceptualization that pain is a biological, psychological, and social experience with parents, this may also help them learn to see their child’s pain differently and seek other supports for pain management where appropriate.
Finally, it is important to address the inclusion of the key note stating that verbal descriptions are only one method by which to express pain. This has great significance to our infant, toddler, and other non-verbal pediatric patients. Facilitating a meaningful assessment of pain through other modalities is critically important in these particular pediatric populations and can contribute to supporting positive learning about the concept of pain. Furthermore, continued use of other methods of pain reporting and assessment contributes to the goal of respecting all reports of pain, another key note. By providing children with developmentally appropriate methods to report pain and treating their reports as valid, children can gain access to appropriate pain management.
While many of the concepts highlighted here are implemented in clinical practice, and there are certainly more specific points that could be raised in regard to pediatric pain, these key notes are important reminders of the various considerations to address the needs of our youngest patients. These points are important for researchers, clinicians, and the public to consider and will spark important discussions on how we think about pediatric pain.
Nicole MacKenzie, PhD student, Dalhousie University, Halifax, Canada
Creating Meaning in Our Patient Education
I can vividly recall the first patient I saw in the clinic who had persistent, widespread pain. Her symptoms had lasted for years, and I was excited to use my newfound knowledge of the physiology of pain, to share what I knew, and communicate how this could help her. I should have known how horribly wrong I would be. After going through peripheral pain neurophysiology and how supraspinal structures process nociceptive signals, the first question she asked me was, “So, you’re saying this is all in my head?” At that moment, I knew I had failed her. This led to a complicated, sometimes turbulent, course of care over the following year.
So how do we know what to say to our patients in these situations? Are there any clinical “cues,” individual characteristics, or outcomes we can use as clinicians and researchers to inform the manner in which we communicate the purpose of our interventions to “match” the understanding of our patients? A recent emphasis in the literature on patient-centered language is communication that is reflective, non-threatening, and demonstrates interest while also validating the perspective of the individual we are working with. But, what about education on pain, particularly persistent pain conditions? Do we need to reel in how advanced our jargon is to ensure that our patients fully comprehend the subject matter? Other studies and literature might suggest otherwise, and we may even be underestimating the abilities of our patients to grasp pain-related concepts.
Reflecting back, I am thankful for the relationship that I had with this individual. Having the opportunity to work with her impacted both my clinical practice and approach to research. She was later treated by a co-worker in my clinic for the same persistent pain, and my co-worker reported a “light bulb” moment in which the educational strategy he used to explain pain physiology was perceived as beneficial by the patient. She ended up writing me a letter a year after that reflected on our relationship and the education she received on her chronic pain. While I won’t divulge any other specifics, the next time she was in the clinic, we spoke briefly, she got emotional, I teared up, we hugged, and then we moved on to the next thing we had to accomplish for the day knowing we had both made an impact on the other; probably she had more of an impact on me.
Maybe each individual’s receptiveness to information is different; some benefit from the “long-game” while others will appreciate a swifter delivery of pain knowledge. Regardless of whether we ease into our pain education or deliver it all up front, consideration of our phrasing to match the readiness and openness of our patients to this information, instead of imposing medical jargon, may end up helping our words mean just that much more.
Andrew Post, PhD student, University of Iowa, US
#SoMe: Generating Impact or Inflating Indices?
It’s no secret that academics are under ever-increasing pressure to publish. Publications, in many institutions, are what ultimately decides who gets hired, who gets fired, who gets funded and who eventually gets tenure…but beyond lengthening your CV and maybe landing you your next grant, how do you make sure that all these publications actually make it to the people that need to read them?
Social media seems to be the answer. At least that’s what the results of a recent RCT would have you believe, showing that just a single tweet of an article can increase citations almost 10-fold in the following year (see the full paper here). This relationship between tweets and citations was exposed almost a decade ago (which you can read about, e.g., here) but now we can see that it actually is the tweet that seems to be responsible for driving citations up, not the quality, novelty, resonance, etc., of the article itself.
On brief consideration, this is great! Evidently, all we need to do is set up a Twitter account, find some followers, and get tweeting. Readers reached. Dissemination done. Check. On deeper consideration, though, it’s a little unnerving. After all, if 280 characters are enough to persuade someone that our work is worth citing, why did we bother writing the 20-page article about it?
Social media is undeniably a great tool to socialize with collaborators, keep up to date, share new findings and discuss discoveries with peers. But we also need to remember that humans are plagued by cognitive bias and tweets seem to be a prime way to tap into that.
Is this a problem? Maybe not on an individual level. We all have access to Twitter and clearly it does increase the visibility of our work, so this is worth exploiting if you’re an up-and-coming researcher. The potential issue is when we start to make bigger decisions (grants, tenure, etc.) based on social media views or resultant citation counts alone. Sure, alternative metrics capturing this (e.g., altmetrics) may be a decent yardstick for quantifying viewer numbers, but it’s still not clear how well they (if at all) reflect the quality and significance of scientific findings, nor if “views” really equate to meaningful impact.
Social media is obviously a powerful tool – but, to quote Uncle Ben, “with great power comes great responsibility.”
Megan McPhee Christensen, PhD Student, Aalborg University, Denmark
Just Because You Can Doesn’t Mean You Should
Is your science ethical? This is not a question of whether you are honest and responsible in conducting and publishing your work, or ensuring the safety and confidentiality of your subjects, but a question of whether your work has a positive impact on society. One might argue that any contribution to our understanding of biology has value. However, science does not exist in a vacuum, and biology has a history of being weaponized against marginalized groups (i.e., the US eugenics movement).
A recent paper touting “evidence that bisexual-identified men tend to show bisexual arousal patterns” attempts to use science to validate an identity. Simply starting/funding this work seems to suggest that identities/experiences are not “real” until we scientifically quantify them. And what if the outcome of this experiment were different? How might someone overinterpret those results as an excuse to deny protections for bisexual-identifying men? The best research questions are those that aim to explore or describe biology where any outcome in any direction is meaningful, rather than “show” or “explain” phenomena. But if one of your outcomes has the potential to harm already disenfranchised groups and negatively impact society, one could argue that the potential harm of the research outweighs any potential good.
