Recommendations by the International Association for the Study of Pain
Executive Summary
The International Association for the Study of Pain (IASP) supports the development of policies that ensure implementation of advances in both the science and delivery of health care for people in pain. It is concerned that, considering the burden of pain, transfer of knowledge is not happening at an appropriate pace. IASP has therefore developed guidance for members, government and nongovernmental organizations working in both developed and developing nations who seek to improve pain care.
IASP recommends strategies that address barriers to progress based on an analysis of submissions from 19 member countries and on feedback from IASP chapters.
The process was overseen by a working party drawn from both developed and developing nations. The document should be read in conjunction with the Declaration of Montréal asserting that access to pain management is a fundamental human right.
Key recommendations are:
- Access to pain education for health professionals and the general population
- Coordination of the care system to ensure timely access to the right support
- A quality improvement program to address access and standards of care
- A reasonable proportion of direct and dedicated funding for pain research
Critical factors for success are:
- Gathering of evidence on the burden of pain to the nation
- Gathering of information on access to care
- Development of government policy on pain services
- Formation of a broad coalition of stakeholders
- A clear plan with timescales to achieve strategic actions
Working Party:
- Michael Cousins, Chair (Australia)
- Harald Breivik (Norway)
- Mary Cardosa (Malaysia)
- Jim Cleary (USA)
- Beverly Collett (UK)
- Liliana De Lima (USA)
- Rollin M. Gallagher (USA)
- Maija Häänpää (Finland)
- Amira Karkin-Tais (Bosnia and Herzegovina)
- Philipp M. Lippe (USA)
- Diederik Lohman (USA)
- Henry Lu (Philippines)
- Mary Lynch (Canada)
- John Ney (USA)
- Germán Ochoa (Colombia)
- Cathy Price (UK)
- M. R. Rajagopal (India)
- Olaitan Soyannwo (Nigeria)
Background
The International Association for the Study of Pain was established in 1973 in response to the recognition that pain should be better managed. In the time since IASP’s inception, remarkable advances have occurred in terms of understanding the epidemiology, causes, and treatment of both short-term and persistent pain. Pain has many facets, including its causes, chronicity, location, and qualities.
Concern that scientific advances are not being matched by better treatment has prompted a series of declarations and actions by national and international bodies advocating better pain control (Appendix 1). These calls to action are based on three suppositions:
- Pain, no matter what type, is inadequately treated due to a variety of cultural, attitudinal, educational, political, religious, economic, and logistical barriers.
- Inadequately treated pain has major physiological, psychological, economic, and social consequences for patients, their families, and society.
- All developed and many developing countries are capable of significant improvement in the treatment of pain.
The International Association for the Study of Pain (IASP) supports the view that every nation should have policies on the management of pain that describe the burden of pain, its impact, and what should be done in terms of policy interventions to reduce these problems. This paper sets out recommendations for the core elements of any national pain strategy. It accompanies the Declaration of Montréal, which asserts the human rights of those in pain. It is intended that this guidance should act as an impetus to clinicians, educators, administrators, and governmental or professional organizations involved in the establishment and maintenance of standards for pain services to take steps to prevent the continued suffering of millions of people and avoid any waste of resources. Patients, their families and others affected by the undertreatment of pain must be welcomed into this process as active participants.
Scientific Advances
Major breakthroughs in our understanding of pain have occurred as a result of advances in the neurobiological, epidemiological, and psychological factors that give rise to high levels of pain. Imaging studies have shown that persistent pain is associated with significant functional, structural, and chemical changes in the brain [28,32]. The exact implications of these data are as yet unknown, but distinct changes have been observed. Patients who have chronic pain disorders with known causes (e.g., osteoarthritis or nerve damage) or unknown causes (e.g., nonspecific low back pain) may have altered cerebral pain processing and loss of gray matter, leading to impaired function [1,27,35,42].
Epidemiological advances in chronic pain include better characterization of the population and longitudinal surveys. The prevalence and impact of chronic pain appear remarkably similar, no matter where in the world they are measured [4,8,10,14,17,20,25,29,30].
Key common findings include:
- One in five people of all ages have moderate to severe chronic pain.
- One-third of individuals of working age who have chronic pain have lost the ability to perform wage-earning or other work.
Worldwide, if we continue to fail at effective pain management, we will continue to pay a staggering and unnecessary price [12].