For example, work from our lab has found that different inbred strains of mice have different responses to painful stimuli. This information is useful and meaningful for other pain researchers who use rodent models, as it is possible that the background strain of a genetic line influences a behavioral phenotype. A logical follow-up would be to determine which gene(s) is responsible for the differences in pain behavior, and based on those results, one might search for an analogous biomarker for pain in humans.
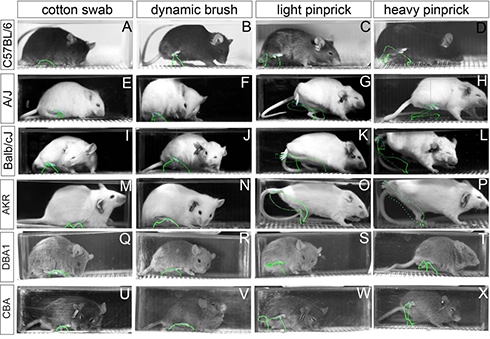
Ideally, that work could improve treatments for pain by removing some subjectivity, as there is currently racial bias in both pain assessment and pain treatment. However, could some outcome of that research provide justification for limiting access to adequate pain management for some people? Could it mean that self-report will no longer be valid, and what might the ramifications of that be? Concurrent with research into pain biomarkers should be conversations about how to interpret such results and the ethics of how they might impact medicine.
Melanie Schaffler, PhD student, University of Pennsylvania, US
A Boost of Dopamine to Ease Pain?
On my first day in the interventional pain clinic, the chief fellow told me something I had heard many times before. Patients with long-term pain don’t respond to opioids. But he went further, saying it’s as if they’re already tolerant, meaning they have diminished response to opioids even without having used them before.
I have heard this repeated so many times it seems like folklore; everyone agrees that patients who have had pain for a long time need higher doses of opioids to achieve the same effect. This is concerning, medically, since higher doses are more addictive and more dangerous. However, it’s also intriguing neurologically. Where in the entire pain processing circuitry, from peripheral nerves to emotion-associated brain areas, could changes have occurred that mimic taking opioids before opioids are administered?
Why does chronic pain look like opioid tolerance? It’s at this intersection that I have spent the better part of a year. I am not sure we have a better understanding of where this road is going, just a few more landmarks to add to the map.
One answer seems to be that long-term pain is associated with altered addiction circuitry. Specifically, rodents with nerve injuries have decreased dopamine release in the presence of rewards, including opioids. Dopamine is commonly referred to in the press as the “reward” neurotransmitter, one of the “happy” neurotransmitters, and is promoted as a chemical that can make you feel pleasure, motivation, and reward. Dopamine actually has numerous described functions, but the dopamine blocked in the presence of chronic pain is that reward- pulse dopamine. It is the dopamine that rushes in after a bite of chocolate or seeing a loved one’s face or, yes, a hit of cocaine.
Morphine and other opioids increase this dopamine, which has long been proposed as the mechanism behind their addictive potential. One major goal of deciphering the specifics of this circuit is to provide pain relief without such high addiction rates. But if long-term pain is directly decreasing reward dopamine, and opioids work through that same dopamine signal, the question becomes whether that signal is necessary for pain relief. If so, preventing this change could be integral to providing pain relief to patients who cannot get it from opioids.
While my own work revolves around finessing the smallest possible neuronal population, it is informed by a recently completed clinical trial which applied the general theory that more dopamine should equal more reward signal and less pain. The addition of a dopamine precursor to a pain treatment regimen did have a strong pain relief effect, predominantly in females. Our hope is that identifying a molecular marker for the exact dopamine neurons in question, and not simply every cell that uses dopamine, will help increase and generalize this effect.
I wrote previously on the importance of including the confound-ridden world of human data in molecular science. The medical observation of pre-existing opioid tolerance in pain patients has been brought all the way down to the level of one sub-population of dopamine neurons, which I manipulate. Ideally, we will be able to target them pharmacologically, and one day we’ll be able to say to medical students that while opioids don’t work, exploration of that led to new ideas about how to provide relief, and a more mechanistic understanding of pain.
Sage Morison, MD/PhD student, Northwestern University, US
The Boring Stuff in Research? Get a Computer to Do It
I have a computer science friend whom I rib for his tendency to enthusiastically advocate the virtues of programming to me. “It’s the skill that every office worker will need within 10 years,” he would say, as I nod politely and glance absentmindedly at the unsolicited links to online coding courses he would send. Buzzwords like “productivity” and “efficiency” were insufficient to curtail my obduracy. I reasoned that by the time I learned how to code and then wrote the code to solve a problem, I may as well have solved it manually.
Then the pandemic occurred. Locked out of my lab for the past few months, I’ve spent a lot of time pondering ways to increase my efficiency for when the lab becomes available again.
Working in research is exciting – there are few careers that involve such a wide range of day-to-day activities and skills. However, I often spend a distressing amount of time doing repetitive tasks for days or even weeks at a time, be it analyzing microscope images, formatting graphs, or mind-numbingly copying information from one spreadsheet to another. That time could be better spent.
More importantly, this stuff is boring.
It was a good time to know of a better way to go about this. Sheepishly, I reached out to my computer science friend and some early career researchers, and skilled up. I’ve begun using R to automate some statistical analysis I would usually do in other software. Now, I don’t need to individually copy spreadsheets into GraphPad Prism and run the same ANOVA over and over again on different sets of data. Working with large data sets also became far more manageable.
Using macros in programs like FIJI means I can batch analyze a set of micrographs overnight rather than sitting at the computer and clicking on menu buttons for hours. The University of Melbourne’s Advanced Microscopy Facility has some great resources on this topic. But there are some programs that don’t have any macro compatibility, so I’m also beginning to use Python (specifically, the PyAutoGui package) to take control of my keyboard and mouse and interact with any program on the screen as though I were clicking and typing myself. The freely available web book Automate the Boring Stuff with Python came in very handy for learning this.