Treatment Advances
Advances in interdisciplinary care have led to improved understanding of how to better manage pain, yet studies have consistently demonstrated the undertreatment of pain. This problem includes inadequate treatment of cancer, postoperative, post-trauma, and chronic pain. A review of published literature has identified that nearly half of people with cancer pain are undertreated [9,15], with similar rates of undertreatment in postoperative pain, even in developed countries [18,39]. Access to timely and appropriate treatment for chronic pain is an international problem [21]. Poor access to care can lead to deterioration in health [21,22,23,36], risking aggravation of the pain condition and further decreases in quality of life, resulting in more expensive interventions being necessary.
Guidelines on cost-effective interventions for the management of pain have been published. Summarizing the literature [6,16,19,26,37,43], we now know that medical interventions aimed at the purported underlying cause of pain may prove to be costly. For those with chronic pain, active self-management strategies are “associated with lower levels of pain-related disability and health care” use (5). Training is often needed in this area for both health care professionals and people in pain, because knowledge is frequently not applied.
The International Association for the Study of Pain has sought to understand why there is a failure in knowledge transfer.
International Strategy Development
IASP invited member chapters to submit any examples of programs in which there had been an attempt to identify and address underlying reasons behind the failure in knowledge transfer.
Nineteen countries submitted health policies on pain for review by a working party. Chapter presidents were surveyed as to their opinion on barriers to effective pain management. Seven countries were found to have a comprehensive strategy to address the management of pain; the remainder had strategies focusing mainly on opioid control. These are contained within Appendices 1 and 2. These findings were reviewed by a working party drawn from 15 nations; barriers and potential solutions were proposed by the group. All chapter presidents together with health policy makers were invited to the international pain summit hosted by IASP.
Throughout this process IASP, highlighted common professional, public, and system barriers to implementation of better pain care:
- Pain measurement is neglected.
- Professionals caring for people in pain often lack the knowledge and skills to manage pain. As a result, attitudes are more often shaped by a variety of beliefs based upon experience and culture than by knowledge. National surveys in Canada and the United Kingdom have identified that veterinary schools have been able to integrate knowledge about pain into their curricula, while medical schools have lagged behind [13,38].
- Resource allocation within the health care system may be overly directed toward trying to treat the underlying cause rather than the pain per se. Financial payment that promotes activity rather than self-care is an example.
- Coordination between health and social care systems is poor. There may be a lack of resources and of clear models of care to ensure coordination of pain management between the various primary and secondary care and health care services and social services [26].
- Research funding: pain research is grossly underfunded, considering the burden of illness [7,24].
- Supply of medicines: there is a relative undersupply of low-cost, effective medications in resource-limited settings and developing countries.
- Population-based surveys on pain are rarely done outside specific research programs. Thus, there is a lack of public health focus on pain as a priority [14].
Based on the consultation and analysis performed, IASP recommends that any strategy should consider four broad areas:
- Pain Education
- Patient Access and Care Coordination
- Monitoring and Quality Improvement
- Pain Research
These areas can be broken down to specific policy development areas:
A. Education for Both Health Care Professionals and the Public in:
- Basic science of pain
- Assessment of the needs of a person in pain
- Best practice in the management of pain
B. Models of Care:
- Biopsychosocial
- Multidisciplinary in focus
- Timely
- Have an emphasis on self-care
- Have provision for special populations e.g., learning difficulties, dementia
- Involve family and caregivers
C: Quality Standards to Include:
- Access times
- Feedback from the patient
- Measurement of quality of life
- Measurement of the economic burden of pain
D: Research to Cover:
- Epidemiology
- Implementation science, especially in the area of knowledge transfer.
Further details are in Appendix 3.
IASP also found that some key actions seem to enable development of health care policy and strategy. IASP therefore recommends:
A. Gathering of Evidence on the Burden of Pain to the Nation
Given that persistent pain is often initially associated with other disease processes, pain is often inadequately recorded both in clinical records and in the administrative coding that is often used as a source for epidemiological studies.
In Australia, the economic burden of disease was estimated through the calculation of Disability Adjusted Life Years from epidemiological data on chronic pain [2].
Nations should carry out a basic health survey that asks questions specifically about pain, its management, and its impact. The data can serve as a useful baseline from which to measure the impact of any interventions introduced [17]. This information can then inform a plan to deliver change [14].
B. Gathering of Information on Access to Care
The recent IASP task force on waiting times has allowed a clear consensus to develop on standards for appropriate waiting times. The National Pain Audit in the United Kingdom is currently measuring this with English and Welsh government sponsorship.
C. Development of Government Policy on Pain Services
Goals for improvement, as laid out above, are agreed by a wide range of stakeholders including central government and prioritized appropriately. It is noted that the impetus for this effort in two nations has occurred through the holding of the United States and Australian Pain Summits, respectively.