My computer science friend is very pleased that I’m a convert. So am I.
Jayden O’Brien, PhD student, University of Sydney, Australia
The COVID Nasal Swab: A Timely Example of Sensation
More people around the world are being tested for COVID-19, and the nasal swab is often used to collect specimens. As a neuroscientist studying sensation and associated emotion, I am quite curious about how the sensory and affective experience of this unique tactile experience varies across people. During the test, a swab is inserted up the nose and is twirled around the nasal cavity, brushing for several seconds. This protocol is the same for the nasopharyngeal test and the anterior nasal swab (the latter doesn't go as far into the nostril).
The overall consensus is that this sensation is not painful per se, though no one has described it as pleasant. Anecdotally, I’ve seen and heard a range of experiences, from burning and stinging, to triggering headaches and gagging, to the sensation of needing to sneeze. “Discomfort” is one of the most common descriptors, as is eye watering triggered by activation of the nasolacrimal reflex (tearing that occurs from stimulating nasal mucosa and activating the lacrimal nerve, a branch of the ophthalmic nerve, which itself branches from the trigeminal nerve, cranial nerve 5). Indeed, tears were one of the chosen metrics in a 2002 publication comparing the two nasal collection methods in children. The authors compared the two methods with self-reported pain scores and investigator-scored facial discomfort scores from videos; crying duration was the metric for their youngest subjects under three years of age (medians of 5 seconds and 20 seconds of crying for nasopharyngeal and anterior nasal swabs, respectively – ufdah!).
A description of a personal account in the San Diego Union-Tribune caught my attention: “It never hurt, but it felt like it was about to hurt.” This anecdote demonstrates how expectation is a key component of sensation, and ties into what we know about placebo, nocebo and pain. Indeed, social and physical cues, and verbal suggestion surrounding treatment, can promote health (placebo) or distress (nocebo). Context can also contribute to placebo/nocebo effects, and probably contributes to the relative discomfort of the nasal swab experience as well. I wonder if it is more distressing to walk up/be in a clinic as compared to a familiar, comfortable context, e.g., your own car in the drive-up test? Maybe differences in prior experience and context of the test partly contribute to why the nasal swab feels so different for individuals. Another way testing could be made less distressing is by performing the swab on oneself, as NPR reported back in May. This would be a boon for medical workers, lowering their potential exposure to the virus, and perhaps patients as well, if it might decrease distress by allowing for increased control. While there were concerns that patient-collected samples might not be of good enough quality, a recent small study from Stanford suggests this approach can be performed reliably.
So, what can a patient do to make the COVID-19 test less distressing if one can’t control the context? Mindfulness – awareness of the present moment in a nonreactive manner – could prove helpful, as studies have suggested it can be for chronic pain. Perhaps a mindfulness meditation focused on the breath, conducted just prior to testing, could help separate the affective emotional response to the nasal swab from the sensory, reflexive experience, just as this practice can be effective in acute painful situations.
The take-home message: if you’re going to get swabbed, try to control the context as much as you reasonably can, engage in mindful breathing, and be prepared for your eyes to water. If you’ve gotten swabbed, what did you experience? And if you’ve done it on yourself, was it less distressing?
Nora McCall, PhD, postdoctoral fellow, University of Pennsylvania, US
Week 2: Monday, July 20, 2020
Defending From Home in the COVID Era
How Inflamed Brains Navigate a Maze
Sharing Is Caring: Knowledge Translation in Pain
Going in Reverse (Translation): Starting in Humans and Working Backwards
Evidence-Based Practice and Patient Beliefs: Mixing Oil and Water?
One of my dad’s favorite quotes is, “The limits of my language are the limits of my world,” from philosopher Ludwig Wittgenstein. While thoughtful and precise definitions are always in style, the importance of diction is tantamount when studying something you generally can’t poke or see. This means that, after all the experiments are done, pain research ultimately relies upon careful definitions to convey meaning. While agreeing on definitions can be challenging, this reliance upon language adds richness and humanity to our science, and allows for revision.
On the topic of revision and definitions, the two-year semantic journey of a 14-member task force formed by the president of the International Association for the Study of Pain (IASP) came to a close this past week (see article here, commentary here, and infographic here). Their mission was to use the collective knowledge of the field to update the IASP 1979 definition of pain:
“An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”
These academic and clinical experts discussed and debated amongst themselves; solicited advice from bioethicists, philosophers, and a linguistics expert; and surveyed the general public, researchers, and pain patients. After synthesizing all of this input, they produced an updated definition of pain, unanimously accepted by the IASP Council:
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”
Admittedly, this revised definition is quite similar to the old one. The phrase “resembling that associated with … tissue damage” does allow for more overt inclusion of pain occurring through neuronal adaptation but without injury, as tissue damage is certainly not a credential required for pain (see PRF related article on nociplastic pain). Unfortunately, for those hoping for a large shift in the definition, the need for a “big tent” to accommodate many aspects of pain – acute and chronic; nociceptive, neuropathic, and nociplastic; human and nonhuman – ultimately won out over major revisions.
However, while the 2020 “concise and precise” definition of pain bears remarkable homology to that of 1979, the real substance of the task force’s update is reflected in the accompanying notes, which, to borrow from Haruki Murakami’s memoir, speak to what we talk about when we talk about pain. Here, the task force centers the experience and authority of the individual in pain rather than the observer. Indeed, the experience of pain is in the first person, and the experience of pain is diverse. The notes further clarify that nociception –activity in the nervous system in response to a noxious stimulus – and pain are not synonymous. At the suggestion of the consulting philosophers, the notes emphasize that pain does not require verbal description to be valid. This is especially important when considering the validity of pain in non-verbal human patients, such as neonates, and is important for preclinical researchers like myself.
A question I’m still chewing on is whether this revised definition should have explicitly mentioned the cognitive facet of pain. While the task force considered including cognitive factors in their notes, they ultimately decided this was implied by the description of pain as a personal, subjective experience. The ability of pain to demand and hold one’s attention is a critical facet that deserves to be acknowledged separately, as it might be treated separately. Indeed, the term “pain catastrophizing,” used to describe an overwhelming focus on chronic pain, highlights the negative impact that this focus on pain has on quality of life. While this term is not perfect – I think it focuses on the perspective of the observer rather than the individual experiencing pain – it does highlight similarities between maladaptive pain and negative affective disorders. In these disorders, as in chronic pain, negative repetitive thoughts about the self impair one’s ability to accomplish daily tasks. Perhaps including the cognitive aspect of pain in the official definition would allow for parallels and treatments to be drawn from other aspects of neuroscience.
While the 2020 definition did not substantially change, the discussion surrounding the revision highlights the depth and breadth of the field of pain research. Looking ahead, it’s important to consider the purpose we want the definition of pain to serve. Should we continue to think broadly, or should we get into the weeds and highlight more details that so many researchers have worked to uncover and understand?
P.S. Stanford is leading the charge to update the term pain catastrophizing! If you are also interested in semantics and pain, you can weigh in here.
Nora McCall, PhD, postdoctoral fellow, University of Pennsylvania, US
Mine is a study by Dr. Lauren Orefice from Dr. David Ginty’s group suggesting that some core symptoms of autism might originate from abnormal function of the peripheral nervous system ("head explodes"). This was huge, as the majority of preclinical autism research has always focused on the brain, and the majority of research on the peripheral nervous system focuses on understanding sensory perception. This paper, therefore, combined my two research interests (social/anxiety-related behavior and sensory perception) in a way I hadn’t seen before, and guided the development of my own thesis project. I revisited this paper recently and wondered whether everyone had a favorite paper. I asked a few friends and received a chorus of yeses, but what is more interesting is the variety of reasons:
Reason 1: “It didn’t need any gimmicks or fancy techniques to tell a good story. It was well written and the data spoke for itself.”
Rigorous, reproducible, and cohesive work is more or less what we’re all aiming for. To move any field forward, we need to employ unbiased and thorough experimental design and analysis. However, I often feel that the use of a new technique is more exciting than the finding it was used to uncover. When designing projects, are you leading with a newly available technique or leading with a scientific question? Is each approach equally valid?
Reason 2: “It asks a philosophical question about a major foundation of logic in a lot of systems neuroscience and levels a critique right at it.”
I find that the science community tends to find less value in controversy. In fact, it can be difficult to publish data that contradicts prior work from a more famous lab. But is it the best practice to automatically trust the data from a lab with a strong record? As there isn’t much space to publish negative data, what happens when no one can replicate those findings?
Reason 3: “It combines all of my interests into one paper. Like, ‘I’m not the only one who’s thought of combining these ideas?’”
It’s often the bold and creative, high-risk, high-reward work that excites both researchers and the general public and leads to medical breakthroughs, but are the processes for obtaining research grants too risk-averse to allow more researchers to engage in this type of work?
In a Venn diagram of these three reasons, where does your favorite paper fall? Where does your research fall?
Melanie Schaffler, PhD student, University of Pennsylvania, US
Defending From Home in the COVID Era

Imagine you’ve worked for three-and-a-half years straight planning studies, piloting methods, recruiting participants, collecting and analysing data, writing articles, battling reviewers … and finally it’s your time to shine! Then, two weeks before the big day, the entire country (if not world) goes into COVID-19 lockdown, and your supervisor tells you to just “wait and see what happens.”
A month passes, and the world is definitely still closed for business. Technology is not your strong suit, but you decide you really want to “get it over with” while everything is still fresh in your mind so you can close this chapter. After all, you’ve already been hired to work on a new project.
Just a few short weeks after applying for an online PhD defense, the big day rolls around again. Except it’s not quite the day you’d hoped for. Sure, you’re still nervous, you’ve still styled your hair and put on a nice shirt … but … you’re also in a pair of track pants, in your living room, staring into a screen showing nothing but your own slides and a list of your audiences’ initials.
This was the story of Line Bay Sørensen, a then-PhD student, now a postdoc at Aalborg University, Denmark, though her story is surely not unique. Online PhD defenses (although not new) have increasingly become the “norm” out of necessity in the COVID era. They get the job done, but they’re not quite the same as an in-person defense. You miss the pep talks from your supervisors, the reassuring nods from your colleagues, and the informal chatter and handshakes with the opponents, not to mention the immediate technical support available when your slideshow decides not to play.
Mind you, when Line and I sat down to chat about her experience, we concluded that it wasn’t all bad. Beyond the economic and environmental savings of not flying opponents in from all parts of the globe, the online experience also allows more friends and colleagues to attend. No matter if people are on parental leave, living abroad, or just stuck at home waiting for a delivery: Anyone can make it from anywhere. That also means other researchers or clinicians from anywhere in the world can attend, just out of interest – something that would rarely happen otherwise.
So should we actually be exploiting modern technology more? Perhaps. It would be a shame to lose the energy of the in-person defense by going virtual for good, but why not get the best of both worlds and have a “hybrid” defense – it already sounds like the way of the future!
Megan McPhee Christensen, PhD Student, Aalborg University, Denmark
How Inflamed Brains Navigate a Maze
A rat finds itself in a dark octagonal chamber. Each of the chamber’s eight walls has an aperture that opens into a straight corridor. This is the 20th day in a row that the rat has found itself here, so the animal goes about its business. Efficient and assured, the rat runs down, one by one, four of the eight corridors, eating the sugar pellet reward at the end that hasn’t changed position for weeks.
A different rat finds itself in the same octagonal chamber. This rat occasionally pokes its snout into a sugar-baited aperture, sniffs around, maybe even stretches itself out halfway through … and then decides against entering. The rat spends most of the five minutes it’s in this maze in the octagonal chamber. Three weeks ago, the animal was efficiently seeking out the sugar reward it knows is still there to take. Now, like about a third of its cohort, the rat is no longer interested.