D. Formation of a Broad Coalition of Stakeholders
Examples of this are the UK Chronic Pain Policy Coalition, Pain Australia, and the European Federation of IASP Chapters (EFIC).
E. Realistic Timelines are Established for Achieving Incremental Change
The impact of such change should be measured in terms of both process and outcome. Population outcome data together with process measurements need to be established and agreed upon.
IASP hopes that this document will be used to enable more rapid implementation of scientific evidence than is currently happening. A further review of the situation is planned to assess the impact of IASP’s recommendations.
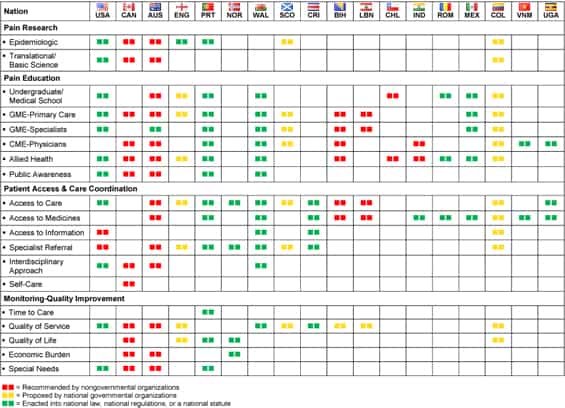
Appendix 1: Summary Chart. Examples of National Pain Care Strategies, Relevant Statements and Proposals, and Enacted Government Regulations/Laws
(click image for larger version)
Appendix 2: Survey Results: National Pain Management Assessment Survey
Purpose
To obtain information on an international scale regarding the state of pain medicine at the primary care and specialist level, and regarding obstacles to improvement in pain management through policy initiatives and government interventions.
Methods
A link to an online questionnaire was sent to 85 International Association for the Study of Pain (IASP) chapter presidents, each representing the pain medicine faculty for a particular country. The questionnaire consisted of 29 largely multiple choice questions in three areas: (1) Pain treatment by primary care providers, (2) pain treatment by specialists, and (3) the role of the government in regulating and oversight of pain management. Several open-ended questions were also asked. The respondents were encouraged to answer all questions to the best of their knowledge, although they were allowed to skip individual questions.
Results
By 12 August, 2011, 29 of 85 responses (response rate of 34%) representing 28 different countries, had been collected. The majority of respondents were from developing nations, although nations with developed health care systems, such as Canada, Australia, and the UK were also represented. The response rate per multiple-choice question ranged from 62% to 76%. The response rates below were based on respondents who actually answered the relevant question in the survey.
- With regard to primary care, the majority of respondents noted that their nation’s populace had access to primary care providers (PCPs) (67.3% of question respondents). Most PCPs were medical doctors (65% of respondents), although nurses also played a significant role (>25% of primary care in respective nations) for 1/4 of respondents. Forty-four percent of respondents indicated that less than half of PCPs in their nation did not have residency training, and 48% of respondents noted that less than 5% of PCPs had supervised clinical rotations in a pain-related medical specialty. Indeed, lack of supervised clinical training in pain for primary care was cited as one of the top three national challenges in pain management by 42% of respondents. However, pain diagnosis and management was felt to be a significant portion (>1/4) of their practice for 45% of respondents. Sixty percent of respondents noted some barrier to PCP prescription of opiates, 45% noted some restriction on the prescription of expensive adjunctive pain medications (anticonvulsants and antidepressants) by PCPs, and 70% indicated some limitation on PCPs performing pain-related procedures, such as joint injections. More than 70% of respondents indicated that PCPs in their nation were able to refer patients to an allied health provider (a physical therapist, counselor, nurse, or pharmacist) to help manage pain disorders.
- For pain specialist care: In assessing challenges to improving pain management on a national level, lack of pain specialists was cited by 100% of respondents. Ninety percent of respondents indicated that pain specialists represented 5% or less of the health care providers in their nation, with 47% of respondents indicating that 5% or less of pain specialists were MDs. Insufficient formal supervised clinical training for pain specialists was noted by 37% of those surveyed. For 69% of respondents, only 1/4 or less of the total practice of pain specialists was related to the diagnosis or treatment of pain. Nearly 40% of respondents indicated that at least 1/4 of pain specialist time was spent managing chronic pain with oral medications, while only 17% indicated that pain specialists in their nation spent more than 1/4 of their time performing procedures. A significant portion of respondents (21%) indicated that more than 1/4 of pain specialists’ practice was spent educating non-specialists. Among different types of pain (cancer-related, neuropathic, post-procedure, or other chronic pain), chronic non-neuropathic/noncancer pain was the type most commonly seen (39% of respondents indicating >1/4 of pain specialist practice). Respondents indicate that patients were more likely to be referred to a pain specialist by a PCP or other medical specialist than to be self-referred.