Both rats have undergone chronic constriction injury of the sciatic nerve – a common model of neuropathic pain – yet they behave very differently. The second rat isn’t in more pain – a von Frey test shows that it has the same hind paw withdrawal threshold. Nor has the second rat forgotten where the sugar pellets are – it makes roughly the same number of memory errors as the first rat.
So what’s the difference between the two rats? What makes one continue to be motivated to seek out a sugar reward while the other loses interest?
The idea that pain lowers mood seems perfectly obvious – pain makes for a deeply unpleasant experience, after all. Few people are surprised to hear that about half of people living with chronic pain also experience depression, anxiety, or both, alarming as the proportion may be.
But let’s flip this around for a moment. Why doesn’t every person with chronic pain experience depression? Surely if two people experience comparable long-term, debilitating pain, they would report a similar amount of mental distress. Not necessarily. The relationship between intensity of pain and depressive symptoms is not strong. The key to answering this question may instead lie in understanding the difference between the two rats mentioned above.
The difference, it seems, is inflammation in the brain. The second rat – which loses motivation following injury – has increased microglial activation and cytokine expression in distinct brain regions, such as the ventral hippocampus and medial prefrontal cortex. These are regions associated with motivated behaviors.
Individual differences in the spread of inflammation from the periphery to the brain may therefore explain why only some chronic pain patients experience depression.
Pending access to the lab post-lockdown, I’ll be working to shed more light on what these individual differences may be.
Jayden O’Brien, PhD student, University of Sydney, Australia
Sharing Is Caring: Knowledge Translation in Pain
Ask any child about to get a needle if they wished it would be painless. It is highly likely that the response would be a resounding “yes.” In fact, ask anyone who has experienced pain, and, chances are, they would want to know more about how to manage pain and learn more about it in general. There is a great deal known about pain, and this knowledge is routinely disseminated amongst the wider academic community through mediums such as academic articles and conference presentations. Dissemination is key in order to share advances in the field and expand knowledge. However, does our conceptualization of dissemination have too narrow a scope if it is predominantly limited to academic audiences?
Consider whom pain affects (e.g., the child about to get a needle) and to whom evidence is usually disseminated (e.g., researchers). Perhaps you, too, have identified the incongruence in this example. The evidence available on how to manage pain may never reach the individual who may benefit from it. This is problematic and raises this question: Are we doing enough to disseminate knowledge, beyond our traditional circles, with those who can benefit in the public as well?
Knowledge translation (KT, sometimes referred to as knowledge exchange, mobilization, or transfer) is a process to close the gap between researchers and individuals who can benefit from knowledge (i.e., knowledge users) through accessible dissemination of information that is simple to understand. These processes are critical to ensuring knowledge gained from research is relevant to actual patient needs and concerns. The specific objectives of KT may include an integrated approach where knowledge users work collaboratively with researchers, such as on developing pain research questions together, as well as end-of-project KT, such as the creation of plain language pain management resources.
KT is one way to expand the scope of dissemination in the field of pain. By sharing information that is accessible about pain, easy to understand, and relevant, we may engage broader audiences in pain research and improve pain management – an especially important goal given the prevalence of pain. KT could potentially also promote public engagement with research, thus creating opportunities for more impactful research through the inclusion of diverse knowledge user perspectives. As dissemination plans become increasingly common aspects of research projects, it will be exciting to see the innovative ways our field can share knowledge about pain with those whom the research concerns.
Nicole MacKenzie, PhD student, Dalhousie University, Halifax, Canada
Going in Reverse (Translation): Starting in Humans and Working Backwards
I am fortunate as a young researcher to be part of Northwestern’s Center for Translational Pain Research, which is a multi-lab endeavor to bridge from the most basic molecular science all the way to clinical trials in humans. Anecdotally, it is also one of the warmest and most collaborative environments I have experienced.
At the annual review this week, I signed on to the all-day Zoom early and was delighted to experience that pre-talk phenomenon of several established principal investigators casually joking amongst themselves and discussing each other’s research. One comment stood out to me in particular, which I will paraphrase as, “If you want to find a new drug for pain, you have to start in humans and work backwards. No pain pharmacology was ever discovered in animals first.”
This comment came from an eminent pharmacologist and was directed at an equally eminent neurobiologist. All laughed, but it struck at the core of something I consider frequently in medical training.
In medical school, I was implicitly taught that we determine the root cause of disease and then design treatment around that cause. I say “implicitly” because it is actually quite common that the discovery went the other way around: A treatment worked and then we determined what it did, thus establishing the root cause of disease. Certainly in the fields of neurology, psychiatry, and pain, this was frequently the true progression: Treatment came first, and then the understanding of the pathophysiology based on the biochemistry of the treatment.
With this in mind I wondered, What are we doing looking for new pharmacological targets in mice? What are we doing looking for biomarkers of pain in model organisms? It reminded me of my early work in a cancer lab, when a mentor told me, “The good news is, mouse cancer is cured. The trick is making it work in humans.” That “trick” prevents greater than 90% of new drugs from passing FDA clinical trials, an enormously inefficient progression.
My own work is focused primarily on circuitry changes in the contexts of chronic pain and chronic opioid use. Within my center, the general hypothesis about which circuitry is important bounced from rats to humans and now back to mouse genetics. Perhaps this same principle of taking what is known in humans and reapplying it to a system in which we can actually study biochemistry of function could increase the chances of truly translational findings.
I hope this post serves as a reminder that even the most basic science, in order to successfully translate to humans, can use a lift from the messy and incidental world of human data. To my knowledge, no one has set out to cure mouse cancer, and I certainly did not set out to treat mouse pain (apologies to my wonderful model organisms). I know this has reinvigorated my own dedication to sometimes wander out of my subfield and into the confound-ridden world of medical literature. After all, bringing the two together is the ultimate goal.
Sage Morison, MD/PhD student, Northwestern University, US
Evidence-Based Practice and Patient Beliefs: Mixing Oil and Water?