- Government role in pain management: Eighty-four percent of respondents indicated that the government was responsible for health care for all of its citizens. A government entity specifically tasked with pain management was noted by only 11% of respondents, while 26% indicated that their government had published referral guidelines to pain specialists, and there was no government involvement in pain specialist training and certification according to 68% of respondents. Ninety-five percent of survey respondents indicated at least moderate difficulty in contacting government legislators, administrators, and political figures regarding health care and pain management. Of 18 possible challenges for national pain management strategies, lack of government prioritization of pain management was cited by 58% of respondents.
Conclusions
Our survey of IASP chapter presidents provides a description of some of the major problems facing pain management on a global scale. The shortage of pain specialists, insufficient training for specialists and primary care providers in pain management, and the minimal role of national governments were each noted as prominent challenges in reforming pain management in their respective nations. Although our results should not be interpreted as definitive, they point to the need for greater education of health care providers and involvement of government in pain practice.
Appendix 3: Detailed Desirable Characteristics of National Pain Strategies
| Characteristics | Examples | Responsible Parties |
|---|---|---|
| Pain Education | ||
| Undergraduate | At an early stage in training to equip trainees with both the knowledge and skills to address all types of pain. The IASP core curriculum sets out standards for education in pain. | Centers of learning, regulatory bodies |
| Postgraduate | All clinicians required to have ongoing education in the relief of pain; clinicians trained to a specialist level in pain medicine. | Centers of learning, regulatory bodies |
| Public awareness | To understand pain and its management, empower consumers, and reduce the stigma of having ongoing pain, access to information on pain should be available to the general public. | Providers of health care, patient organizations, and health educator programs |
| Patient Access and Care Coordination | ||
| Care in differing settings | Rapid access to expert pain care. All hospitals should have staff with expert training in pain assessment and management to call upon. All primary care practitioners should be able to perform a basic assessment of need with regard to pain that includes determination of relief of pain and suffering. | Health care policy makers, providers and commissioners of health care |
| Medicines | The World Health Organization’s list of essential medicines should be available in preparations suitable for all ages. Support from the pharmaceutical industry will be needed to achieve this goal. | Government regulatory agencies, drug enforcement agencies, and key clinical staff |
| Informed choice | Coordination of the system so that access to the right help is available as early as possible with a fully informed choice on options. | |
| Care pathways | Care pathways agreed on by consensus are a useful way to achieve this goal. | Providers and commissioners of health care |
| Expert care | Establish pain care networks to ensure excellent relationships between providers. Where secondary care exists, there should be a vertical system for escalation of referrals of difficult problems from primary, through secondary, to tertiary care centers. | Commissioners and providers of health care |
| Interdisciplinary approach | A biopsychosocial approach to assessment and management that involves a team of health care professionals working closely together within a non-hierarchical framework. | Providers of health care |
| Family and caregiver involvement | Families and caregivers should be actively included in the management of a person in pain. | |
| Self-care | Adoption of approaches and systems that support self-care. Any pain management program must engage the community both in advocacy and in use of trained volunteers in the care program. Development of patient-led support networks. | |
| Special populations | Special populations include the very young and very old, victims of torture and natural calamities, those with learning difficulties, those with mental health and addiction disorders, ethnic minorities, and impaired persons. Their needs should be recognized and provided for. | Providers and commissioners of health care |
| Monitoring-Quality Improvement | ||
| Time to care | Standards for access times and activity planning that allow sufficient time to assess and care for people in pain. | |
| Quality of service | Improvements in patient experience should be routinely sought, including reduction in waiting times for care. | |
| Quality of life | Improvements in individual patients’ quality of life (pain relief if possible and improvement in function) using both generic and disease-specific measures. | |
| Economic burden | Monitoring should include work loss and school absence due to pain, prescription costs, urgent care, and use of other services. | |
| Outcomes | Outcomes from care should be routinely measured including patient safety, patient experience, and clinical effectiveness, drawing upon IMMPACT’s recommendations. | |
| Pain Research | ||
| Epidemiologic | A national health survey to determine population needs for pain care and monitor progress both in the general population and within institutions. | Public health services, health economists |
| Science | Prioritization of pain for funding opportunities that target gaps in pain treatment, implementation science, knowledge transfer, education, and policy development. | Federal health research funding bodies |