Researchers in the field of persistent pain conditions continue to make significant gains in helping those with these challenging diagnoses. Persistent pain presents unique challenges for clinicians as each patient often does not fit into a standardized approach. An emphasis has been placed on being less prescriptive with our treatments and individualizing our care to treat the “whole person.”
So where does a patient’s belief system come into play under the scenario where a patient’s perspective does not match ours regarding what is going to help their symptoms? As healthcare professionals and researchers, do we set aside our training and knowledge that we have spent years on in favor of something that our patient tells us? Furthermore, as clinicians, if we provide this intervention, how comfortable do we feel with billing and documenting for reimbursement?
While practicing as a new clinician, I would run into situations where a patient would communicate their perspective on what they needed to improve. At times, this would not match practice guidelines that guide evidence-based care. In discussing this with a clinical mentor, she told me that providing an intervention that has no evidence of effectiveness is like “the pickle.” She went on to tell the story of a restaurant that provided a free pickle spear with each customer’s dish. Eventually, the restaurant stopped providing this free pickle to save money, as it realized most patrons simply tossed away the pickle. Ultimately, the restaurant received backlash and had to change its policy. Is this story true? Who knows? Does this principle relate more to customer service? Most likely. But the moral of the story was that people often find value in things that we may not deem necessary or effective.
So what do we do the next time a patient comes into the clinic or lab and expresses a belief regarding their own care that is completely against evidence-based practice? Do we go on a mission to prove them wrong? Or do we listen to them and proceed forward with their preference? Perhaps the answer is somewhere in the middle. Given that each individual’s pain experience is unique to them, approaching the person sitting in front of us and listening to their story may be the first step in improving this mixture of oil and water.
Andrew Post, PhD student, University of Iowa, US
I’m sure many of us will relate to this experience: You go to a restaurant, you are warned against a dish (“Are you sure you want to have that? It really is quite spicy!”), you ignore the warning, and you deeply regret your decision. It turns out the dish really was quite spicy; you now feel as though your mouth is on fire.
What’s the science behind this? Why does spicy food feel hot?
The answer is simple: capsaicin. Capsaicin is a chemical that can be found in some foods like chili peppers. It causes a burning sensation because it tricks our brain into thinking we are being exposed to hot temperatures. To understand how this happens, we first need to understand how “painful heat” is perceived as such.
Pain perception is a complex topic, still under debate – heated debate. But there are some key players nearly everyone agrees on: ion channels. Ion channels are proteins that are present on the membrane of some cells, including neurons. Most ion channels are closed until being activated (opened) by something. Once open, they allow ions to go into the neuron, which may activate it. If so, this neuron can then pass the signal on to other neurons.
Importantly, different types of ion channels are opened differently, and each neuron only has some types of ion channels. This means that, roughly speaking, the specific combination of neurons activated by a certain stimulus “tells” the brain what the stimulus was. For example, TRPV1 is an ion channel that is sensitive to extreme heat. In the presence of very high temperatures (above about 42°C in mice), TRPV1 channels open, and the specific sensory neurons that have TRPV1 channels are activated. This signal may then be passed on to other neurons and all the way up to the brain. When it gets there, you perceive that you are being exposed to something extremely hot.
How does this relate to capsaicin? Interestingly, heat is not the only thing that can open TRPV1 channels – capsaicin can do it, too! So when capsaicin is present (e.g., when you eat chili peppers), similar mechanisms are at play as they would be for extreme heat: The same TRPV1 channels will open, those same neurons will be activated, and the signal will be transmitted to the brain. Essentially, because the same neurons are activated as when you are actually being exposed to hot temperatures, you will perceive capsaicin as extreme heat.
This is why chili peppers burn!
Elisa Clemente, PhD student, University College London, UK
Week 1: Monday, July 13, 2020
Curiosity Killed the Clinician and Created the Scientist (in Me)
A Passion for Children’s Health, Pain Management, and Communication
A Biopsychosocial Educational Approach
Researching the Emotional Aspects of Chronic Pain
I've lost count of the number of times I've been asked this question during my PhD. Depending on my mood and the audience, my reply usually varies between jokingly pointing out “I sure hope they do ─otherwise my PhD will have been for nothing!” accompanied by a creepy laugh, and the more serious answer: "We can't know for sure, but they have many of the anatomical features required for pain in humans and other mammals." (To clarify, I’m not a monster – I normally reserve the former reply for close friends and family). Funnily enough, this is the very question I've set out to answer during my PhD. Or rather, a variation of that: “Can we establish zebrafish as an animal model for pain?”
I started my PhD at University College London (UCL) in 2017 as part of the London Interdisciplinary Doctoral programme (LIDo-DTP). I chose this project because I was particularly drawn both to its cellular/molecular approach to a translational topic, and to the topic itself: pain.
It is hard to state my deep interest in pain without sounding even creepier than in the first paragraph of this text. But pain really is incredibly interesting! Think about it. Almost every single person in the world experiences physical pain at some point in their lives. And yet, no one knows exactly what someone else’s pain actually feels like. It’s in the very nature of pain to be a subjective experience. At the same time, there is also something very universal to it: all complex animals do their very best to avoid the unpleasant experience of pain. It acts as a warning sign, being critical for survival. Nevertheless, pain can also become maladaptive and a source of great distress for the millions of people worldwide who suffer from chronic pain.
This duality between its uniqueness and universality, and how something crucial for survival can become so damaging, makes pain something really interesting to study. On top of that, even the smallest discovery regarding this highly complex phenomenon has the potential to positively impact someone’s life. Therefore, this can also be a very rewarding endeavor.
For the last couple of decades, zebrafish have been increasingly used as an animal model in neuroscience. As relatively simple and well-characterized vertebrates, they often strike the perfect balance between simplicity and complexity to address a number of questions. However, zebrafish have been a late arrival to the pain field. Consequently, we still require a better understanding of its potential and limitations as a model of pain.
So I guess, after all, I do need to work out if “fish even feel pain.”
Elisa Clemente, PhD student, University College London, UK
Recently I find myself wondering what it would be like to just be a graduate student. While not a very productive thought exercise, I sometimes think about how my life would be and how my future would look if all I had to worry about were my experiments, presentations, coursework, career goals, grant applications, committee meetings, teaching, etc. Instead, I also have to worry about how sexism and racism affect how I am perceived while executing these already challenging tasks.
I am a PhD student in the Neuroscience Graduate Group at the University of Pennsylvania studying the role of mechanosensory neurons in stress resilience. I discovered neuroscience as an undergraduate at Wesleyan University and have been pursuing questions of the brain and behavior ever since. However, to be engaged in academic pursuits means to also be plighted by the flawed and structurally biased American academic system. People will always say “just focus on the science,” but I am aware (and have been told directly) that my science is viewed differently.
For example, every time I apply/compete for something, and whether I get it or not I think, “if I get this [award, position, opportunity] people are going to say I only got it because I’m Black.” Follow-ups include: “If I ask a dumb question in class or in a talk, this will confirm everyone’s suspicions” and if it’s a diversity award, “everyone will assume it’s less competitive.”
I am working on not letting these things bother me. I am also working on being a better scientist, exploring my interests in writing and science communication (thank you PRF Correspondents Program), and advocating for issues I care about. I’m finding ways to push back and give my anger and frustration a positive outlet.
Melanie Schaffler, PhD student, University of Pennsylvania, US
Curiosity Killed the Clinician and Created the Scientist (in Me)
Curiosity has a lot to answer for. To be curious is to be eager to learn something unknown, regardless of whether what a person learns is ultimately favorable or not. Come to think of it, curiosity is perhaps the perfect scientific motive, albeit unlikely to bring home much funding.
I like to think I have always been curious. I want to understand what is going on, even if I can’t “fix it.” I think that’s why, when I started seeing patients with complex persistent pain as a new graduate physiotherapist, I got frustrated. Of course, I didn’t expect to be able to help everyone, but I did expect to be able to identify the source of the problem. Unfortunately, pain is not always like that (as you surely well know).
To try and make some sense of it, I went on a little Euro-trip to listen to the world’s leading experts speak at the European Pain Federation (EFIC) congress. Who knew? Turns out there were thousands of other people puzzled by pain just like me, and they were trying to learn more! Unfortunately, they didn’t have all of the answers either. In fact, even after then taking a masters in pain management, I had learned a lot about pain, but still had many unanswered questions. It was time to take the PhD plunge and find out just how many unanswered questions there really are!
That brings me to now – Hi! I’m Megan, an Aussie physio currently finalizing my PhD at the Center for Neuroplasticity and Pain (CNAP) at Aalborg University in Denmark. So far, I’ve been focused on understanding sensitization in patients with low back pain, and now I’m learning to communicate as a PRF correspondent, but who knows where curiosity will take me next.
Megan McPhee Christensen, PhD student, Aalborg University, Denmark
Hi! It’s Jayden here, corresponding from Sydney, Australia. I’m a PhD candidate in the Laboratory of Neuroimmunology and Behavior at the University of Sydney, where I’m researching the role of neuroinflammation in preclinical and clinical chronic pain states. I’m particularly interested in how inflammation in distinct brain regions in neuropathic pain conditions is linked to depression and anxiety so commonly experienced by pain patients.
I’m very excited to be a part of the Correspondents program and improve my skills in communicating pain science to a range of audiences. The importance of quality science communication cannot be understated – it deeply affects how everyone values and engages with not just scientific information, but expertise more generally.
The ability of experts to communicate scientific information with clarity and inclusivity is more important than ever in public discourse. I’m continuing to ride the learning curve in this area, but I’m hoping to contribute something worthwhile for researchers, clinicians, and patients alike over the next several weeks.
I’m very keen to share with you some key areas of interest I’m working on, the thoughts and opinions that cross my mind, and my experiences in pain research and communication more generally. I’m sure there will be some reflections on graduate study in a COVID-19 world at some point, too. Stay tuned for some content I’m developing on topics and issues that don’t always get the spotlight in pain research. I’m excited to share these with you.
Jayden O’Brien, PhD student, University of Sydney, Australia
A Passion for Children’s Health, Pain Management, and Communication
Hello, PRF readers! I am Nicole MacKenzie, a clinical psychology PhD student at Dalhousie University, and I am thrilled to be part of the PRF Correspondents Program. I have long had interests in childhood development and health, and my interest in these areas developed from volunteering and working at a large pediatric hospital in Toronto. Through working with families in various clinics and settings, and having seen pain faced routinely by children, the importance of managing pain and empowering families to be in control of pain management became very clear to me.
My passion for children’s health, pain management, and communication led me to move from Toronto, where I studied early childhood development and developmental psychology, to Halifax, on Canada’s east coast. I made this move to study at Dalhousie University to pursue research in pediatric pain and knowledge translation, especially as it relates to procedure pain.
In my work thus far, I have reflected on what role researchers and health care providers can play in making pain management more accessible to patients and their families. Through my research in Dr. Christine Chambers’ lab, I have begun looking for the answers to some of those questions pertaining to what makes research accessible to families, as well as what promotes the uptake of evidence-based practices for pain management. My research has focused on knowledge translation, or the exchange of information between researchers and knowledge users, in the context of improving use of pain management strategies, specifically during children’s vaccinations.
Through my research, I have developed a passion for science communication, not only with researchers and healthcare providers, but with the public as well. It is rare for research to be shared directly with the public, especially in terms that are easily understood, and science seems to be increasingly called into question in public forums.
The importance of science communication is therefore more important than ever. I believe it is key not only to engage all individuals who can benefit from research findings, but also to inspire interest and support for science by the public as well. Since pain is an issue that affects people from all walks of life, it is of particular importance that we engage in open communication in this field to promote better pain management. This is an issue I look forward to discussing further in my time here as a PRF Correspondent and beyond.
Nicole MacKenzie, PhD student, Dalhousie University, Halifax, Canada
A Biopsychosocial Educational Approach
I am a second-year PhD student at the University of Iowa, where Dr. Ruth Chimenti, PhD, is serving as my advisor. I am a physical therapist and completed my DPT degree from Grand Valley State University; then I practiced full-time for six years. During my time in the clinic I worked with a persistent pain population and developed a greater appreciation of the complexity of pain. This appreciation generated my desire to delve deeper into pain research and ultimately led me to Iowa City.
Currently, in our lab we are looking at the effects of a biopsychosocial educational approach for patients with persistent Achilles tendinopathy in combination with a progressive tendon loading exercise program. We are interested in how addressing psychological-related factors such as kinesiophobia and pain catastrophizing in this patient population may improve movement-pain and function. We are also exploring how the central nervous system may be involved with the modulation of persistent and recurrent Achilles tendon pain. Additionally, with Dr. Kathleen Sluka, I am working on a multi-site, pragmatic trial that aims to explore the impact of Transcutaneous Electrical Nerve Stimulation (TENS) on movement-evoked pain in individuals with fibromyalgia.
I am excited to have the opportunity to serve as a PRF Virtual Correspondent. One of my career goals is to improve the translation of research into clinical practice and to provide patients who suffer from chronic pain greater access to resources to enhance their understanding of their symptoms. Through my clinical practice, I found that greater awareness by both clinicians and patients of non-invasive treatment mechanisms and of physiology of pain assisted with improved outcomes. I am excited and grateful for the platform provided by IASP as a PRF Virtual Correspondent to reach a broad audience to communicate with pain researchers, clinicians, and patients who suffer from persistent pain.
Andrew Post, PhD student, University of Iowa, US
Five years ago in an undergraduate general neuroscience class on touch senses, a question occurred to me that will likely drive my whole career: why do we classify pain as a sense? Turning to the textbooks and literature, I essentially found that the answer was: because we feel it. Thus began my fascination and obsession with understanding pain as an unexplored window into perception.
This fascination dovetailed with my desire to be a doctor. The more I understood pain as an experience and not simply a sensation, the less I understood the medical approach to pain. When I started to learn about chronic pain, I knew I had found my niche. I would be one bridge between the latest neuroscience on pain processing and medical treatment.
I work in a systems and molecular neuroscience wet lab whose specialty is dopamine neuron subtypes. I describe my research as using complex mouse genetics to make specific neurons glow under exact conditions. My lab is a strong basic science lab, fascinated with knowledge for knowledge’s sake. So what is a practical, medical person doing there?
I have a firm belief that you cannot design a new treatment if you don’t know what you’re treating. The broad medical understanding of pain as a simple sense to be dulled, as with anesthesia during surgery, has hampered our ability to combat more complex or emotional components of pain. So, during my PhD and research career I hope to contribute to this most basic knowledge by asking the most basic questions. Once more is known about what exactly pain processing consists of, treatment design can be sharper and, crucially, more efficacious.
It is from this perspective that I will write these blog posts, and I am so excited to be a part of this community working at all levels to enhance pain care and heal people.
Sage Morison, MD/PhD student, Northwestern University, US
Researching the Emotional Aspects of Chronic Pain
Greetings PRF community! I’m Nora, a postdoctoral fellow living in Philadelphia, Pennsylvania. I first got into neuroscience as an undergraduate during a month-long research experience, after which I took my first neuroscience class – and the rest is history! The throughline of my research career has been to understand how experience can change the brain and behavior, and how the brain influences our perception of experience. I have studied how nutrition, stress, and drug exposure can influence mental health and addiction-like behaviors in rodent models, and now my work focuses on the emotional and cognitive facets of chronic pain.
I have worked in the laboratory of Gregory Corder at the University of Pennsylvania for about a year since receiving my PhD from the University of Minnesota in 2019, and this is my first time in the pain field. The goal of my research is to identify cortical brain circuits responsible for the emotional symptoms of chronic pain in preclinical models. The emotional aspect, or “affect” in rodents, of chronic pain is a significant source of suffering for patients. Interestingly, the current standard of care – opioid analgesics –removes attention to this symptom, i.e., “it hurts, but who cares?” Furthermore, this experience aligns with that of patients whose intractable pain was treated with cingulotomy, the lesion of a brain region implicated in affect and attention, including the anterior cingulate cortex or the cingulum bundle. Following surgery, patients could perceive the sensation of pain, but no longer found it bothersome. The removal of the negative emotional aspect of pain and the attention it draws, but the preservation of the adaptive ability to respond to acute harmful stimuli, represents a potential approach to chronic pain treatment.
My research seeks to understand the mechanisms at play with opioid and cingulotomy analgesia. I accomplish this by providing insight into cortical circuits that underlie chronic pain-induced affective-attentional rodent behaviors. In particular, I’m focused on understanding how anterior cingulate neurons activated by noxious experience could be modulated by endogenous opioids. I take full advantage of using a model system to answer my research question: I look at microcircuits of the cortex with slice electrophysiology, modulate genetically-defined circuits and neuronal populations during behavior, and use in vivo imaging to assess neuronal activity while subjects respond to noxious stimuli. My ultimate goal is to improve our understanding of chronic pain to improve treatment.
I’m interested in how emotion and pain perception impact each other, how pain and pleasure overlap, and how social constructs can impact pain treatment in the clinic. As a preclinical researcher, my focus on mechanisms and circuits inadvertently blinds me to real issues at the clinical level that might make my work less relevant, e.g., disparities in the perception of a patient’s pain and their treatment, driven by race or class. I want to better understand the complex clinical context in which findings like mine might ultimately be used.
I’m excited to use this platform with PRF to learn more about the newish-to-me pain field while improving my science communication. My biggest science communication “sin” is using jargon. I hope that over the course of this experience, my writing becomes more “human” again. See you next week!
Nora McCall, PhD, postdoctoral fellow, University of Pennsylvania, US